Distal Humerus
EPIDEMIOLOGY
This is a relatively uncommon injury, comprising approximately 2% of all fractures and one-third of all humerus fractures.
Incidence of distal humerus fractures in adults is 5.7 per 100,000 per year.
Distal humerus fractures have a bimodal age distribution, with peak incidences occurring between the ages of 12 and 19 years in men and 80 years and older in women.
Greater than 60% of distal humerus fractures in the elderly occur from low-energy injuries, such as a fall from standing height.
Extra-articular fractures (40%) and bicondylar intra-articular fractures of the distal humerus (37%) are the most common fracture patterns.
Extension-type supracondylar fractures of the distal humerus account for >80% of all supracondylar fractures in children.
ANATOMY
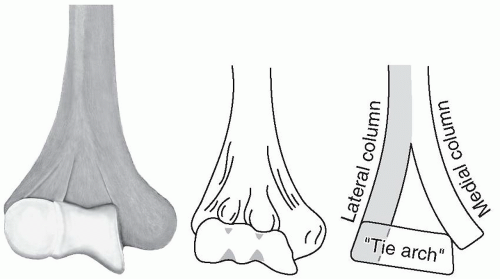
Distal humerus may be conceptualized as medial and lateral “columns,” each of which is roughly triangular in shape and composed of an epicondyle, or the nonarticulating terminal of the supracondylar ridge, and a condyle, which is the articulating unit of the distal humerus (Fig. 17.1).
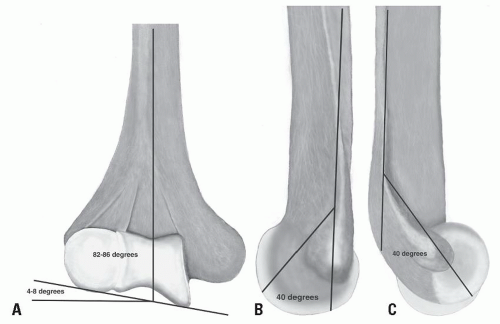
Articulating surface of the capitellum and trochlea projects distal and anterior at a 40- to 45-degree angle. The center of the arc of rotation of each condyle’s articular surface lies on the same horizontal axis; thus, malalignment of the relationships of the condyles to each other changes their arc of rotation, thus limiting flexion and extension (Fig. 17.2).
The trochlear axis compared with the longitudinal axis of the humerus is 4 to 8 degrees of valgus.
The trochlear axis is 3 to 8 degrees internally rotated.
The intramedullary canal of the humerus ends 2 to 3 cm above the olecranon fossa.
MECHANISM OF INJURY
Most low-energy distal humeral fractures result from a simple fall in middle-aged and elderly women in which the elbow is either struck directly or is axially loaded in a fall onto the outstretched hand.
Motor vehicle and sporting accidents are more common causes of injury in younger individuals.
CLINICAL EVALUATION
Signs and symptoms vary with degree of swelling and displacement; considerable swelling frequently occurs, rendering landmarks difficult to palpate. However, the normal relationship of the olecranon, medial, and lateral condyles should be maintained, roughly delineating an equilateral triangle.
Crepitus with range of motion and gross instability may be present; although this is highly suggestive of fracture, no attempt should be made to elicit it because neurovascular compromise may result.
A careful neurovascular evaluation is essential because the sharp, fractured end of the proximal fragment may impale or contuse the brachial artery, median nerve, or radial nerve.
Serial neurovascular examinations with compartment pressure monitoring may be necessary with massive swelling; cubital fossa swelling may result in vascular impairment or the development of a volar compartment syndrome resulting in Volkmann ischemia.
RADIOGRAPHIC EVALUATION
Standard anteroposterior (AP) and lateral views of the elbow should be obtained. Oblique radiographs may be helpful for further fracture definition.
Traction radiographs may better delineate the fracture pattern and may be useful for preoperative planning.
In nondisplaced fractures, an anterior or posterior “fat pad sign” may be present on the lateral radiograph, representing displacement of the adipose layer overlying the joint capsule in the presence of effusion or hemarthrosis.
Minimally displaced fractures may result in a decrease in the normal condylar shaft angle of 40 degrees seen on the lateral radiograph.
Because intercondylar fractures are almost as common as supracondylar fractures in adults, the AP (or oblique) radiograph should be scrutinized for evidence of a vertical split in the intercondylar region of the distal humerus.
Computed tomography is often used to delineate the fracture pattern, amount of comminution, and intra-articular extension.
CLASSIFICATION
Descriptive
Supracondylar fractures
Extension type
Flexion type
Transcondylar fractures
Intercondylar fractures
Condylar fractures
Capitellum fractures
Trochlea fractures
Lateral epicondylar fractures
Medial epicondylar fractures
Fractures of the supracondylar process
Orthopaedic Trauma Association Classification of Fractures of the Distal Humerus
See Fracture and Dislocation Compendium at http://ota.org/compendium/index.htm.
GENERAL TREATMENT PRINCIPLES
Anatomic articular reduction
Stable internal fixation of the articular surface
Restoration of articular axial alignment
Stable internal fixation of the articular segment to the metaphysis and diaphysis
Early range of elbow motion
SPECIFIC FRACTURE TYPES
Extra-Articular Supracondylar Fracture
This results from a fall onto an outstretched hand with or without an abduction or adduction force.
The majority are extension patterns with a minority being flexion types.
Treatment
Nonoperative
This is reserved for nondisplaced or minimally displaced fractures, as well as for severely comminuted fractures in elderly patients with limited functional ability.
A posterior long arm splint is placed in at least 90 degrees of elbow flexion if swelling and neurovascular status permit, with the forearm in neutral.
Posterior splint immobilization is continued for 1 to 2 weeks, after which range-of-motion exercises are initiated in a hinged brace. The splint or brace may be discontinued after approximately 6 weeks, when radiographic evidence of healing is present.
Frequent radiographic evaluation is necessary to detect loss of fracture reduction.
Operative
Indications
Displaced fractures
Vascular injury
Open fracture
Inability to maintain acceptable reduction
Patient positioning
Supine on a radiolucent table with arm over chest
Quick and easy setup
Good for multiply injured patients with multiple extremity involvement
Requires assistant to hold arm during procedure
Lateral
Allows good access to posterior arm and elbow without need for additional assistant
Prone
Allows good access to posterior arm and elbow without need for additional assistant
Image positioning
Image intensifier can be placed on same or opposite side of the injured extremity
Surgical approaches:
Triceps splitting approach
Easy to perform
Enables intact trochlear notch of proximal ulna to act as template to assist fracture reduction
No need for additional hardware to reattach olecranon
Can be converted to exposure necessary for total elbow replacement or olecranon osteotomy for increased articular exposure
Affords limited articular exposure—usually used for extra-articular fractures
Paratricipital approach
Easy to perform
Uses windows on either side of the triceps to assess fracture reduction
Can be converted to exposure necessary for total elbow replacement or olecranon osteotomy for increased articular exposure
Has limited articular exposure compared to olecranon osteotomy
Usually used for extra-articular fractures or if chance of conversion to elbow arthroplasty during surgery
Triceps reflecting anconeus pedicle (TRAP) approach
Uses a proximally based triceps-anconeus flap
Medial portion of flap is created by subperiosteal dissection from the subcutaneous border of the ulna
Kocher interval is used to raise the anconeus muscle and develop the lateral portion of the flap
Anconeus flap elevated and reflected proximally to expose the triceps insertion, which is also released
Advantage is preservation of the neurovascular supply to the anconeus
Soft tissue repair required to reattach the extensor mechanism
Bryan-Morrey approach
Involves subperiosteal reflection of the triceps insertion from medial to lateral in continuity with the forearm fascia and anconeus muscle
Although the triceps tendon insertion is detached, the extensor mechanism maintains its continuity as a single sleeve through its soft tissue attachments
Extensor sleeve is repaired using drill holes or osseous anchors
Used primarily for arthroplasty
Van Gorder approach (triceps tongue)
Transection of triceps at musculotendinous junction (V-Y incision)
Used for arthroplasty or fractures with complete/high-grade triceps tendon laceration
Olecranon osteotomy
Most extensile approach
Uses a transverse or apex distal, chevron-type osteotomy of the olecranon which exits in the so-called bare area of the trochlear groove
Osteotomy is initiated with an oscillating saw and completed with an osteotome
Osteotomy requires fixation using a tension band construct, an intramedullary screw/nail, or a plate.
Implant options
Plate fixation
Plate fixation is used on each column, either in parallel or 90 degrees from one another.
Use of locked plates has gained in popularity and affords much better metaphyseal fixation than conventional nonlocked plates.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree