Chapter 80 Distal Femur Fractures
Anatomy
General Anatomy
The distal femur extends for approximately the distal third of the femur.23,28,70 It begins as the canal gradually widens and the cortices thin and continues distally to the joint line. The supracondylar region (distal metaphysis) flares medially greater than laterally in the coronal plane and broadens laterally greater than medially in the sagittal plane. The anterior and distal trochlear groove allows patellar articulation with the distal end of the femur. The intercondylar notch is posteriorly based and houses the cruciate ligaments.
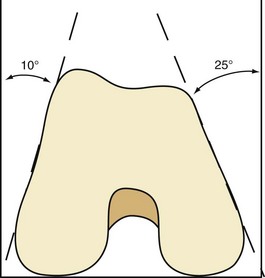
An axial cut through the distal articular surface reveals a trapezoidal shape with the greatest dimension located posteriorly in a lateral-to-medial direction and the narrowest dimension located medially in an anterior-to-posterior direction. The medial side slopes approximately 25 degrees in a posteromedial-to-anterolateral direction. The lateral side slopes approximately 15 degrees in a posterolateral-to-anteromedial direction (Fig. 80-1).54 The shaft lies in the anterior two thirds of the condyles in the sagittal plane and slightly lateral, with a 9-degree valgus orientation in the coronal plane.28,54,61,87
Radiographic Anatomy
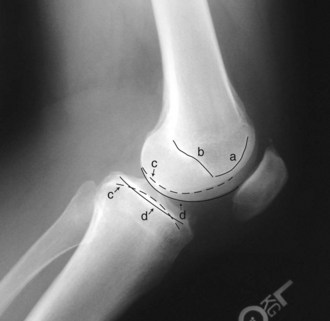
The anteroposterior (AP) radiograph demonstrates the 9-degree valgus angle created between the femoral shaft and the distal joint line. It also shows the greater medial condyle flare but does not reveal the trapezoidal shape as seen on an axial computed tomography (CT) image. The lateral radiograph demonstrates an anterior curvilinear sclerotic line representing the trochlear groove and a convergent posterior sclerotic line representing the intercondylar notch (Blumensaat’s line), both of which end as they meet distally (Fig. 80-2). In addition, a true lateral radiograph of the knee allows identification of the medial femoral condyle as it articulates with the concave medial tibial plateau, and the lateral femoral condyle as it articulates with the convex lateral tibial plateau (see Fig. 80-2). Flexion of the knee during the AP radiograph allows visualization of the intercondylar notch.
Incidence and Etiology
The incidence of supracondylar femoral fractures has a bimodal distribution—young adult patients with higher-energy injuries and elderly patients with lower-energy injuries.3,23,38 The supracondylar femoral fracture is typically the result of an external force, but the amount of force required to cause the fracture can vary significantly and is dependent on bone quality. In a 2000 report on 2165 distal femoral fractures, the distribution of such fractures was found to be bimodal, occurring in young men and elderly women.47 Lower-energy injuries are generally the result of ground-level falls or torsional injuries in patients with osteopenic or osteoporotic bone. Periprosthetic fractures are usually low-energy injuries that are encountered most commonly in the elderly as a result of disuse osteopenia, osteoporosis, and/or stress shielding around a prosthetic device or other metallic implant. A stress riser is created in the transition area between the prosthesis and routine bone. Examples include the area distal to a hip stem, proximal to a short supracondylar nail, and proximal to a total knee prosthesis.
The amount of energy required to cause a supracondylar or distal femoral fracture in young patients with no existing bone pathology is usually significant, and this fracture is often seen in conjunction with other associated fractures.4,6,8,14,81 Knee ligament injuries and intra-articular pathology have been reported in approximately 20% to 70% of ipsilateral femoral fractures.6,14,81 Motor vehicle or motorcycle accidents, falls from heights, pedestrian versus auto accidents, and other heavy industrial accidents are common mechanisms of injury.47
Classification
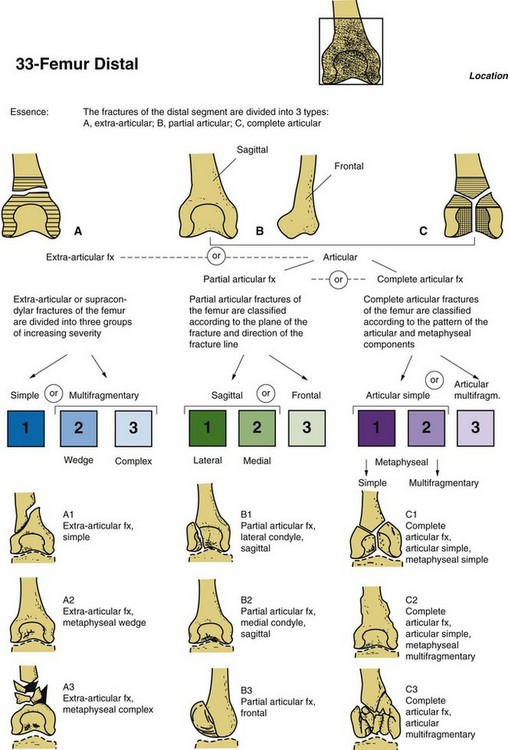
A number of classification systems have been proposed for fractures of the distal femur. In 1967, Neer and associates described a classification system that divided fractures into three main categories: minimal displacement, condylar displacement from the shaft, and supracondylar or shaft comminution.57 Seinsheimer later published a more detailed system.70 The Swiss Arbeitsgemeinschaft für Osteosynthesefragen/Association for the Study of Internal Fixation (AO/ASIF) group has since developed a comprehensive fracture classification scheme that has become accepted in the trauma community: type A, extra-articular; type B, unicondylar; and type C, bicondylar (Fig. 80-3). This classification is further subdivided by the degree of comminution.56 The Orthopaedic Trauma Association (OTA) has developed a similar detailed and well-accepted classification system that encompasses the entire axial skeleton.19
Diagnosis
History and Physical Examination
As with any traumatized patient, a complete history and detailed physical examination should be conducted. The preinjury level of function and additional medical conditions should be recorded because such knowledge will aid in determining whether conservative or operative treatment should be performed. The mechanism of injury must also be ascertained to help determine the severity of the injury and other associated injuries. The physical examination should include a detailed evaluation of the entire limb and other extremities to rule out ipsilateral and associated fractures.8 The skin must be circumferentially inspected for open wounds, and a detailed neurologic and vascular examination of the entire extremity should be documented. Higher-energy injuries can result in laceration or rupture of the quadriceps tendon, the femoral artery as it exits the adductor hiatus, the popliteal artery, and knee ligaments.4,6,81 The knee joint itself should be evaluated for an effusion because an effusion often represents a radiographically unnoticed intercondylar split, an associated tibial plateau or patellar fracture, and/or anterior or posterior cruciate ligament rupture.
In higher-energy fractures, the ankle-brachial index should be documented even if palpable pulses are present. A ratio less than 0.9 has been shown to correlate with a high incidence of arterial injury, whereas ratios greater than 0.9 show that vascular intervention was not required. If abnormal, angiography and vascular surgery consultation should be performed.37,51
Radiographic Examination
As with any fracture, orthogonal views (AP and lateral) are indicated. Both knee and femur radiographs are necessary to fully evaluate the fracture and the entire femoral shaft. A traction radiograph may be helpful to better delineate all fracture fragments. Knee views will better diagnose intra-articular extension or comminution and associated patellar or tibial plateau fractures. Coronal condylar fractures (the so-called Hoffa fragment) seen in the lateral view must not be missed because the presence of such coronal splits will influence the selection of fixation devices.4,30 Femoral shaft radiographs will reveal the proximal extent of the fracture, segmental fracture patterns, or possibly ipsilateral femoral neck fractures. If femoral neck involvement is at all suspected, dedicated hip radiographs must be obtained, because intraoperative discovery of this associated fracture can lead to different instrumentation and patient positioning. CT is indicated for comminuted fractures, or if absolute certainty of all fracture lines cannot be gained from plain radiographs. Once all fracture planes are determined, more optimal fixation can be applied. The authors routinely obtain CT scans when planning definitive internal fixation.
Management
Alternative Exposures
Anterior
The anterior approach requires a midline incision and a parapatellar arthrotomy. It allows excellent joint exposure but also requires separation of the vastus intermedius as the approach is extended proximally from the knee joint. A variation of the anterior approach described as the “swashbuckler” also allows for excellent joint exposure and is basically a lateral approach with an anteriorly placed incision.75 Other variations of the aforementioned standard approaches have also been described.52,58
Implants—Design and Function
Numerous implants have been described and designed for supracondylar and distal femoral fractures. Implant types include short and long retrograde nails, various fixed-angled devices, and standard compression and buttress plates. Specific examples include Zickel, GSH, and standard retrograde nails; the AO angled blade plate; the dynamic condylar screw; the condylar buttress plate; and, more recently, locked plates.*
Additional fixed-angle devices have become available in the form of anatomically designed plates with locking screw technology that can be inserted through a traditional open approach or percutaneously.17,41 The locking plate design also creates a 95-degree angle between the distal screws and the plate. Proper insertion is achieved with the distal screws parallel to the joint line; this is followed by reduction of the femoral shaft to the plate.20,65 The advantage of locked plates over the traditional angled blade plate is seen with intercondylar split fractures. Insertion of an angled blade generates significantly more force than is generated by insertion of a threaded locked screw, and can therefore displace an undisplaced or previously reduced and compressed intercondylar split. In addition, rotational freedom during insertion is present with locked plates, as with the condylar screw, and the advantage of a fixed-angle device is gained. Newer anatomically designed locking plates may also allow for variable-angle locked screws that are inserted at the surgeon’s preferred angle and then locked to the plate once fully seated.86
In cases of extreme osteopenia, osteoporosis, tumor, or other conditions with poor bone quality, a second medial implant has been described to add to construct stability.26,35,48,49,64 The addition of bone cement has been advocated in similar situations to achieve increased screw purchase.5,77 With the advent of modern locking plate technology, the need for adjunctive medial fixation or cement augmentation has essentially been eliminated.
The choice of implant is dependent on the location of the fracture, the fracture pattern, existing hardware, bone quality, and surgeon preference. It must also be stated that great care must be instituted when using locking plate technology as there is early evidence that these constructs may actually be too rigid, thereby increasing the risk of nonunion if not used properly.8
Treatment
Initially, as with all fractures, splinting and immobilization were favored over internal fixation. In the 1940s and 1950s, internal fixation was reported, but without overwhelming success.1,79,85 As technology advanced and techniques improved, success rates with internal fixation began to increase. The Swiss AO group in 1958 defined the goals of open reduction and internal fixation as follows: (1) anatomic reduction, (2) preservation of the blood supply, (3) stable internal fixation, and (4) early mobilization.55 Schatzker and Wenzl began documenting improved results with the AO principles and showed open reduction and internal fixation to be superior to conservative management.66–6884 Other authors soon reported similar findings.* Today, although slightly modified, the AO principles are still being used, and the results of surgical treatment remain superior to those of nonoperative management for displaced fractures.
Conservative Treatment
Conservative management of distal femoral and supracondylar fractures has fallen out of favor as surgical techniques, implant designs, and rehabilitation protocols have continued to progress and yield outcomes superior to those of nonoperative treatment.† Certain situations, however, still require nonoperative management; it is therefore necessary to remain familiar with conservative treatment options.
For patients with low-energy, extra-articular, nondisplaced fractures who refuse or cannot medically tolerate a surgical procedure, cast bracing or casting is recommended. Non–weight bearing must be enforced until adequate healing is achieved to avoid creating a deformity or unstable fracture. Knee joint stiffness typically becomes problematic with longer than 6 weeks of immobilization.21
Operative Management
High-energy injuries involving the distal femur are frequently comminuted and have significant intra-articular involvement (Fig. 80-4A through D). If the fracture is an open fracture, adequate initial débridement must be performed, followed by thorough irrigation and temporary or definitive stabilization. If temporary stabilization is chosen, a spanning external fixator can be used, with the pins for the fixator placed away from the region of future definitive fixation. Two pins are typically inserted anteriorly or laterally into the femur, and two pins into the proximal end of the tibia, with the frame then spanning the knee joint (Fig. 80-5). If the soft tissues appear stable and appropriate studies and implants are available, definitive fixation may be performed at the time of initial débridement. When significant intra-articular comminution warrants a CT scan, a staged approach must be adopted if the CT scan is not available prior to the initial open fracture débridement. The distal femur has better soft tissue coverage than the tibia, so plate application can be safely performed acutely unless significant soft tissue loss and/or excessive gross contamination is present. If tissue transfer is required for bone or plate coverage, or for both, initial spanning external fixation would be more appropriate. Intravenous antibiotic coverage based on the type and degree of soft tissue wounds is necessary, as in all long-bone open fractures. Initial bone grafting of open fractures is not recommended because of the increased risk of infection, although the literature mostly pertains to open tibia rather than open femur fractures. Intraoperative techniques that can assist in achieving adequate length or fracture reduction include manual traction, application of the AO femoral distractor, and use of the AO articulating tensioning device.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree