Dislocations
Thomas F. Smith
Robert G. Aguilar
Sonya Kurichh
Dislocations represent injuries to the structures that bind joints together. The soft tissue structures around joints provide strength for stability yet permit freedom for motion. There are a large number of joints within the foot and ankle, each of which may be susceptible to some form of soft tissue injury. The osseous disruption witnessed in fractures may be obvious on radiographs, but the ligamentous damage that occurs with dislocations can be extrapolated only from clinical and x-ray evaluation. The injury may vary from a simple sprain to occult joint subluxation to frank joint dislocation. The findings may be representative of a significant degree of ligamentous compromise, depending on the joint involved.
Careful diagnosis and appropriate early reduction, stabilization, and later rehabilitation of dislocations of the foot aid in reducing the recovery time and the ultimate functional impairment from these injuries. In some instances, pedal dislocations can be missed or misdiagnosed. Generally, patients with unreduced dislocations or unidentified redislocations are more prone to posttraumatic arthrosis and pain. With an awareness of dislocations that may develop within the foot, one may more readily identify the acute problem or better understand the processes that may lead to chronic symptoms.
GENERAL CONSIDERATIONS
The history may be an important component in appreciating dislocations within the foot. Understanding pedal dislocations may be facilitated by an understanding of the how, where, and when of the traumatic incident. It is important to evaluate the neurovascular status of the foot to ensure tissue viability. Pedal dislocations may involve tremendous forces, and the resultant damage may affect not only neurovascular structures but also the tendons in the involved area. Loss of tendon function may be due to entrapment of the tendon within the affected joint, potentially preventing closed reduction of the dislocation. Careful palpation of the involved joint area may help in detecting subtle injuries. Breaks in the continuity of the skin should be evaluated because an open dislocation requires special attention and may drastically alter the postreduction treatment program.
Standard radiographs of the foot are usually adequate for the initial assessment of a pedal joint injury. Three views may be necessary to depict subtle dislocations. Significant pedal injuries may warrant the use of ankle radiographs to rule out other associated trauma. In some patients, the presence of associated injuries may be the only clue of a dislocation within the foot or ankle. The malalignments associated with dislocations may be very subtle. Main and Jowett (1) reported a delay in diagnosis in 30 of 73 cases of midtarsal dislocation related to inadequate radiographs. Fractures may accompany dislocations, thus requiring that all pedal and ankle osseous structures be carefully evaluated. The normal joint alignments of all pedal joints in all planes should be appreciated on evaluation.
Once these factors have been evaluated, then the mechanism of the injury may be more evident. Establishing the mechanism of the injury is important for two reasons. The reduction maneuvers of most pedal dislocations are primarily an exaggeration of the original injury pattern, followed by a reversal of this process. Furthermore, associated trauma around the joint may be evaluated more logically if the mechanism of injury can be determined. Some injury patterns are predictable and the components less likely to be unappreciated if a pattern of injury is established.
Postreduction radiographs should be carefully evaluated for fractures or dislocations obscured by osseous overlap and malalignment present in the prereduction films. Depending on the type of injury, there may be certain sequelae that are predictable complications. Although the postreduction radiographs of a dislocated joint may appear normal, the extraarticular damage can have a devastating prognosis, even in a properly managed patient.
SUBTALAR JOINT DISLOCATION
According to Shands (2), the first case involving subtalar joint dislocation was reported in the literature in 1811 by
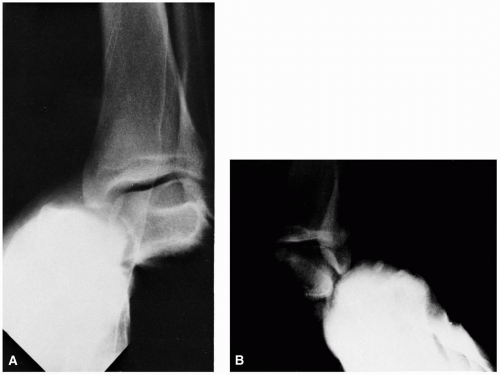
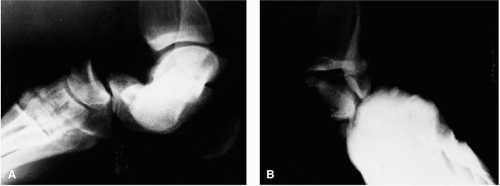
Judey and Dufaurest. The incidence of this injury is estimated to be approximately 1% of all dislocations (3,4). The nomenclature for subtalar dislocations has varied, and descriptions have appeared in the medical literature under many headings including luxatio pedis sub talo, subastragalar dislocation, and peritalar dislocation (5). Classic subtalar dislocation actually involves disruption of not only the subtalar joint but the talonavicular joint as well (6). Talocalcaneonavicular joint dislocation is probably a more descriptive nomenclature. At present, the term most commonly employed is subtalar dislocation. Subtalar dislocations are categorized by the position of the foot in relation to the talus. In medial subtalar dislocation, the foot lies medial to the talus. In a lateral subtalar dislocation, the foot is lateral to the talus (Fig. 1). In an anterior subtalar dislocation, the foot is anterior to the talus, and in posterior subtalar dislocation, the foot is posterior.
Judey and Dufaurest. The incidence of this injury is estimated to be approximately 1% of all dislocations (3,4). The nomenclature for subtalar dislocations has varied, and descriptions have appeared in the medical literature under many headings including luxatio pedis sub talo, subastragalar dislocation, and peritalar dislocation (5). Classic subtalar dislocation actually involves disruption of not only the subtalar joint but the talonavicular joint as well (6). Talocalcaneonavicular joint dislocation is probably a more descriptive nomenclature. At present, the term most commonly employed is subtalar dislocation. Subtalar dislocations are categorized by the position of the foot in relation to the talus. In medial subtalar dislocation, the foot lies medial to the talus. In a lateral subtalar dislocation, the foot is lateral to the talus (Fig. 1). In an anterior subtalar dislocation, the foot is anterior to the talus, and in posterior subtalar dislocation, the foot is posterior.
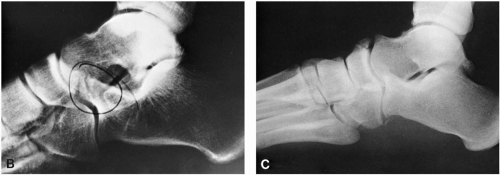
A subtalar dislocation is nearly identical in clinical presentation to a Hawkins type II fracture of the neck of the talus. Both injuries include complete disruption of the subtalar joint in either a medial or lateral injury pattern. However, in a Hawkins type II injury, radiographic evaluation demonstrates a displaced talar neck fracture and an intact talonavicular joint, as opposed to the disruption of the talonavicular joint associated with a classic subtalar dislocation (Fig. 2C,D). Interestingly, swivel dislocations of the midtarsal joint are also nearly identical in clinical presentation to Hawkins I talar neck fractures. Both present with little clinical evidence of malalignment. Either injury can be easily missed both clinically or radiographically (Fig. 2A,B). The swivel dislocation of the midtarsal joint presents with a total disruption or, more commonly, a partial subluxation of the talonavicular joint. The Hawkins I talar neck fracture generally has minimal displacement of the fracture and, like a swivel dislocation of the midtarsal joint, minimal subtalar involvement.
Anatomic Considerations
Ligaments and soft tissues that normally support the subtalar and ankle joints can be disrupted in subtalar dislocations. The subtalar joint is reinforced by a joint capsule. Thickenings within the capsule known as the medial and lateral talocalcaneal ligaments help bind the subtalar joint medially and laterally. The sinus tarsi contains the interosseous talocalcaneal ligament. It is composed of thickenings of the anterior aspect of the subtalar joint and the posterior aspect of the talocalcaneonavicular joint capsules. The ligamentum cervicis lies at the lateral aspect of the sinus tarsi, attached to the neck of the talus and below to the calcaneus (7). These ligaments are all disrupted with subtalar joint dislocations.
The talocalcaneonavicular joint complex is supported by a joint capsule known as the talonavicular ligament. The
ligament surrounds the joint and blends into the deltoid ligament as the two main supporting structures of the talonavicular joint. In the first phase of a subtalar dislocation, the talar head punctures the talonavicular joint capsule. The bifurcate ligament and the spring ligament are not disrupted in this injury because these ligaments course directly from the calcaneus to the cuboid or navicular and do not include the talus. The relationship of the calcaneus, cuboid, and navicular, and the associated soft tissue structures remains intact in subtalar joint dislocations.
ligament surrounds the joint and blends into the deltoid ligament as the two main supporting structures of the talonavicular joint. In the first phase of a subtalar dislocation, the talar head punctures the talonavicular joint capsule. The bifurcate ligament and the spring ligament are not disrupted in this injury because these ligaments course directly from the calcaneus to the cuboid or navicular and do not include the talus. The relationship of the calcaneus, cuboid, and navicular, and the associated soft tissue structures remains intact in subtalar joint dislocations.
An important clinical consideration is the involvement of the ankle ligaments in this injury because the deep portions of the deltoid ligament and the calcaneofibular ligament are torn with both medial and lateral subtalar dislocations (8). This is understandable because both ligaments cross the subtalar joint and bind the calcaneus to the ankle through the talus. The deltoid ligament inserts along the sustentaculum tali of the calcaneus from the tibia. The calcaneofibular ligament attaches to the midportion of the lateral surface of the calcaneus from the fibula (7). Instability, stiffness, and pain of the ankle are potential sequelae of a subtalar dislocation.
Classification
Medial Subtalar Dislocations
The most common type of subtalar dislocation is the medial subtalar dislocation (2,3,9, 10, 11, 12, 13), and it may be the predominant injury pattern in as much as 84% of patients (12). The higher incidence of medial subtalar dislocations may be due to the greater degree of instability in the subtalar joint to inversion forces (14). The clinical appearance of the injury has prompted some authors to describe the medial subtalar dislocation as “basketball foot” or “acquired clubfoot” (15, 16, 17).
Larsen (16) described the mechanism of injury for medial subtalar joint dislocations as a forceful inversion of the foot. The sustentaculum tali acts as a fulcrum for the posterior body of the talus to produce the dislocation. The talonavicular joint is dislocated first as the talar head punctures the lateral talonavicular joint capsule. A rotary subluxation of the subtalar joint itself then occurs as the calcaneus proceeds medially with the navicular under the talus. Leitner (18) believed further that medial subtalar dislocation represented
the primary stage of a total dislocation of the tarsus and ankle. The ankle is weakened by this injury and further inversion force could produce gross ankle dislocation (Fig. 1A).
the primary stage of a total dislocation of the tarsus and ankle. The ankle is weakened by this injury and further inversion force could produce gross ankle dislocation (Fig. 1A).
A number of subtalar dislocations can present as open injuries, 37% in one report (12). Open subtalar dislocation is a severe injury in which only fair functional and poor anatomic results can be expected (19). The primary factor that influences the outcome of open subtalar dislocations is infection, not the time elapsed before treatment, direction of the dislocation, or associated fractures (20). Subtalar joint dislocations have a high incidence of associated fractures, approaching nearly 30% (13). In one study, 68% of patients were found to possess associated osteocartilaginous joint injuries (12). The inversion force that produces the dislocation can produce predictable bone and soft tissue injuries at remote sites in the foot and ankle. The associated injuries and their incidence were summarized by Christensen et al. (10). With the force of inversion, avulsion of bone or rupture of soft tissue elements may develop elsewhere in the lateral column of the foot and ankle. In the medial column, one will more likely note compression injuries of the respective bones and soft tissues. Fractures of the lateral navicular, dorsomedial head of the talus, and posterior process of the talus are the most common associated osseous injuries (Fig. 3). Associated soft tissue injuries include injury to the tibial nerve, laceration of the posterior tibial artery, and rupture of the posterior tibial tendon (21). The dorsalis pedis artery and deep peroneal nerve can become entrapped between the talus and navicular (22).
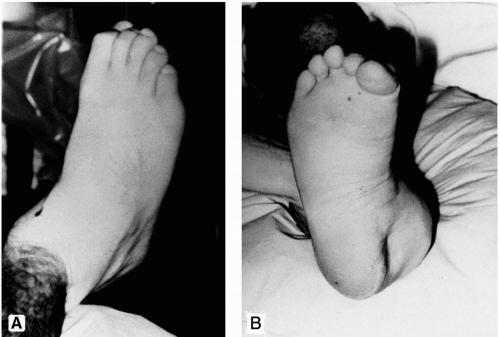
In patients with medial subtalar dislocation, the head of the talus is palpable on the dorsum of the foot (Fig. 4). The head of the talus is disarticulated from the navicular and lies between the extensor hallucis longus and the extensor digitorum longus tendons, and rests on the dorsal surface of the navicular or cuboid. The overlying skin may be tight and blanched, and soft tissue necrosis is possible if reduction is delayed. The calcaneus, along with the rest of the foot, is displaced medially with respect to the leg. The medial border of the foot appears shortened, whereas the lateral border appears lengthened. The digits may appear dorsiflexed. The lateral process of the talus is easily palpable laterally. The sustentaculum tali and navicular are palpable medially, whereas the tibial malleolus is not visible.
Radiographic examination of medial subtalar dislocations is facilitated by both ankle and foot studies (Fig. 5). Ankle injuries may require surgical reduction and, therefore, may alter the postreduction treatment program. The anterior ankle radiograph demonstrates the medially displaced foot through the subtalar joint, with the talus intact in the ankle mortise. Lateral radiographs of the foot and ankle demonstrate overlap of the talus with the tarsal bones and no clear subtalar joint. Depending on the angle of the x-ray tube, the head of the talus may be visible dorsal to the midtarsal bones. The foot appears more as it would in an oblique radiograph. The calcaneocuboid joint remains congruous. The dorsoplantar radiograph exhibits a medially displaced navicular with a nonarticular talonavicular joint. Kite’s angle is negative.
Lateral Subtalar Dislocations
Lateral subtalar dislocation results from forced eversion of the tarsus. The anterior calcaneal process acts as a fulcrum
for the anterolateral corner of the talus (8). The joint disruptions of this injury follow a sequential pattern. First, the head of the talus is forced through the talonavicular joint capsule medially. In the next step, the subtalar joint is disrupted as the calcaneus is forced laterally. Lateral subtalar dislocations may require a greater force to develop. As in medial subtalar dislocation, disruption of the ankle ligaments and other soft tissues occurs in lateral subtalar dislocation, yet with an opposite effect (Fig. 1B). Lateral subtalar dislocations have a greater incidence of associated fractures than do medial subtalar dislocations (9,13). The fractures tend to consist of avulsion injuries along the medial column of the foot and ankle, and compression injuries along the lateral column.
for the anterolateral corner of the talus (8). The joint disruptions of this injury follow a sequential pattern. First, the head of the talus is forced through the talonavicular joint capsule medially. In the next step, the subtalar joint is disrupted as the calcaneus is forced laterally. Lateral subtalar dislocations may require a greater force to develop. As in medial subtalar dislocation, disruption of the ankle ligaments and other soft tissues occurs in lateral subtalar dislocation, yet with an opposite effect (Fig. 1B). Lateral subtalar dislocations have a greater incidence of associated fractures than do medial subtalar dislocations (9,13). The fractures tend to consist of avulsion injuries along the medial column of the foot and ankle, and compression injuries along the lateral column.
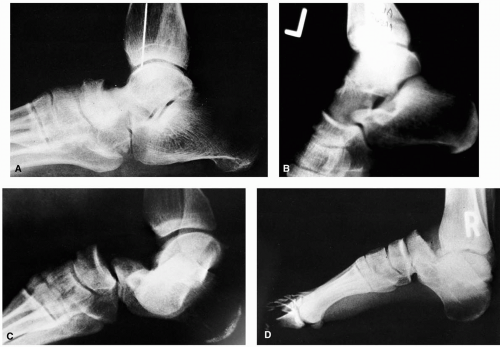
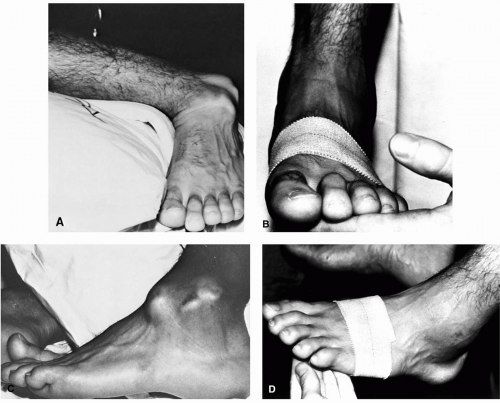 FIG. 4. Clinical presentation of a medial subtalar dislocation. Prereduction (A) and postreduction anteroposterior view of foot (B). Prereduction (C) and postreduction lateral view of foot (D). |
In a lateral subtalar dislocation, the foot is displaced lateral to the leg (Fig. 6). The lateral border of the foot appears shortened, whereas the medial border appears lengthened. The digits appear plantarflexed because of the stretch placed on the structures of the tarsal canal. The talar head is palpable medially, and the fibular malleolus is obscured laterally.
Radiographic evaluation of lateral subtalar dislocations is facilitated by studies of both the ankle and the foot. Associated eversion-type ankle injuries are possible. Foot fractures remote from the dislocation may be noted. As in medial subtalar dislocations, lateral foot radiographs demonstrate overlap of the tarsal bones without a demonstrable subtalar joint. The navicular is laterally displaced from the talus in the anteroposterior foot radiograph (Fig. 7). Anterior ankle radiographs reveal an intact ankle mortise and talus, with the foot laterally displaced. The calcaneocuboid joint remains congruous.
Posterior Subtalar Dislocations
Posterior dislocations of the subtalar joint have been reported, but are extremely rare, accounting for less than 1% of subtalar joint dislocations (15,23). These injuries usually result from falls from a height on an outstretched foot in a plantarflexed position, resulting in hyperplantarflexion injury (16). Clinically, the longitudinal axis of the foot appears normal. The forefoot appears shortened, with the heel protruding posteriorly. Radiographs demonstrate a foot that is posteriorly displaced, with the talus remaining in the ankle mortise (Fig. 8). Reduction is carried out by reversal of the mechanism of injury. Heel traction is first applied to disengage the dislocation for reduction, and the foot is then dorsiflexed on the talus (24).
 FIG. 5. Radiographic presentation of a medial subtalar dislocation. Prereduction (A) and postreduction anteroposterior view of foot (B). Prereduction (C) and postreduction (D) lateral view of foot. |
Anterior Subtalar Dislocations
Anterior dislocations are also rare injuries (15). Anterior dislocation results from a fall from a height with axial loading onto a dorsiflexed foot. Clinically, the foot appears lengthened longitudinally with a flattened heel (16). Reduction is accomplished by distracting the foot distally with heel traction. The foot is then forcefully directed backward under the talus (24). A rare case of anterior subtalar joint dislocation associated with a large talar fragment that prevented closed reduction has been reported (25).
Treatment
Generally, closed reduction is a procedure that requires general or spinal anesthesia, or intravenous sedation. Intravenous muscle relaxants may be needed to relax muscle
spasms and splinting about the tarsal joints and ankle. Reduction of the dislocation should proceed as quickly as possible to relieve pressure on vital structures and relax skin tension over the bony prominences created by the injury. The reduction maneuvers are based on the mechanism of injury and the sequence of events involved in the dislocation.
spasms and splinting about the tarsal joints and ankle. Reduction of the dislocation should proceed as quickly as possible to relieve pressure on vital structures and relax skin tension over the bony prominences created by the injury. The reduction maneuvers are based on the mechanism of injury and the sequence of events involved in the dislocation.
For medial subtalar dislocations, distal traction is initially applied to the heel and countertraction is applied to a flexed knee. This helps relax the gastrocnemius muscle and facilitates reduction. First, relocation of the talocalcaneal component of the subtalar joint dislocation is accomplished. An inversion force is applied to the foot, followed by an eversion force and a return to the neutral subtalar joint position while distal traction force is maintained. Second, the talonavicular component of the subtalar dislocation is reduced by downward pressure on the head of the talus while the foot is plantarflexed. The foot is then dorsiflexed and pronated to relocate the head of the talus with the navicular.
Certain obstacles may prevent a successful closed reduction of the medial subtalar joint dislocation. These obstacles include impaction of the navicular with the talar head, talar head buttonholing through the extensor retinaculum, peroneal tendons that may become entrapped around the talar head, and talar head buttonholing through the extensor digitorum brevis muscle belly (3). Closed reduction maneuvers are possible to help overcome these obstacles (3,22). Open reduction may be indicated in resistant cases to release the talar head from entrapment in local soft tissue or osseous structures. The incision is placed laterally over the head of the talus and oriented proximal to distal. Any structures that bind the head of the talus may then be released, permitting reduction.
The maneuvers for reduction of lateral subtalar dislocations follow the same principles as those for medial dislocations. Distal traction is applied to the calcaneus around a flexed knee. Relocation of the talocalcaneal joint is accomplished first because this phase of the injury occurred last. The foot is forcefully everted, followed by inversion of the foot about the talus to a neutral position. The talonavicular joint is reduced by pressure on the head of the talus, with the foot held in a pronated position. The tibialis posterior tendon (3,26,27), long flexor tendon (6), or impaction fracture of the navicular and talus (8) may prevent closed reduction. Open reduction is carried out through an incision lateral to the head of the talus oriented proximal to distal. Structures that may be binding the head of the talus may be released, and compromise of medial skin is thus avoided.
After reduction, a compression dressing is applied. These dressings are maintained and vascular status is monitored until swelling is controlled, generally for the first 3 to 5 days following the injury. Internal fixation or percutaneous wire fixation is generally not indicated for subtalar dislocation alone, although fixation may be required for fractures associated with the injury. There has been one report of an unstable reduction of the subtalar joint that required fixation owing to an associated fracture of the sustentaculum tali (28). Postreduction radiographs are employed to assess the adequacy of reduction. A reevaluation is then performed because fractures may be more evident at this point than with the overlap of osseous structures in the prereduction radiographs.
As devastating as these injuries may seem, the long-term disabilities and complications have not been reported as severe (5,8, 9, 10, 11,16,28,29). Skin necrosis is the most immediate complication that may be encountered. Christensen et al. (10) reported skin necrosis in 3 of 30 patients, one requiring skin grafting. Trauma blisters may also be noted (30). The long-term complications resulting from this injury include postural deformations, ankle instability, avascular necrosis of the talus, arthritis, and pain (10). Stiffness of the subtalar joint has been consistently noted, although a limited range of motion is not necessarily related to disability and pain (8,9,11). Radiographic changes in the posterior facet of the subtalar joint appear most frequently, although Monson and Ryan (11) noted that when tarsal pain did develop after injury that the most common site was at the talonavicular joint. Significant subtalar joint pain was not appreciated in their patients. Avascular necrosis of the talus is not considered a common complication of subtalar dislocation as an isolated injury (10,11,29).
In 1944, Plewes and McKelvey (31) first reported the absence of this complication. Two cases have been reported with associated fractures of the posterior process of the talus (9,10). Damage to the posterior talus may serve to compromise further circulation already affected by damage to the vessels of the sinus tarsi and appears to increase the risk of avascular necrosis. If a fracture of the posterior process fracture is present, then careful monitoring of the talus is indicated. Subtalar dislocations associated with ankle dislocations have a poor prognosis, with avascular necrosis of the talus being a strong possibility.
An interesting finding has been that subjective long-term pain is greater when associated injuries have required prolonged
immobilization (8,10,12). Current trends in treatment are to promote early ambulation with the protection of a below-the-knee cast. Guarded weight-bearing cast support has been used as initial treatment in these cases. Physical therapy modalities, including whirlpool and range-of-motion exercises, may be continued for 3 to 4 months. Early results after an average of 2 years have been encouraging. This bears out McKeever’s findings in 1963 that early guarded ambulation helps prevent subtalar stiffness and pain (32).
immobilization (8,10,12). Current trends in treatment are to promote early ambulation with the protection of a below-the-knee cast. Guarded weight-bearing cast support has been used as initial treatment in these cases. Physical therapy modalities, including whirlpool and range-of-motion exercises, may be continued for 3 to 4 months. Early results after an average of 2 years have been encouraging. This bears out McKeever’s findings in 1963 that early guarded ambulation helps prevent subtalar stiffness and pain (32).
MIDTARSAL (CHOPART’S) JOINT DISLOCATION
Trauma to the midtarsal, or Chopart’s, joint is a relatively common injury and is frequently overlooked. Main and Jowett (1) reported a delay in diagnosis in 30 of 73 cases owing to inadequate radiographs. They recommend anteroposterior, lateral, and oblique views of the foot for a more accurate diagnosis and postreduction assessment. A feature that is common to both midtarsal and classic subtalar dislocation is a subtle disruption of the talocalcaneal relationship. Radiographic evidence of subluxation and malalignment of the subtalar joint may be a helpful clue to identify minimally incongruous midtarsal dislocations. Both subtalar dislocations and midtarsal dislocations can involve a talonavicular dislocation.
Main and Jowett (1) proposed a classification system based on the mechanism of injury. They defined midtarsal joint injuries according to the direction of the force producing the dislocation. The forces that produce these injuries make up the basis for the classification system and include medial, longitudinal, compression, lateral, plantar, and crushing force injuries. They also proposed a classification of swivel injury or tarsal rotation injury. This dislocation may occur within either medial or lateral force injury classifications. In the classification proposed by Main and Jowett, there were no components described of pure dorsal midtarsal injury. Others have agreed (33,34), and the premise is that a force directed dorsally through the foot will produce injury primarily at the tarsometatarsal joint.
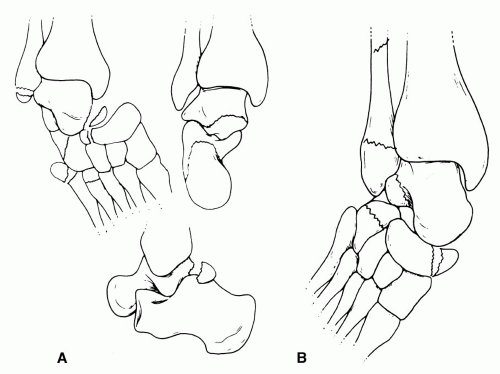
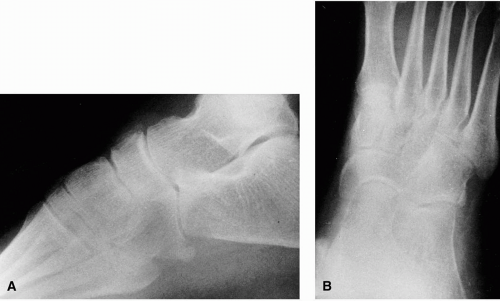 FIG. 9. Medial force midtarsal joint fracture sprain. A: Dorsal talonavicular joint flake fractures. B: Calcaneocuboid joint avulsion fracture. |
Medial Force Midtarsal Injury
Medial force midtarsal joint injury occurs secondary to a force directed at the lateral aspect of the foot in a medial direction. An inversion-type midfoot injury similar to an inversion ankle sprain is typical of this pattern. Medial force midtarsal joint dislocation can result in three grades of joint trauma. The first type, fracture sprain, is the mildest form of midtarsal injury. Radiographically, with a fracture sprain, one may visualize only flake fractures of the talus or navicular dorsally and avulsion fractures of the calcaneus or cuboid laterally (Fig. 9). The second type or stage of medial force midtarsal injury is fracture subluxation. Fracture subluxations are evidenced by a medially displaced forefoot through the midtarsal joint, with a normal talocalcaneal relationship. This injury represents a greater degree of compromise to the midtarsal joint soft tissues (Fig. 10). The third type of medial force midtarsal joint dislocation is the swivel dislocation. Swivel dislocations may be considered similar to the first step of a subtalar dislocation. The mechanism appears to be a rotation of the midtarsal joint about an axis that corresponds to the interosseous talocalcaneal joint. The talonavicular
joint subluxates with the head of the talus lateral or dorsal to the navicular. The calcaneocuboid joint remains intact (Fig. 11). The subtalar joint is subtly deviated but not totally disrupted. The mild radiographic incongruity of the subtalar joint can be a useful radiographic clue that a swivel dislocation exists.
joint subluxates with the head of the talus lateral or dorsal to the navicular. The calcaneocuboid joint remains intact (Fig. 11). The subtalar joint is subtly deviated but not totally disrupted. The mild radiographic incongruity of the subtalar joint can be a useful radiographic clue that a swivel dislocation exists.
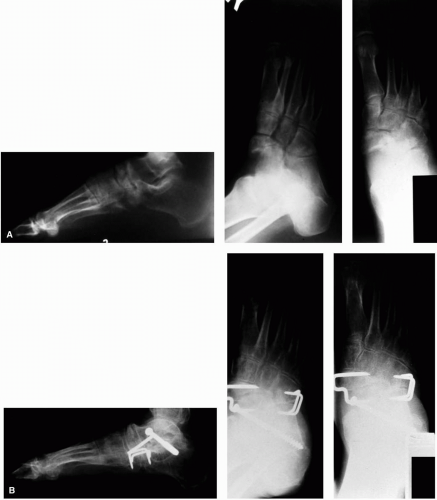
 FIG. 10. Medial force midtarsal joint fracture subluxation. Prereduction (A) and postreduction anteroposterior view of foot (B). Prereduction (C) and postreduction lateral view of foot (D). |
Medial force midtarsal injuries are reduced by distal forefoot traction and reversal of the mechanism of injury. A wide variety of treatment programs have been attempted from strapping to casting, both with and without weight bearing. The most satisfactory treatment for medial fracture sprain and fracture subluxation has been a compression dressing and non-weight bearing for 1 to 2 weeks, followed by use of a weight-bearing cast for 4 to 6 weeks. Persistent midtarsal pain has accompanied immediate weight bearing with or without a cast. Early identification and treatment is essential.
Swivel dislocation of the midtarsal joint represents a severe tarsal malalignment mandating immediate reduction. Delay in reduction of these injuries due to misdiagnosis most often results in arthritic destruction of the tarsal joints. Triple
arthrodesis appears to afford the only surgical solution to aid in the persistent pain if the diagnosis is missed and reduction is not effected (35) (Fig. 12).
arthrodesis appears to afford the only surgical solution to aid in the persistent pain if the diagnosis is missed and reduction is not effected (35) (Fig. 12).
Longitudinal Force Midtarsal Injury
Longitudinal force midtarsal joint injury is due to a force directed from distal to proximal through the foot. This injury can be likened to kicking or striking the forefoot distally against a fixed or firm object. These longitudinal forces can result in fractures and dislocations of either the proximal or distal joints of the navicular. The fracture and dislocation pattern depends on the site of maximal compression between the talus and cuneiforms. Dorsal or plantar subluxation of the navicular fracture fragments is possible. This is a serious injury to the articular portions of the navicular, both proximally and distally (Fig. 13).
Lateral Force Midtarsal Injury
Lateral force injuries result from stress directed to the medial foot in a lateral direction. Fracture sprains are mild clinical injuries with tenderness about the midfoot region and few radiographic findings other than edema. The primary factor that distinguishes a lateral force midtarsal injury from a medial force midtarsal injury is a history of an eversion-type force through the foot. Lateral force fracture sprains can be identified radiographically by avulsion fractures of the navicular tuberosity, flake fractures over the dorsal talonavicular joint region, and impaction fractures of the calcaneus and cuboid. Fracture subluxations result from greater force and may result in a talonavicular lateral subluxation combined with compression injury of the cuboid. Hermel and Gershon-Cohen’s (36) nutcracker cuboid fracture and the cuboid extrusion injury of Drummond and Hastings (37) fall into this category. Swivel injuries result in a medially displaced talus from the navicular and an intact calcaneocuboid joint.
Lateral force midtarsal injuries are potentially the most serious in terms of joint pain and long-term instability (38). This is believed to be caused by disruption of the rigid lateral column needed for normal ambulation. Calcaneocuboid fusion is recommended for persistent symptoms. For most patients with persistent pain and instability following medial or lateral midtarsal injury, triple arthrodesis is recommended as opposed to talonavicular arthrodesis alone. This recommendation is based on the fact that all three major tarsal joints are typically involved in most tarsal joint dislocations. Recurrent midtarsal joint subluxations have been reported (39).
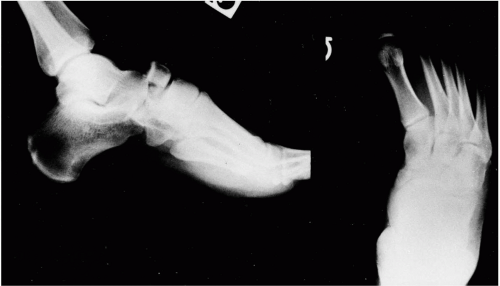 FIG. 13. Longitudinal force midtarsal joint fracture-dislocation. Note the fractures of the navicular and the adductus attitude of the foot. |
Lateral force midtarsal joint injuries are managed in a similar manner to medial force midtarsal joint injuries. The degree of non-weight bearing and immobilization is based on the severity of the injury. The distinction of the various grades of lateral force midtarsal joint injury is pertinent also for accurate prognosis.
Plantar Force Midtarsal Injury
These injuries result from forces directed on the dorsum of the foot in a plantar direction. Mild forms of this injury can result in little clinical evidence of malalignment, with pain only in the midfoot region. The talocalcaneal relationship generally remains intact. Milder injuries are demonstrated radiographically with dorsal talonavicular avulsion flake fractures and an intact midtarsal joint relationship. More severe forms of plantar force midtarsal injury can result in a plantarly dislocated navicular and cuboid relative to the talus and calcaneus, with gross evidence of deformity. Impaction fractures of the inferior aspect of the calcaneocuboid joint or the talonavicular joint can occur. Avulsion fracture of the bifurcate ligament origin from the calcaneus can occur with varying degrees of size and complexity (Fig. 14).
Crush Midtarsal Injury
Crush injuries of the midtarsal joint vary in the nature and pattern of injury, and are usually associated with open wounds. Contusion to soft tissues may result in serious vascular compromise and loss of skin and soft tissues (Fig. 15). Review of this injury pattern is more appropriate as a fracture than a dislocation.
TARSOMETATARSAL (LISFRANC’S) JOINT DISLOCATION
Lisfranc’s, or the tarsometatarsal, joint forms a bony arc from medial to lateral across the midfoot region. The anatomy of the articulating surfaces appears as a stone arch with wide dorsal and narrow plantar contours. This osseous configuration, along with the strong ligaments and recessed second metatarsal base, provides the stability for this joint complex (Fig. 16). Dislocations of these joints are rare, representing less than 1% of dislocations reported (40, 41, 42, 43, 44, 45, 46). The severity of the presentation may range from obvious clinical and radiographic malalignment and deformity to a near-normal clinical and radiographic presentation (47,48). Even with accurate diagnosis and appropriate reduction, the chance for morbidity after this injury is great whether the reduction is open or closed. The diagnosis has reportedly been missed in up to 20% of cases (49,50). The potential for disability following a tarsometatarsal dislocation is worse when the diagnosis or treatment is delayed, the reduction is inadequate, or the dislocation recurs (51).
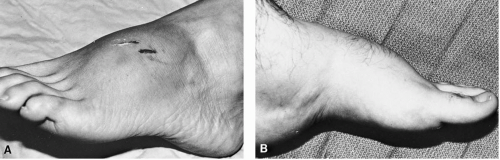 FIG. 15. Midtarsal joint crush injury. A: Contusion and open lacerations around the midtarsal joint. B: Contusion and edema around the midtarsal joint without an open wound. |
The diagnosis of tarsometatarsal dislocation requires little insight when obvious clinical and radiographic malalignment is present. This is contrasted with a diagnosis of tarsometatarsal dislocation that requires a high index of clinical suspicion when few, if any, clinical or radiographic findings exist. Often, the patient recalls an audible snap or pop after experiencing a forced plantarflexion of the forefoot on the
rearfoot. The patient may relate stepping off a curb, slipping on the stairs, or stepping in a hole. The plantarflexed foot sustains a longitudinal force against a fixed surface. This was classically considered an equestrian injury, occurring as the foot was caught in a stirrup by a falling rider (52). Many injuries have also been sustained as the patient stepped into a hole while walking. At present, industrial injuries and motor vehicle accidents appear to be the source of disruption in the majority of cases (43,45,48).
rearfoot. The patient may relate stepping off a curb, slipping on the stairs, or stepping in a hole. The plantarflexed foot sustains a longitudinal force against a fixed surface. This was classically considered an equestrian injury, occurring as the foot was caught in a stirrup by a falling rider (52). Many injuries have also been sustained as the patient stepped into a hole while walking. At present, industrial injuries and motor vehicle accidents appear to be the source of disruption in the majority of cases (43,45,48).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree