CHAPTER 56 Distal Humeral Fractures–Acute Total Elbow Arthroplasty
INTRODUCTION
Distal humeral fractures are infrequent when compared with other fractures and comprise approximately 1% to 2% of all adult fractures and 10% of humeral fractures.27,29,33 The population distribution of such fractures tends to be bimodal, with a peak in the second and third decades, and with a second peak in the sixth to eighth decades.13
NONSURGICAL MANAGEMENT
Nonoperative options of soft sling or plaster cast are traditionally used in cases in which reconstruction is not an option, by virtue of patient or surgical factors. Although widely propagated as an acceptable methodology, it is documented that such a strategy does not yield consistent pain relief or consistent joint stability, with unsatisfactory results in approximately 40% of cases.17
FRACTURE FIXATION
A prerequisite for reconstruction is to fix the fracture fragments with some form of rigid fixation construct that then synchronously allows stable fixation and joint motion. However, there are three main fracture factors that adversely affect the ability to reconstruct the distal humeral fracture: (1) Comminution: If the distal humeral articular surface is significantly comminuted (Fig. 56-1A), not only is it not possible to fix all the bony fragments, but the cartilage surface would also have undergone considerable injury, leading to a suboptimal bearing surface. (2) Size of fracture fragments: It is straightforward to understand the issues with a large number of small bony fragments, with a significant number made up of small osteochondral fragments. Additionally a transcondylar or very low supracondylar fracture also poses the same problem of the ability to hold the fracture sufficiently rigidly while allowing joint motion (see Fig. 56-1B). (3) Quality of bone stock: Good quality young bone stock allows better fixation than does osteopenic/osteoporotic older bone.26,31 In a young population with an average age of 35 years, distal humeral articular surface fractures treated with internal fixation achieved good and sustainable results, although 40% required secondary procedures: an average flexion arc of 106 degrees, average foream rotational arc of 165 degrees, and a Mayo Elbow Performance Score (MEPS) of 91.2 A choronologically older group of patients with distal humeral fracture fixation, but without objective proof of osteoporosis, resulted in a 75% good/excellent range of motion and 80% satisfaction,15 although other studies of the older age group found less satisfactory results.27 Helfet et al8 demonstrated that despite good surgical technique and adequate internal fixation, 2-10% of such patients develop non-unions. Furthermore, if early motion is sacrificed, a compromise made for the quality of bone stock, the prediction is a better rate of union with a stiff joint. Pajarinen and Bjorkenheim26 correlated that immobilization greater than 3 weeks was a poor prognostic factor, after open reduction and internal fixation (ORIF), for achieving a good functional score. Thereby, when the principle of rigid internal fixation with early joint mobilization cannot be adhered to, then fracture fixation, joint immobilization to union, and a secondary motion gaining procedure may have to be considered.
ACUTE TOTAL ELBOW ARTHROPLASTY
An alternative strategy that has gained a wider acceptance is the acute total elbow replacement, when the fracture is judged to be unreconstructable or reconstructable without the predictability desired to allow early motion. However, the replacement of an unreconstructable fracture involving a joint is not a new concept. Hip7 and shoulder,6,25 and less commonly knee,7,14 surgeons, have an established body of literature regarding the relevance and successful outcomes of this concept.
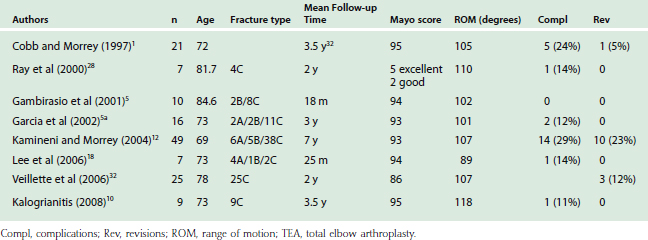
Total elbow replacements have been proven effective in the treatment of distal humeral nonunions,22 post-traumatic arthritis,16,24,30 rheumatoid arthritis,23 and chronic fracture dislocations.20 More recently, a growing literature appears to be favorable regarding this concept in the treatment of the difficult-to-reconstruct distal humeral fracture in the older age group of patients (Table 56-1). The first large series, which was reported by Cobb and Morrey,1 was a retrospective study of 21 distal humeral fractures in patients with an average age of 72 years. Ten of the cases had pre-existing rheumatoid arthritis, and the follow-up period was an average of 3.3 years (Table 56-2). The outcomes, based on the MEPS, were 15 excellent and five good results, with inadequate data in one case. Only one patient required revision arthroplasty due to a fractured ulna component (Table 56-3).
TABLE 56-1 Indications and Contraindications for Acute Elbow Arthroplasty
TABLE 56-3 Complications Associated with Acute Elbow Arthroplasty
This study was extended by Kamineni et al12 to 43 patients, and re-reported with a seven year follow-up. Nineteen patients in this cohort had pre-existing rheumatoid arthritis. The average flexion arc was 107 degrees, with an average MEPS of 13/100. Five patients required revision arthroplasty due to trauma (n = 3), aseptic loosening (n = 1), and septic loosening (n = 1). This latter study demonstrated that the results were maintained over a longer follow-up period, although the revision rate increased with time, from 5% at 3 years to 12% at 7 years.
Ray et al28 reported on seven patients with a mean age of 81 years who underwent acute total elbow arthroplasty without underlying pathology. The functional outcomes were excellent in five and good in two patients, with an average flexion arc greater than 100 degrees. Only one patient had mild pain, with the other six patients being completely pain free.
The use of unlinked prosthesis for an acute arthroplasty was reported in only one series, which focused on a group of patients with an average age of 73 years and a follow-up of 3.5 years.11 The MEPS was 95, and the average arc of flexion was 98 degrees. This helps to corroborate the concept of acute arthroplasty for fractures, independent of the choice of linked or unlinked prostheses.
When distal humeral fractures are associated with underlying rheumatoid or other inflammatory arthritides, the indications for an acute arthroplasty are more relaxed.1,11,12,28 Furthermore, fractures in the rheumatoid population should be considered a different pathology than that of a fracture in a joint that was nonpathologic before injury.1,12,28 The generally good results that can be expected in the fractured rheumatoid population was reported by Ikavalko and Lehto.10 A 100-degree arc of flexion was maintained up to a 4-year period. However, due to the low demands of this population, complications can be dealt with much more conservatively than the non-rheumatoid patient.
Whereas the indications for acute elbow joint replacement are being extended, as is expected of any new procedure, caution must be exercised when making the decision between conservative, osteosynthesis, and arthroplasty management. The importance of a correct and timely decision is highlighted by the functional outcomes of a successful osteosynthesis versus an acute arthroplasty, as opposed to a later conversion of a failed osteosynthesis to a secondary arthroplasty. Frankle et al have reported a retrospective comparison of value.4 Patients older than 65 years with C2 or C3 intra-articular distal humeral fractures were treated with either osteosynthesis or acute elbow arthroplasty. In the osteosynthesis group, there were one fair and three poor MEPS outcomes, whereas in the arthroplasty group, only excellent and good results were achieved at a 2-year follow-up. Veillette and McKee32 corroborated these findings with a multicenter prospective randomized study comparing osteosynthesis with acute elbow arthroplasty in patients older than 65 years. The MEPS revealed a significant improvement with acute arthroplasty (total elbow arthroplasty [TEA] 86 versus ORIF 73) over a 2-year follow-up. However, the Disabilities of the Arm, Shoulder and Hand (DASH) questionnaire showed a significantly better outcome for acute arthroplasty in the first 6 months, but at a longer 2-year follow-up, the results between the two groups showed no statistical difference. However, a finding of note was that the arthroplasty group had a lower reoperation rate (12% versus 26%).
When the decision to perform an osteosynthesis is incorrect at the time of injury and the fixation fails, requiring a secondary arthroplasty, the results are generally poorer than if the primary intervention was an acute elbow arthroplasty. Mighell et al21 reported 28 cases of failed osteosynthesis converted to total elbow arthroplasty in patients with an average age of 66 years. At a 3-year follow-up, the improvement in functional outcomes (American Shoulder and Elbow Surgeons [ASES] scores) were statistically significant from 36 to 65, with improvements in pain, motion and function. These results could be interpreted as lesser to those results for a primary acute arthroplasty. In addition, 21% (6/28) required revision implant surgery, five patients required revision arthroplasty for aseptic loosening, and one required ultimate arthrodesis for septic loosening. Hence, the wrong decision at the primary intervention appears to result in a lesser functional outcome and a higher complication and revision rate.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree