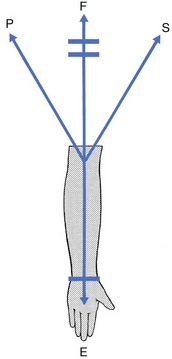
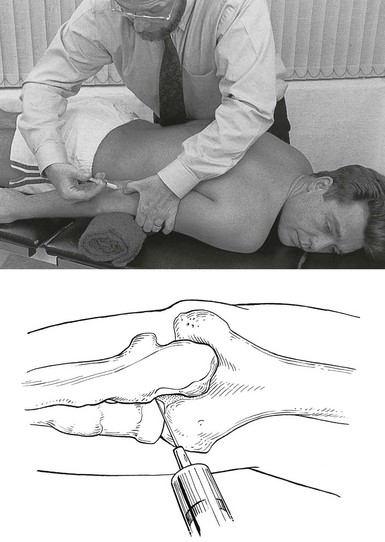
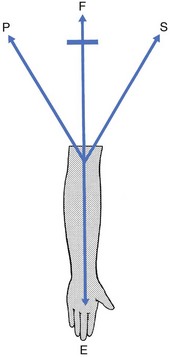
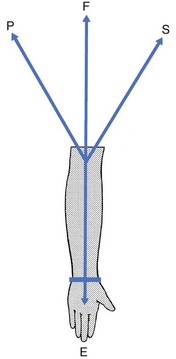
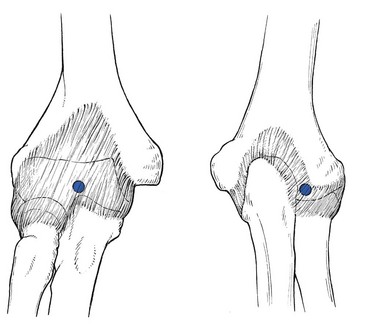
18 The capsular pattern at the elbow is characterized by limitation of flexion and extension (Fig. 18.1), flexion usually being more limited than extension, although equal limitation of both movements does occur. Rotations remain full and painless except in advanced arthritis, in which they can be painful at the end of the range. The following conditions are the most common. On palpation, some swelling may be detected. If the swelling came on immediately after an accident, it is probably caused by blood and this should be aspirated at once. If not, the effusion is secondary and disappears as soon as the arthritis subsides. Also, a positive fat pad sign on a lateral radiograph – a response to distension of the joint capsule – is indicative of intra-articular fluid.1,2 There are two situations that are worthy of attention. The olecranon lies superficially and is therefore very vulnerable. Injury to the elbow, and especially a fall on a bent elbow, may result in fracture of the olecranon. It is, of course, tender to the touch and marked articular signs are found on examination: warmth, swelling and limitation of passive movement in the capsular pattern.3,4 Resisted movements are also positive in that isometric extension, an action of the triceps muscle, is painful and weak (see also p. 453). Radiography confirms the fracture and its type: it is mostly displaced but stable, and then requires surgery. When it is not displaced, immobilization suffices.5 Radial head fractures account for about 30% of all elbow fractures and mostly occur as a result of falling on to an outstretched hand.6 They are most common in females.7 Treatment options for radial head fractures include conservative treatment, excision, open reduction–internal fixation, and arthroplasty, all depending on the type of fracture and the degree of displacement.8,9 Technique: intra-articular injection The patient lies prone on a couch with a small pillow under the elbow. The arm is held by the side with the forearm fully supinated. In this position the joint lines between humerus and radius and the radial side of the olecranon are both easily felt. A 2 mL syringe is filled with triamcinolone acetonide 10 mg/mL and a 2 cm thin needle is fitted. The needle is inserted at the joint line and aimed slightly obliquely under the olecranon (Fig. 18.2). Another valuable treatment is rest in flexion. It can be used in those patients who cannot tolerate an injection. As soon as the patient is seen, the elbow is immobilized in as much flexion as possible by means of a collar-and-cuff bandage. Every day the elbow is flexed more, until full movement can be achieved; thereafter it is held in this position for 2 weeks. The elbow is then rested in slightly less flexion. Three days later the joint is re-examined and, if the range of flexion is still full, the forearm is allowed to extend a little further. Some 6 weeks later, the patient reaches the stage in which the arm can be worn in a sling. After 2 or 3 months, movements of the elbow should be full and painless. Another static progressive splinting method by means of a turnbuckle splint has proved to be useful in the treatment of long-standing post-traumatic stiffness of the elbow.10,11 This condition may come on spontaneously in late middle age12 and is often bilateral. It may also occur as the result of a fracture or dislocation.13 Intra-articular distal humerus fractures, for example, are most often associated with the development of degenerative joint disease over time.14 Repeated minor injuries15,16 or a loose body in the joint may also account for early arthritic changes.17 The patient, most often a male,18 complains that, after he uses his elbow excessively, the joint aches slightly. He may also find the inability to fully straighten the arm inconvenient. The differential diagnosis is neuropathic arthropathy,19 which presents with gross painless limitation of movement in the capsular pattern. On radiography, decalcification and later erosion of cartilage may be visible. Gout (uric acid crystals) and pseudogout (calcium pyrophosphate crystals) seldom affect the elbow joint during a first attack (in only 4.5% of gout cases)20 but more frequently cause acute olecranon bursitis.21 As disease develops, polyarticular attacks may occur, in which case the elbow joint is affected in 30% of cases. The sudden unprovoked onset and the shiny red appearance of the joint are characteristic. The following diagnostic criteria may be useful in gout. When uric acid crystals are found in the synovial fluid during microscopic, chemical or histological examination, or tophi are seen on the ears, the diagnosis is certain, as it also is when two of the following four criteria are present: history of a typical attack of gout at the big toe; history of two typical attacks of gout at another joint; clinical picture of tophus; remission within 48 hours of the acute attack after the administration of colchicine or phenylbutazone.22 Haemarthrosis may occur after injury to the joint, especially an intra-articular fracture or a direct contusion of the joint capsule, or, less commonly, in haemophilic patients. Bleeding into the joint leads to gross swelling and a marked capsular pattern.23 Aspiration must be carried out immediately to avoid destruction of cartilage. Polyarticular rheumatoid arthritis may affect the elbow joint. Apart from the gross swelling, rapidly ensuing limitation of extension is typical.24 The elbow is also one of the sites of predilection, together with the knee and shoulder, for chondromatosis. Pigmented villonodular synovitis occurs most commonly at the knee, followed by elbow and ankle.25 In these and the other rheumatoid-type arthritides, systemic medication is required, and sometimes even a surgical approach. Good results have been reported with total elbow arthroplasty.26–33 A bacterial infection of the elbow joint is always very serious. It may not only lead to total destruction of the joint but may also be life-threatening.34 It can be the result of an open injury to the joint (e.g. open fracture), penetration of a foreign body (e.g. rose or bramble thorns during gardening or fruit picking) or direct inoculation of a bacterium during intra-articular injection, especially injection of a steroid suspension. It can also be caused by haematogenous dissemination from focal infections: dental abscess, cystitis, urethritis, skin infections. These causes are very dependent on the patient’s resistance to infections: patients with diabetes, renal failure or a deficient immune system (e.g. rheumatoid arthritis) are more likely to suffer from haematogenous dissemination followed by a septic arthritis.35–37 Treatment consists of systemic antibiotic therapy and daily local aspiration38 and drainage by arthroscopy.39 Elbow tuberculosis is a rare disease which accounts for 1–3% of all cases of osteoarticular tuberculosis.40 The diagnosis is very difficult to make because of the insidious onset with mild and non-specific local or systemic symptoms. The radiological findings are also non-specific in the early stage. Tuberculosis of the elbow is therefore easily misdiagnosed as degenerative arthritis or rheumatoid arthritis.41 Several months after the onset of symptoms, there is pain at night, and examination reveals a gross capsular pattern and a spastic end-feel. The radiograph reveals periarticular osteopenia, bone erosion and joint space narrowing.42 On haematological testing, the erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) are elevated.43 The gold standard for the diagnosis of tuberculous arthritis is identification of Mycobacterium tuberculosis either directly or after culture of the synovial fluid.44 A loose body in the elbow joint is not uncommon and may hinder normal movements. It prevents the joint either from moving into full flexion, leaving extension free (Fig. 18.3), or from moving into full extension, leaving flexion free (Fig. 18.4). It then changes the hard end-feel of extension into a rather soft one. A loose body is a common cause of elbow trouble in adolescents and is the only non-traumatic cause of arthrosis encountered in a young person. The condition does not occur before the age of 14 and usually results from osteochondritis dissecans, mostly on the humeral capitellum,45,46 or an intra-articular chip fracture, conditions that may lead to exfoliation of one or more fragments of bone covered by articular cartilage.47 Osteochondritis dissecans is not uncommon in young female gymnasts with hyperextension and valgus of the elbow.48–50 It also affects young pitchers or athletes involved in high-demand, repetitive overhead activities.51,52 Diagnosis can be confirmed by anteroposterior radiography performed with the elbow in 45° of flexion,53 because in this position the X-ray beam is almost parallel to the gap between the fragment and the underlying capitellar bone. Recently, magnetic resonance imaging (MRI) has been suggested for assessing osteochondritis dissecans,54 and sonography also seems to be effective.55,56 If the patient is seen during an attack, manipulative reduction can be carried out. However, arthroscopic57,58 or surgical59 removal of the loose piece(s) should always be advised for the following reasons: as the loose body has an osseous nucleus and still lies within its nutrient synovial fluid, it may grow and the condition may worsen at each attack. It is also important to realize that the loose body is considerably larger than it may seem on a radiograph, as it is covered with radiotranslucent cartilage. If surgery is not performed, loose bodies may finally cause gross arthrosis.60 Limitation of extension may considerably hinder activities and should therefore be prevented. A very clear non-capsular pattern is found with limitation of either flexion or extension, depending on the position of the fragment. If the loose body lies in the triangle formed by the humeral capitellum, the head of the radius and the base of the coronoid process of the ulna, extension is slightly limited, while flexion remains full and painless. The end-feel on passive extension is soft. When the loose piece of cartilage lies anteriorly, flexion is quite limited, the fragment catching between the anterior aspect of the humerus and the tip of the coronoid process (Fig. 18.5). A loose body that limits extension can usually be reduced. Manipulation under strong traction shifts the loose piece of cartilage to a position at the back of the joint. It then no longer blocks movement, which becomes normal again. The manipulation can be repeated each time derangement occurs. Nothing else should be done, unless recurrence is very frequent, in which case removal during arthroscopy would be a possibility.61,62 A loose body that limits flexion cannot be reduced by manipulation, but limitation of flexion, unless gross, is not a major concern. The alternatives in this case are: arthroscopic or surgical removal or nothing, depending on the patient’s age, preference and functional disablement.63
Disorders of the inert structures
Limited range of movement
Capsular pattern
Traumatic arthritis
Fracture of the olecranon
Fracture of the head of the radius
Treatment
![]()
Arthrosis
Monoarticular steroid-sensitive arthritis
Crystal synovitis
Haemarthrosis
Rheumatoid-type arthritis
Septic arthritis
Tuberculous arthritis
Non-capsular pattern
Limitation of flexion or extension in isolation
Loose body in the joint
In adolescence
In a normal joint in adulthood
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree