Laurie Ruth Chaikin, MS, OTR/L, OD, FCOVD After reading this chapter the student or therapist will be able to: 1. Identify and analyze visual anatomy and physiology as they pertain to visual function. 2. Analyze the functional visual skills and how visual dysfunction may affect functional performance. 3. Identify the symptoms of visual dysfunction. 4. Develop the skill necessary to take a visual case history by use of behaviors and clinical observations. 5. Identify the difference between phoria and strabismus. 6. Identify and evaluate the difference between visual field loss and unilateral neglect. 7. Identify and differentiate various pediatric and age-related disease conditions that may affect vision. 8. Clearly differentiate nonoptical and optical assessment and intervention adaptations for patients with low vision. 9. Differentiate basic tools for vision screening. 10. Identify when and why to refer and the tools necessary to document that decision. Vision is an integral part of development of perception. Some aspects of vision, such as pupillary function, are innate, but many other aspects are stimulated to develop by experience and interaction with the environment. Visual acuity itself has been demonstrated to rely on the presence of a clear image focused on the retina. If this does not occur, a “lazy eye,” or amblyopia, will result. Depth perception develops as a result of precise eye alignment. This ability will be delayed, less precise, or absent if correction of eye misalignment is not done within the first 7 years of life. Research has demonstrated that, in fact, most visual skills such as acuity, binocular coordination, accommodation, ocular motilities, and depth perception are largely intact by age 6 months to 1 year.1 Visual skill development parallels postural reflex integration and provides a foundation for perception. Structures and function are discussed from anterior to posterior (Figure 28-1). The first structure that light hits after it is reflected from an image is the cornea. (Technically, light first hits the tear layer, which has its own structure and rests on the corneal surface.) Corneal tissue is completely transparent. Light is refracted, or bent, to the greatest degree by the cornea because the light rays must pass through different media, which change in density, as in going from air to water.2 The refraction of light can be observed by noting how a stick placed into water appears bent where it enters the water (Figure 28-2). Damage to the cornea from abrasions, burns, or congenital or disease-related processes can alter the spherical shape of the cornea and disturb the quality of the image that falls on the retina. Radial keratotomy, a surgical procedure done in the 1980s to reduce nearsightedness by placing spokelike cuts in the cornea, sometimes had the side effect of scarring the cornea and causing distorted vision. This surgery is no longer done. The newer surgeries such as laser-assisted in situ keratomileusis (LASIK) are far superior and more predictable in their reduction of refractive error (nearsightedness, farsightedness, or astigmatism) and induce virtually no scarring or distortion. In keratoconus the cornea slowly becomes steeper and more cone shaped, distorting the image and causing reduced vision.3 Behind the cornea is the iris, or colored portion, which consists of fibers that control the opening of the pupil, the dark circular opening in the center of the eye. The constriction and dilation of the pupil control the amount of light entering the eye in a similar fashion to the way the f-stop on a camera changes the size of the aperture to control the amount of light and the depth of field.4 Under bright light conditions the opening constricts, and under dim light conditions it dilates, allowing light in to stimulate the photoreceptor cells of the retina. This constriction and dilation are under autonomic nervous system (ANS) control, with both sympathetic and parasympathetic components.5 Under conditions of sympathetic stimulation (fight or flight) the pupils dilate, perhaps giving rise to the expression “eyes wide with fear.” Under parasympathetic stimulation the pupils constrict. The effect of drugs that stimulate the ANS can be observed.6 For example, someone who has taken heroin will have pinpoint pupils. Behind the iris is the lens. The lens is involved in focusing, or accommodation. It is a biconvex, circular, semirigid, crystalline structure that fine-tunes the image on the retina. In a camera the lens is represented by the external optical lens system. The ability to change the focus on the camera is achieved by turning the lens to change the distance of the lens from the film, which effectively increases or decreases the power of the lens, allowing near or distance objects to be seen more clearly. The same effect, a change in the power of the lens, is achieved in the eye by the action of tiny ciliary muscles, which act on suspensory ligaments, thereby changing the thickness and curvature of the lens. A thicker lens with a greater curvature produces higher power and the ability to see clearly at near distances. A thinner lens and flatter curvature produces less optical power, which is what is needed to allow distant objects to be clear (Figure 28-3). The process of lens thickening and thinning is accommodation.4,5 Ideally the lens will bring an image into perfect focus so that it lands right on the fovea, the area of central vision. If the focused image falls in front of the retina, however, then a blurred circle will fall on the fovea (Figure 28-4). In this case the lens is too thick, having too high an optical power. One simple remedy is to place a negative (concave) lens externally in front of the eye in glasses (or contact lenses) to reduce the power of the internal lens and allow the image to fall directly on the fovea. In presbyopia (old eyes), the flexibility of the lens fibers decreases and the lens becomes more rigid.7 Accommodation gets weaker until the image can no longer be focused on the retina. Normal-sighted individuals first begin to notice these changes in their early forties. When this occurs, a plus (positive) lens (or bifocals, progressive lenses, bifocal or monovision contact lenses) may be worn to aid in reading.4 The space behind the lens, which is filled with a gel-like substance, is called the vitreous chamber. As we age, the gel tends to liquefy, and some of the remnants of embryological development that were trapped are released to float freely. This can cause the very common perception of “floaters,” the shadows cast by these particles onto the macular region. They can be disturbing but generally float out of view over time.5 The retina at the back of the eye is the photosensitive layer, like the film in a camera, receiving the pattern of light reflected from objects. The topography of the retina (Figure 28-5) includes the optic disc, which is where the optic nerve exits and arteries and veins emerge and exit. This is also the blind spot because there are no photoreceptor cells on the disc. The macula is temporal to the optic disc and contains the fovea, providing central vision. The surrounding retina provides peripheral vision and defines a 180-degree half-sphere.5 The visual pathway begins with the photoreceptor cells, which begin a three-neuron chain exiting through the optic nerve. This chain consists of the rods and cones, which synapse with bipolar cells that synapse with ganglion cells (Figure 28-6).5,8 The phenomenon responsible for the high degree of neural representation of the foveal region and that accounts for the tremendous conscious awareness of the central view is called convergence.5 At the periphery of the retina the degree of convergence is great; many photoreceptor cells synapse on one ganglion cell, which accounts for poor acuity but high light sensitivity. The closer to the macula, the less the degree of convergence, until, finally, at the fovea there is no convergence. This means that one photoreceptor cell synapses with one bipolar cell and one ganglion cell. The awareness of what is seen is directly related to the amount of convergence, which reflects the extent of neural representation. The 1:1 correspondence between photoreceptor and ganglion cell at the fovea means that there is a high degree of neural representation of the foveal image in the brain. It is even greater than the neural representation of the lips, tongue, or hands.9 This accounts for the primary awareness of what is in the foveal field and secondary awareness of the peripheral field. Conscious awareness of the environment is whatever is in the foveal field at the moment. But continuous information about the environment is flowing over the peripheral retina, usually subconsciously. Attention quickly shifts from foveal to nonfoveal stimulation when changes in light intensity or rapid movement are registered. This type of stimulus arouses attention immediately because it could have specific survival value. For example, a person is driving down the street and senses rapid motion off to the right. The foveas swing around immediately to identify a small red ball bouncing into the street. This information goes to the association areas, in which “small ball” is associated with “small child soon to follow.” Frontal cortical centers are aroused and a decision is made to initiate motor areas to take the foot off the accelerator and put it onto the brake, while simultaneously moving the wheel away from the ball and scanning for the object of concern, that is, the child. The moment light hits the retina, the photographic film model must be abandoned for the image processing or computerized image enhancement model. The primary visual pathway at the retinal level is a three-neuron chain. From back to front the first neuron is the photoreceptor cell, rods or cones. They synapse with a bipolar cell, which in turn synapses with a ganglion cell. The axon of the ganglion cell exits by means of the optic nerve. Image enhancement occurs at the two junctions of the three–nerve-cell pathway. Lateral cells at the neural junctions have an inhibitory action on the primary three-neuron pathway, and through the inhibition of an impulse the image is modulated. For example, at the first junction between photoreceptor cell and bipolar cell, there are horizontal cells. These cells enhance the contrast between light and dark by inhibiting the firing of bipolar cells at the edge of an image. This makes the edge of the image appear darker than the central area, which increases the contrast and thereby increases attention-getting value. After all, it is by perceiving edges that we are able to maneuver around objects. In a similar manner, amacrine cells act at the second neural junction between bipolar and ganglion cells to enhance movement detection.10 The visual pathway continues through the brain (Figure 28-7). The ganglion cell axons exit the eyeball by means of the optic nerve, carrying the complete retinal picture in coded electrochemical patterns. From there the patterns project to different sites within the central nervous system (Figure 28-8). Projections to the pretectum are important in pupillary reflexes; projections to the pretectal nuclei, the accessory optic nuclei, and the superior colliculus are all involved in eye movement functions.5 The largest bundle, called the optic tract, projects to the lateral geniculate body in the hypothalamus, where additional image enhancement and processing occurs. The next group of axons continues to the primary visual cortex and from there to visual association areas. At what point does the retinal image become a perception, and with what part of the brain does one see? Current theory regarding visual perception is the result of Nobel prize–winning research by Hubel and Wiesel in the 1960s called the receptive field theory.11 This theory states that different neurons are feature detectors, defining objects in terms of movement, direction, orientation, color, depth, and acuity. Research in 1990 by Hubel and Livingstone12 was able to locate a segregation of function at the level of the lateral geniculate body. They identified two types of cells, one type being larger and faster magno cells, which are apparently phylogenetically older and color blind but which have a high contrast sensitivity and are able to detect differences in contrast of 1% to 2%. They also have low spatial resolution (low acuity). They seem to operate globally and are responsible for perception of movement, depth perception from motion, perspective, parallax, stereopsis, shading, contour, and interocular rivalry. Through linking properties (objects having common movement or depth) emerges figure-ground perception. Much of this perception occurs in the middle temporal lobe. The eye movement system consists of six pairs of eye muscles: the medial recti, lateral recti, superior and inferior recti, and superior and inferior obliques (see Figure 28-8). Together they are controlled by cranial nerves III (oculomotor), IV (trochlear), and VI (abducens). The eye movement system has both reflex and voluntary components. Reflexive movements are coordinated through vestibular interconnections at a midbrain level. The vestibuloocular reflex (VOR) functions primarily to keep the image stabilized on the retina. Through connections between pairs of eye muscles and the semicircular canals, movement is analyzed as being either external movement of an object or movement of the head or body. From this information the VOR is able to direct the appropriate head or eye movement.5 Before discussing binocular coordination and the individual visual skills, it is important to describe refractive errors and how they can affect binocular coordination. Three common types of refractive errors are myopia or nearsightedness, hyperopia or farsightedness, and astigmatism.5,10 The following are examples of different refractive errors: −5.50 DS (diopter sphere): myopia +1.50 c¯ − 1.50 × 180: astigmatism (Note: × stands for the axis of the cylinder correction.) Binocular coordination is the end result of the efficient functioning of the visual skills (Box 28-1). The individual visual skills include accommodation, eye alignment or vergence, eye movements with normal vestibular coordination, stereopsis (depth perception), and peripheral and central coordination. During normal activities, all the skills are inseparable. Accommodation is the ability to bring near objects into clear focus automatically and without strain. Relaxation of accommodation allows distant objects to come into focus. The primary action is that of the ciliary muscles acting on the lens, and the primary system of control is the ANS, with sympathetic and parasympathetic components.5 Both accommodation and pupil size changes are reflexes that work in concert: as accommodation relaxes the pupil dilates and as accommodation increases the pupil constricts.4 As a person focuses on a near object, the lenses thicken, allowing the near object to come into focus. At the same time the pupils constrict to increase depth of focus (just as in a camera). As a person looks into the distance, the lens gets flatter, relaxing accommodation, and the pupil dilates, decreasing the depth of field. Problems in pursuits or saccades can be the result of a dysfunction of any individual muscles, the VOR, or areas of the brain controlling pursuits or saccades.13–15 Because the VOR helps to stabilize the image on the retina and to differentiate image movement from eye movement, simple tracking can be more difficult. In addition, visual field loss, either central or peripheral, can dramatically affect localization ability. People with blind half- or quarter-fields can be observed to do searching eye movements rather than directly jumping to the object. Memory also may be affected by an eye movement dysfunction. Research by Adler-Grinberg and Stark16 and Noton and Stark17 examined patterns of eye movements as subjects looked at a picture. Distinct eye movement patterns, called scan paths, became apparent. When the subject was asked to recall the picture, the same eye movement pattern was elicited as when the subject originally saw the picture. It would appear that a type of oculomotor praxis is involved in recall. Applying this idea to the clinical setting, if a patient has inaccurate eye movement with poor pursuits or excessive saccades, then perhaps the stored memory is less efficiently stored and consequently more difficult to reconstruct from memory. Additionally, if a patient has a type of brain damage with generalized dyspraxia, the eye movement system could quite likely be affected and might be involved in the patient’s perceptual dysfunction. Another more recent example of the relationship between eye movements and memory is the use of eye movement desensitization and reprocessing (EMDR) therapy to help individuals with posttraumatic stress disorder reintegrate traumatic experiences.18 Although the exact mechanism is at this time unknown, the prevailing hypothesis is that the lateral eye movements elicit an orienting response, scanning the environment for further danger, and that this is an investigatory reflex associated with a relaxed physical state.19 Clinical observations include the following: Phoria is measured in units of prism diopters, which indicate the size of the prism needed to measure the eye position in or out from the straight-ahead position.4 The essential concept in understanding the difference between phoria and strabismus is that in strabismus fusion and depth perception are not present. Definitions of different types of strabismus are presented in Box 28-2. It is not a conclusive list; many other types and permutations are beyond the scope of this discussion. The intent here is to expose the therapist to different terms that may be used by the physician in diagnosing the type of strabismus. Many convergence problems are amenable to vision therapy,20–22 but some are not.23 Whether a particular problem can be helped by vision therapy can be determined by an eye doctor, who can prescribe specific exercises. Oculomotor dysfunction is a very common sequela of neurological deficits, with an incidence as high as 90% according to Ciufredda and colleagues.24,25 Commonly the smooth pursuit system will be affected, such that the smooth movement is interrupted by a series of fixation stops and the movements appear jerky. Damage anywhere along the visual motor pathway may cause a variety of eye movement disorders. This includes injury to the pontine and mesencephalic reticular formation, oculomotor nucleus in the brain stem, caudate nucleus and substantia nigra, cerebellum, and vestibular nuclei.24 As mentioned previously, detection of peripheral targets serves to direct an eye movement with a specific velocity and direction to bring the foveas in line for purposes of identification. Therapy for rehabilitation of eye movement disorders should be directed at using peripheral awareness with slow controlled eye movement toward the target. Once these movements are tolerated, head movement can be added, then slowly body movement.26,27 Visual field loss may indicate damage that is prechiasmic, at the optic chiasm, postchiasmic, in the visual radiations of the thalamus, or in the visual cortex. The resultant visual field loss is characteristic (even diagnostic) in each case. The visual field loss pattern will generally reflect the location of the lesion. It could be bitemporal (outer half of each field), half-field loss (hemianopsia) with or without macular involvement, or quarter-field loss (see Figure 28-7). Some symptoms of field loss are an inability to read or starting to read in the middle of the page, ignoring food on one half of the plate, and difficulty orienting to stimuli in a specific area of space. Hemianopsia is a loss of half of the visual field in each eye, and quadrantanopsia is loss of a quarter of the visual field in each eye. Homonymous hemianopsia refers to the inner or nasal half and the outer or temporal half of each eye being affected. The retina itself is intact, but a neurological lesion has interrupted the ability of the visual cortex to receive recognition of the image. Vision processing may be occurring at lower centers, such as the lateral geniculate body, but if signals are not being received by the cortex, then they are not recognized as “seen.” In 1979, Zihl and von Cramon28 published their findings that damaged visual fields could be trained by use of a light stimulus presented repeatedly at the border of the visual field defect. Balliet and co-workers29 (when attempting to repeat the experiment, adding controls for oculomotor fixations) proposed that subjects were actually learning to make small compensatory eye movements rather than experiencing true improvements in the visual fields. In the 1980s and 1990s a group of German researchers developed a computer-based field training system for researching the question of visual field training. They found in their research that visual fields did expand on average by 5 degrees, with functional improvements noted by more than 80% of their patients (Figure 28-9).30–34 A company called NovaVision introduced the computer-based visual field restitution training program in the United States with good results (see Appendix 28-A). This author has also noted documentable and functional improvements in visual fields even when trained with less sophisticated methods. Table 28-1 summarizes primary visual deficits. Once a therapist or other specialist has eliminated the possibility of primary visual deficits, the clinician must assess whether the identified problem is resulting from central associative processing that is causing visual-perceptual dysfunction. TABLE 28-1 Copyright by Mary Jane Bouska, OTR/L, 1988. Modified by Laurie R. Chaikin, OD, OTR/L, FCOVD. The incidence of retinopathy of prematurity is increasing because of the improved survival of premature infants as a result of improved ventilation.35 Immature retinal vessels are sensitive to high oxygen tension. The effect on the vessels is vasoconstriction, eventually leading to obliteration of the vessels. This creates a state of ischemia, which stimulates the growth of new blood vessels. These small, fragile vessels bleed easily, leading to fibrosis and traction on the retina. As a result of the traction, the macula gets stretched, interfering with the function of central vision. The temporal vessels are most affected because they develop last. The degree of damage may be mild or severe, depending on the amount of prematurity.7 Therapists who work with children with cerebral palsy may have noticed a high incidence of vision problems. Many studies confirm these observations. A study by Scheinman36 examining the incidence of visual problems in children with cerebral palsy and normal intelligence found the following incidences: strabismus in 69%, high phorias in 4%, accommodative dysfunction in 30%, and refractive errors in 63%. In the senile cataract the lens slowly loses its ability to prevent oxidation from occurring, and liquefaction of the outer layers begins. The normally soluble proteins adhere together, causing light scatter.3 Vision slowly declines as opacification and light scatter increase, until the lens must be removed. Age-related macular degeneration (AMD) is the leading cause of blindness in the Western world and is the most important retinal disease of the aged (affecting 28% of the 75- to 85-year-old age group).7 Loss of central vision results from fluid that leaks up from the deeper layers of the retina, pushing the retina up and detaching it from the nourishing layer. New vessel growth and hemorrhage and atrophy further destroy central vision. There is much research going on regarding treatments for AMD. The most promising at this time is the use of bevacizumab (Avastin) or ranibizumab (Lucentis), which is injected into the eye; then the eye is treated with a laser. The drug targets the neovascular network of blood vessels, and the laser treatment obliterates the vessel network, sparing the photoreceptors.37 Glaucoma occurs in 7.2% of the 75- to 85-year-old age group.7 It is generally caused by an increase in the intraocular pressure. This pressure interferes with the inflow and outflow of blood and nutrients at the optic disc. As it progresses, glaucoma can cause tunnel vision and, in some, complete blindness. Because of the type of vision loss affecting the periphery, mobility and safety are significantly impaired. Try walking around holding a paper towel tube to your eye while closing the other eye, and see what happens to your ability to maneuver around obstacles or find your destination.
Disorders of vision and visual-perceptual dysfunction
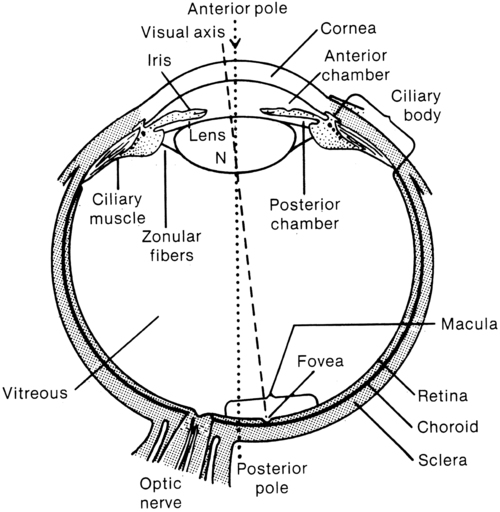
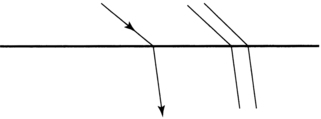
Anatomy of the eye
Eye chamber and lens
Iris
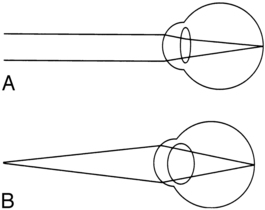
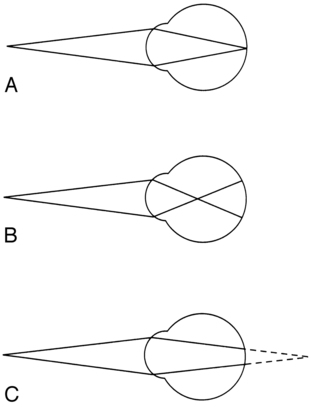
Lens
Vitreous chamber
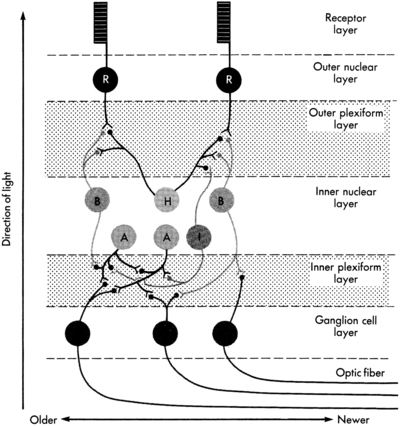
Retina
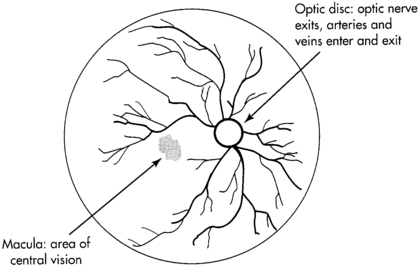
 Retinal topography.
Retinal topography.
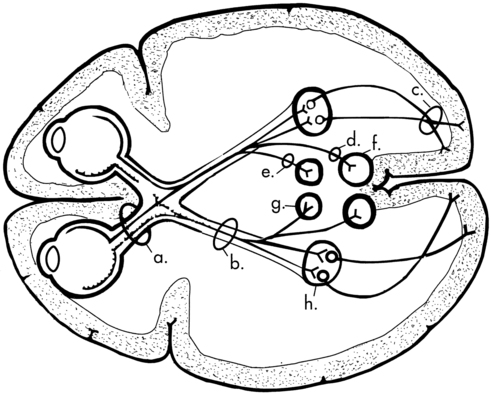
Visual pathway
Exercise 28-3: peripheral central awareness
Eye movement system
Functional visual skills
Refractive error
Accommodation
Pursuits and saccades
Symptoms of visual dysfunction
History
 Are you having difficulty with seeing, or with your eyes?
Are you having difficulty with seeing, or with your eyes?
 Do you wear glasses? Contact lenses? For distance, near, bifocals, or monovision (one eye near, other distance)?
Do you wear glasses? Contact lenses? For distance, near, bifocals, or monovision (one eye near, other distance)?
 Does your correction (glasses, contact lenses) work as well now as before the (stroke, accident, and so on)?
Does your correction (glasses, contact lenses) work as well now as before the (stroke, accident, and so on)?
 Have you noticed any blurriness? Near or far?
Have you noticed any blurriness? Near or far?
 Do you ever see double? See two? See overlapping or shadow images?
Do you ever see double? See two? See overlapping or shadow images?
 Do you ever find that when you reach for an object that you knock it over or your hand misses?
Do you ever find that when you reach for an object that you knock it over or your hand misses?
 Do letters jump around on the page after reading for a while?
Do letters jump around on the page after reading for a while?
 Are you experiencing any eye strain or headaches? Where and when?
Are you experiencing any eye strain or headaches? Where and when?
 Do you ever lose your place when reading?
Do you ever lose your place when reading?
 Are portions of a page or any objects missing?
Are portions of a page or any objects missing?
 Do people or things suddenly appear from one side that you did not see approaching?
Do people or things suddenly appear from one side that you did not see approaching?
 Head turn or tilt during near tasks, or postural adjustments to task
Head turn or tilt during near tasks, or postural adjustments to task
 One eye appears to go in, out, up, or down
One eye appears to go in, out, up, or down
 Eyes appear red, puffy, or irritated or have a discharge (Notify nurses or physician of these observations.)
Eyes appear red, puffy, or irritated or have a discharge (Notify nurses or physician of these observations.)
 Has difficulty maintaining eye contact
Has difficulty maintaining eye contact
 Spaces out, drifts off, daydreams
Spaces out, drifts off, daydreams
 During activity, neglects one side of body or space
During activity, neglects one side of body or space
 During movement, bumps into walls or objects (either walking or in a wheelchair)
During movement, bumps into walls or objects (either walking or in a wheelchair)
 Underreaches or overreaches for objects
Underreaches or overreaches for objects
Phoria and strabismus
 Esophoria: The eyes are postured in front of the point of focus.
Esophoria: The eyes are postured in front of the point of focus.
 Exophoria: The eyes are postured in back of the point of focus.
Exophoria: The eyes are postured in back of the point of focus.
Oculomotor dysfunction
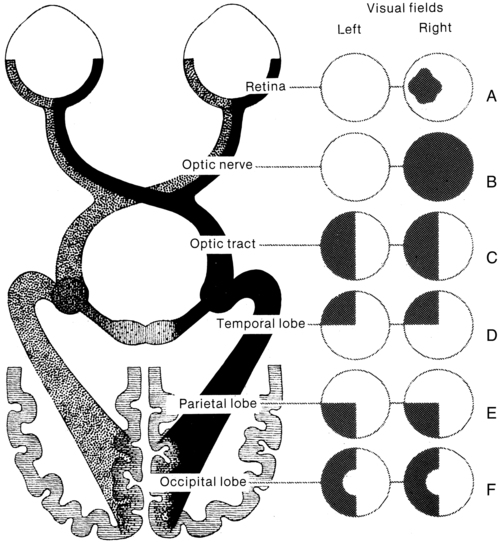
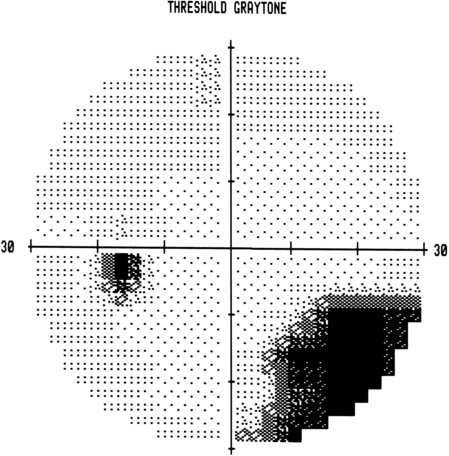
Visual field defects—hemianopsia and quadrantanopsia
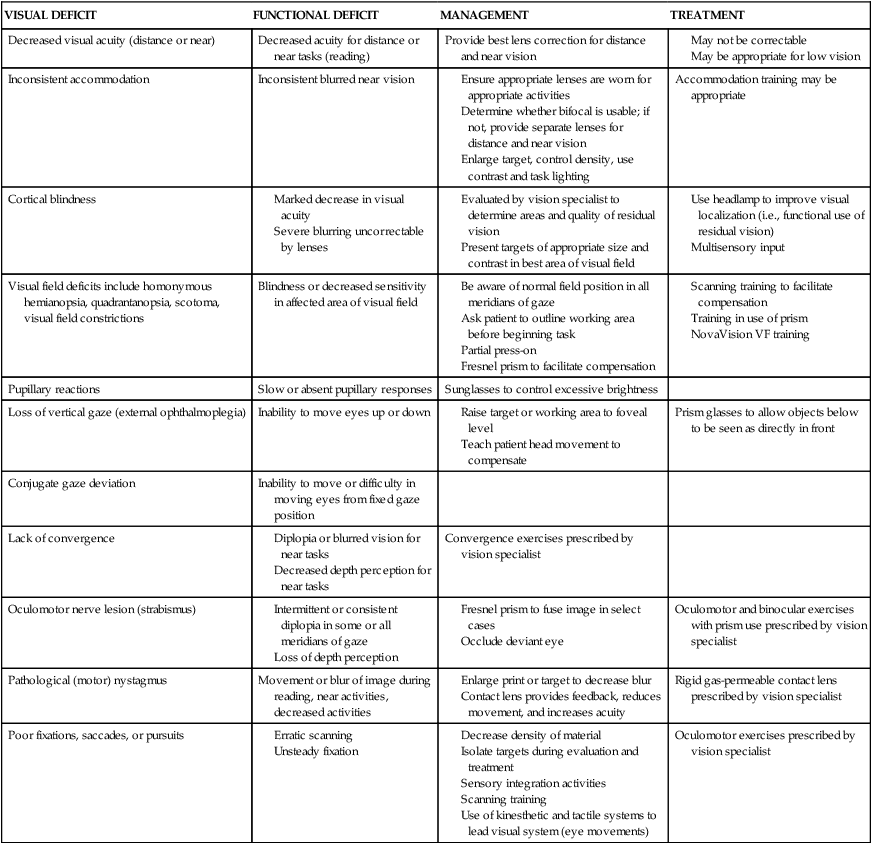
Summary of disorders of vision

VISUAL DEFICIT
FUNCTIONAL DEFICIT
MANAGEMENT
TREATMENT
Decreased visual acuity (distance or near)
Decreased acuity for distance or near tasks (reading)
Provide best lens correction for distance and near vision
Inconsistent accommodation
Inconsistent blurred near vision
Accommodation training may be appropriate
Cortical blindness
Visual field deficits include homonymous hemianopsia, quadrantanopsia, scotoma, visual field constrictions
Blindness or decreased sensitivity in affected area of visual field
Pupillary reactions
Slow or absent pupillary responses
Sunglasses to control excessive brightness
Loss of vertical gaze (external ophthalmoplegia)
Inability to move eyes up or down
Prism glasses to allow objects below to be seen as directly in front
Conjugate gaze deviation
Inability to move or difficulty in moving eyes from fixed gaze position
Lack of convergence
Convergence exercises prescribed by vision specialist
Oculomotor nerve lesion (strabismus)
Oculomotor and binocular exercises with prism use prescribed by vision specialist
Pathological (motor) nystagmus
Movement or blur of image during reading, near activities, decreased activities
Rigid gas-permeable contact lens prescribed by vision specialist
Poor fixations, saccades, or pursuits
Oculomotor exercises prescribed by vision specialist
Eye diseases
Pediatric conditions
Retinopathy of prematurity
Cerebral palsy
Age–related conditions
Cataracts.
Age-related macular degeneration.
Glaucoma.
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Disorders of vision and visual-perceptual dysfunction
Only gold members can continue reading. Log In or Register to continue