Trauma to the Nail and Associated Structures
Scot D. Malay
Injuries involving the pedal nail bed and associated structures are common. Acute toenail injuries are most frequently caused by dropping a heavy object on the toe or by stubbing the toe. Other, less common mechanisms of acute injury include puncture wounds, as well as lacerations caused by lawn mower blades (1), axes, and other tools or machinery. Chronic nail trauma is usually caused by repetitive mechanical pressure associated with digital deformities and shoe gear. Delayed nail bed repair may result in less than satisfactory reconstruction, most notably nail bed scar formation and resultant onycholysis. Therefore, it is important that timely identification of the extent of the injury (2) and appropriate acute care of nail bed injuries be provided in the office, emergency department, or operating room.
NAIL ANATOMY, PHYSIOLOGY, AND FUNCTION
The perionychium consists of the paronychium (proximal nail fold, medial and lateral nail grooves), the nail matrix, and the nail bed (Fig. 1) (3). The proximal end of the nail plate rests in the proximal nail groove, with the proximal nail fold situated dorsally. The stratum corneum of the proximal nail fold forms the cuticle, which adheres to the dorsal surface of the nail plate. The nail plate consists of specialized keratin formed from germinative matrix cells located deep to the proximal nail fold and extending distally to the level corresponding to the distal margin of the lunula. The lunula is the visibly whitish-appearing semilunar area of matrix extending distal to the proximal nail fold and cuticle. The nail bed consists of epithelial cells that do not add to the ventral (plantar) surface of the nail plate but form a relatively smooth, longitudinally furrowed plateau on which the nail plate glides as it grows distally (4,5). It takes at least 5 to 6 months, and frequently as long as 9 months, to grow an entirely new toenail in a healthy adult. In general, toenails grow faster in children as compared with adults, and fingernails grow faster than do toenails. Moreover, toenails tend to grow faster in warmer environments and well-perfused digits.
The subcutaneous region deep to the nail bed is highly vascularized, and the nail bed and matrix are situated almost immediately adjacent to the periosteum of the distal phalanx. In essence, the nail bed anchors the nail plate to the distal phalanx, and at least 5 mm of healthy nail bed distal to the lunula is generally necessary for satisfactory nail plate adherence and stability (6). This is an important guideline for reconstruction of digital tip injuries that involve loss of the distal portion of the nail bed.
The plantar toe pulp consists primarily of subcutaneous tissue providing a firm, yet elastic pad for contact with the weight-bearing surface. Afferent nerves terminating in the toe conduct touch-pressure and temperature sensations, allowing proprioception and nocioception, whereas digital vascular structures (subungual glomus) permit effective peripheral temperature regulation. The resilient nail plate protects these underlying structures from injury and combines with the distal phalanx to provide a stable support against ground reactive force as the toe pulp contacts the substrate.
Nail matrix and bed damage can result in poor nail plate adherence and malalignment. Onycholysis, onychocryptosis, and a predisposition to onychomycosis, or bacterial infection, may develop following injury. Hypertrophic, dystrophic, and deformed nails with ridges, split-nail (canaliformis) changes, discoloration including streaking and loss of normal nail plate sheen, and pterygium formation (permanent adherence of the proximal nail fold ventral epithelium to the dorsal surface of the nail plate) may occur after perionychial injuries. It has been reported that distal growth of the nail plate is arrested or delayed for up to 21 days following local trauma or significant systemic stress to the individual (7). This results in the appearance of relative thickening of the nail plate proximal and distal to the visibly thinner transverse line of diminished nail plate production. Proximally, the newly formed nail plate is actually thicker than the normally formed, distal segment of the plate. The proximal thickening results from an approximately 50-day period of increased matrix activity without distal elongation of the
plate. Toward the end (last 30 days) of the period of increased matrix activity, distal progression of the nail plate occurs. Following the period of increased nail plate production, there is an approximately 30-day period of decreased activity before normal matrix activity resumes. Therefore, approximately 100 days of abnormal nail plate production can be expected following trauma. The nail plate will typically reveal a transverse groove, or Beau’s line, after such an injury (Fig. 2).
plate. Toward the end (last 30 days) of the period of increased matrix activity, distal progression of the nail plate occurs. Following the period of increased nail plate production, there is an approximately 30-day period of decreased activity before normal matrix activity resumes. Therefore, approximately 100 days of abnormal nail plate production can be expected following trauma. The nail plate will typically reveal a transverse groove, or Beau’s line, after such an injury (Fig. 2).
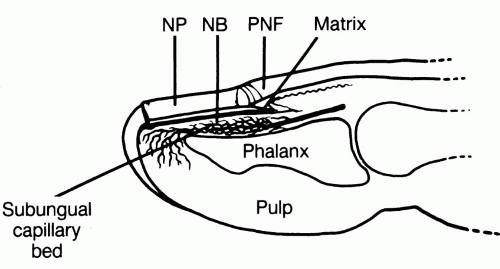 FIG. 1. Nail anatomy and associated structures. NB, nail bed; NP, nail plate; PNF, proximal nail fold. |
The nail plate and perionychium are subject to a variety of injuries ranging from minor contusions to trauma causing severe tissue loss and the need for either acute or delayed surgical reconstruction. The hierarchy of nail bed injuries, ranging from least extensive to most extensive, includes primary (idiopathic) onycholysis, subungual hematoma, simple nail bed lacerations, complex (crushing or stellate) nail bed lacerations, nail bed lacerations with distal phalangeal fracture, and a variety of nail bed and toe tip tissue loss (avulsion, amputation, and degloving) injuries. Patients with such injuries may seek medical attention at the hospital emergency room or the local podiatrist’s office. Accurate initial diagnosis of the extent of injury and proper initial treatment will greatly enhance the chance that posttraumatic sequelae will be minimized (8). A useful guideline to remember for the acute care of the traumatized nail is to preserve the unity of the toe tip: nail plate, nail bed and matrix, proximal and medial and lateral nail folds, distal phalanx, and the toe pulp.
MECHANICAL ONYCHOLYSIS
Mechanical onycholysis, or minor separation of the nail plate from the underlying bed due to repetitive friction and pressure, is not, in any way, considered an emergency situation. However, a distinction between chronic mechanical nail injury and pathogenic onychomycosis should be made so that appropriate therapy can be rendered (9). Separation of the nail plate from the underlying nail bed effects a change in the nail plate’s refractive index to light, and the area of separation appears as a small white blotch in the nail plate. Mechanically induced separation of the distal margin or edges of the nail plate from the nail bed often occurs in conjunction with hammer toes and other digital contractures, or digital pressure caused by tight-fitting shoes, and frequently affects the hallux or longest toe. The area of nail plate separation may become secondarily infected with dermatophytes, yeast, or bacteria. Associated subungual hematoma may also occur, especially in athletes (turf toe). Treatment is aimed at alleviating the cause of the repetitive mechanical trauma and providing appropriate antimicrobial therapy, if necessary.
SUBUNGUAL HEMATOMA
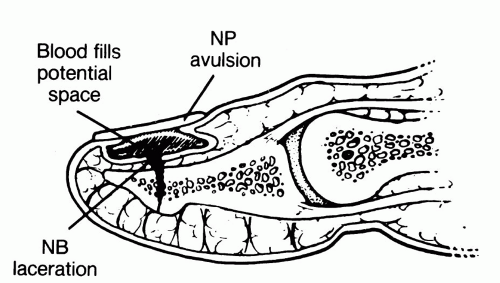
A potential space exists between the nail plate and the underlying nail bed and matrix (Fig. 3). Onycholysis results in the creation of a space between the plate and bed, which may or may not fill with blood. Acute injuries that create visible onycholysis greater than 1 mm2 usually result in subungual hematoma. When a patient is seen with a swollen toe and reports throbbing pain shortly after sustaining a digital injury, nail bed damage and subungual hematoma should be suspected. Subungual pressure secondary to hemorrhage can damage cells of the matrix and nail bed, especially if it is not relieved within 6 to 12 hours after the initial trauma. Hemorrhagic nail plate discoloration, which appears reddish blue initially and brownish black after 5 to 7 days, confirms
the diagnosis of a disrupted nail bed. Unless subungual hematoma is suspected, it may be overlooked in the presence of a thick, discolored, or mycotic nail plate, because the hematoma can be hidden by the overlying dystrophic nail plate. Moreover, radiographs of the digit should be considered during the initial evaluation of a subungual hematoma because approximately 19% to 25% of these lesions are associated with an underlying phalangeal fracture (2,10).
the diagnosis of a disrupted nail bed. Unless subungual hematoma is suspected, it may be overlooked in the presence of a thick, discolored, or mycotic nail plate, because the hematoma can be hidden by the overlying dystrophic nail plate. Moreover, radiographs of the digit should be considered during the initial evaluation of a subungual hematoma because approximately 19% to 25% of these lesions are associated with an underlying phalangeal fracture (2,10).
 FIG. 4. Crush injury, with 100% subungual hematoma. Note the dissecting hematoma separating the proximal nail fold epidermis from the underlying dermis. |
Treatment of subungual hematoma involves draining the blood to reduce subungual pressure. If the hematoma involves an area less than 25% of the visible nail plate, drainage can be obtained through the nail plate with the use of a hand cautery unit, an 18-gauge needle, a No. 11 blade scalpel, a heated paper clip, or the podiatry drill with an appropriate small ball bur (3,10). The status of the patient’s tetanus prophylaxis should be ascertained and the nail plate cleansed before penetrating it. Consideration should also be given to the use of appropriate antibiotic prophylaxis or therapy, when indicated. Once the plate is penetrated, blood is expressed and subungual pressure alleviated. A water-soluble antiseptic solution or antibiotic cream and a dry sterile dressing with appropriate splinting are then applied, and the patient is reevaluated in 1 to 2 weeks. If the subungual hematoma involves more than 25% of the visible nail plate or the nail plate has been avulsed in such a way as to disrupt the proximal, medial, or lateral nail folds, then a significant nail bed laceration should be suspected and direct visualization and surgical repair of the nail bed is recommended (Fig. 4) (3,11).
NAIL BED LACERATIONS
Simple Nail Bed Laceration
When a significant nail bed laceration is suspected, the nail plate is avulsed following digital block and a surgical scrub and draping. Tetanus prophylaxis and appropriate antibiotics are initiated. If indicated, a Penrose or another type of digital tourniquet may be used for hemostasis at the base of the toe. If the toe is too edematous for further fluid injection, a more proximal regional block (Mayo block) is employed and the digital tourniquet is not used.
Once the nail plate has been removed, dilute povidoneiodine irrigation is used to flush away hematoma and debris, and the nail bed is inspected (Fig. 5). Because of the friable nature of the tissue, nail bed débridement is kept to a minimum. The margins of the laceration are then meticulously reapproximated with the use of a 5-0 or 6-0 absorbable suture on an atraumatic needle in a simple interrupted fashion. Suturing can be difficult because the nail bed is very friable and intimately adherent to the periosteum of the underlying phalanx. Although superglue (octylcyanoacrylate) has been used successfully in the repair of other friable tissues (12, 13, 14), the author has encountered robust scar hypertrophy and resultant onycholysis in the single case in which this technique was used for a transverse nail bed laceration without fracture. Lacerations of the proximal and lateral nail folds are repaired with 4-0 or 5-0 suture. Nonabsorbable suture on a reverse cutting needle has worked well. Care must be taken to avoid driving the needle through the germinative nail matrix. Primary repair of the nail bed can be attempted up to 7 days following laceration, after which time wound contraction and granulation are typically too advanced for accurate nail bed reapproximation (3).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree