Chapter 60 Dislocation of the Proximal Tibiofibular Joint
Dislocation of the proximal tibiofibular joint is a very rare condition that is easily misdiagnosed without suspicion of the injury. Proximal tibiofibular dislocation can be an idiopathic subluxation of the joint, more commonly seen in conjunction with high-energy tibia and ankle fractures. It is most common in sports that involve violent twisting of the knee such as wrestling, parachute jumping, mixed martial arts, gymnastics, skiing, rugby, football, soccer, snowboarding, long jumping, and baseball.* The pathology of the tibiofibular joint is a result of anatomic variations of the proximal joint, the biomechanical axis of the ankle, and training program errors.39 Injury to this structure can be caused by ligaments that strengthen and support the proximal tibiofibular joint, as well as allow the functional structure and the biomechanics of the lower kinetic chain to influence movements at the joint, all of which increase the chance of instability.29,30 Some physicians question the frequency of tibiofibular joint injury due to common misdiagnosis.30,39 Diagnosis of this rare injury will be improved by a better understanding of the anatomy and biomechanics of the joint, the mechanisms leading to instability, and the symptoms that result from this injury.
Anatomy
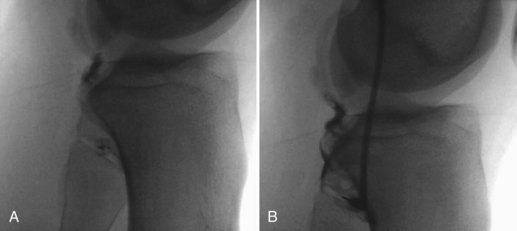
The chief function of the proximal tibiofibular joint is to dissipate some of the forces on the lower leg such as torsional stresses on the ankle, lateral tibial bending movements, and tensile weight bearing.27 The proximal tibiofibular joint is a synovial membrane–lined, hyaline cartilage articulation that communicates with the knee joint in 10% of adults† and must be considered as the fourth compartment of the knee (Fig. 60-1A and B). The joint capsule is strengthened by ligamentous attachments that increase in strength and thickness from anterior to posterior.‡ Responsibility for stabilization of the proximal tibiofibular joint falls on the anterosuperior and posterosuperior tibiofibular ligaments.48 The joint capsule consists of the tibial facet and the fibular facet, located on the posterolateral aspect of the tibial condyle and the medial proximal surface of the head of the fibula, respectively.39
The anterior capsule of the joint is stabilized by the anterior tibiofibular ligament, which consists of three broad bands that pass obliquely distal from the fibular head and connect to the anterior aspect of the lateral tibial condyle. An extension of the deep layer of the biceps femoris tendon located anterior to the anterior proximal tibiofibular ligaments connects on Gerdy’s tubercle and helps to stabilize the anterior joint capsule8,25,28,32,35 (Fig. 60-2).
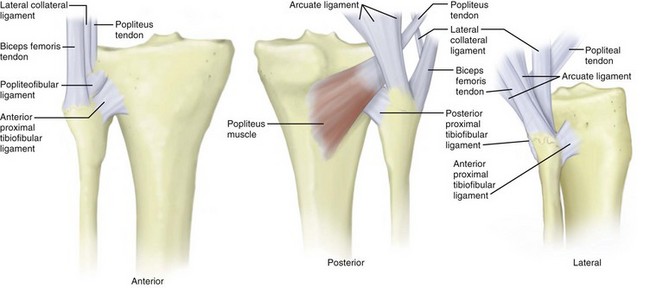
Figure 60-2 Anatomy of the proximal tibiofibular joint.
(© Whiddon DR, Parker TA, Kuhn JE, Sekiya JK: Disorders of the proximal tibiofibular joint. In Scott NW [ed]: Surgery of the knee, ed 4, Philadelphia, 2006, Elsevier, pp 797–803.)
The posterior joint capsule is supported by the posterior proximal tibiofibular ligament, which consists of two thick bands that pass obliquely upward from the fibular head and connect to the posterior aspect of the lateral tibial condyle. The popliteus tendon covers and reinforces the posterior proximal tibiofibular ligament8,28,32,35 (see Fig. 60-2).
Some physicians also believe that the posterolateral structures of the knee, including the arcuate ligament, the fabellofibular ligament, the popliteofibular ligament, the popliteus muscle, the interosseous membrane, and the lateral collateral ligament, stabilize the joint.36,37,44 The lateral collateral ligament arises from the lateral femoral condyle in the midcoronal plane and runs distally and posteriorly to the posterolateral aspect of the fibular head25,27,28 (see Fig. 60-2).
Ogden’s historic 1974 article described two different anatomic variants based on the arbitrary determinant of a 20-degree angle with the horizontal plane.27 The inclination angle for the proximal tibiofibular joint with respect to the horizontal plane is important when the anatomic stability of the joint is determined. The greater the slope that the joint makes with the horizontal plane, the more vulnerable it is to rotational forces.48 Ogden described a horizontal variant as <20 degrees of joint inclination (Fig. 60-3A). It has been observed to have greater resistance to rotational forces because of its position behind the prominent ridge of the proximal tibia and its large planar, circular articular surface with an average surface area of 26 mm2. The horizontal variant was also observed to have greater external rotation compared with the oblique variant.27–29 Ogden described an inclination of >20 degrees as an oblique variant (Fig. 60-3B). This increased angle of inclination can reach as high as 76 degrees and causes a highly variable surface area, averaging 17 mm2, and configuration. The angle of inclination shows an inverse correlation with the surface area of the joint.27,29,35 The oblique variant was found in 70% of the joint injuries described by Ogden and instability is thought to stem from the decreased surface area and increased angle of inclination found in oblique joints.29,45

(© 2003 American Academy of Orthopaedic Surgeons. Reprinted from the Journal of the American Academy of Orthopaedic Surgeons, vol 11[2], pp 120–128, Figure 45-2, with permission.)
The normal orientation of the proximal tibiofibular joint does not sit in a sagittal plane; as a result, it encounters normal movement in the anterolateral and posteromedial direction.39 Anterior-posterior motion during flexion and extension, respectively, is increased in children and gradually decreases with age.27 During anterior movement of the fibular head, the biceps femoris tendon, which inserts on the styloid process and the upper surface of the head of the fibula, adds support and stability.
When the knee is flexed between 0 degrees and 30 degrees, the lateral collateral ligament is tight and supports the joint. When the knee is flexed beyond 30 degrees, the lateral collateral ligament and the biceps femoris tendon relax, causing the proximal fibula to migrate anteriorly. Laxity in the joint capsule caused by the orientation of the knee in the flexed position increases the vulnerability of the proximal tibiofibular joint to injury.27
When the knee is extended, the same structures become tightened, causing the fibular head to return to its posterior position.1,27 Because of the arrangement and tightening of the ligaments around the joint, the proximal tibiofibular joint is most stable when the knee is extended.16,48
The proximal tibiofibular joint is very important in the external rotation of the fibula with ankle dorsiflexion. It has been observed that during movement of the ankle, rotational movement can be observed in the proximal tibiofibular joint.38 The oblique variant causes greater constraint in rotational mobility and is thought to increase torsional loads during forced ankle dorsiflexion, increasing the probability of fibular dislocation or fracture.27
Semonian et al reported that it is important to recognize the neurologic aspect of the lateral region of the knee owing to the fact that many diagnoses of joint instability go unnoticed until patients develop footdrop. The common peroneal nerve passes posteriorly over the head of the fibula and comes in close contact with the proximal tibiofibular joint. The peroneal nerve is palpable along the lateral aspect of the knee because of its path as it wraps around the fibular neck before the peroneus longus muscle overlaps it laterally.39 Physicians diagnosing a patient with anterolateral, posteromedial, or superior dislocation must be aware of peroneal nerve injury.48
Classification of Instability
Ogden described the four commonly used types of dislocation based on the direction of instability of the joint: atraumatic subluxation, anterolateral dislocation, posteromedial dislocation, and the rare superior dislocation.29,35 In Ogden’s study of 43 patients, 10 had subluxation, 29 anterolateral dislocation, 3 posteromedial dislocation, and 1 superior dislocation.29 The literature also describes five cases of inferior dislocation.11,26 Physicians diagnosing this type of injury should be aware of its association with a common peroneal nerve injury that most commonly occurs in patients diagnosed with anterolateral or posteromedial dislocation.5,8
Injury to the anterior and posterior capsular ligaments, and commonly the lateral collateral ligament, can lead to common anterolateral dislocation29,30,35 (Fig. 60-4A). The main cause of this injury is a fall on a hyperflexed knee with the foot inverted and plantarflexed.* Flexion of the knee results in relaxation of the lateral collateral ligament and the biceps femoris tendon, and twisting of the body creates a torque that forces the fibular head laterally to the edge of the bone buttress of the lateral tibial metaphysis.13,29 A reflex contracture of the peroneal, extensor hallucis longus, and extensor digitorum longus muscles, caused by forced plantar flexion and ankle inversion, forces the laterally displaced fibular head anteriorly.4,28,29,32
Posteromedial dislocation typically stems from direct trauma to the knee or from a twisting injury that puts torsional strain on supporting ligaments, causing them to tear27,29,32,35 (Fig. 60-4B). The resulting loss of support causes tension in the biceps femoris tendon to displace the fibular head posteriorly and medially along the posterolateral tibial metaphysis.29
Subluxation typically occurs in patients who have no history of inciting trauma but may have generalized ligamentous laxity; it is not commonly bilateral.29,30,35 The anterior capsule and the anterior ligament of the joint are thought to be involved in proximal tibiofibular joint subluxation.39 Symptoms of subluxation include excessive anterior-posterior motion without actual dislocation of the joint.
Superior dislocations are caused by tearing of the tibiofibular interosseous membrane and result in dislocation of the entire fibula29 (Fig. 60-4C). The superior migration of the entire fibula commonly results from high-energy ankle injuries.35 They are commonly found in conjunction with lateral malleolar and tibial fractures.29,32 Atraumatic superior dislocation of the proximal tibiofibular joint has been seen in conjunction with congenital dislocation of the knee.29
Five cases of inferior proximal tibiofibular dislocation have been described in the literature, and all were associated with severe neurovascular injury and fracture of the tibial shaft.11,26 In all cases, the common peroneal and tibial nerves were affected; all were high-energy motorcycle injuries.11
Clinical Presentation
Early recognition of injury to the proximal tibiofibular joint is important to optimize management and avoid potential misdiagnosis.36 Early treatment of these injuries may prevent this condition from developing into chronic or fixed subluxation, which is more difficult to treat.39 Before a diagnosis of proximal tibiofibular joint instability is made, the integrity of surrounding ligamentous structures must be checked because of the common injuries that can present with the same symptoms.48 When a patient presents with high-energy trauma, the proximal tibiofibular dislocation may be missed initially because of other traumatic injuries such as fracture of the tibial plateau or shaft, ipsilateral femoral head or shaft, distal femoral epiphysis, ankle fracture, or knee dislocation.10,29
Anterolateral injury usually occurs after a fall on a flexed knee or a violent twisting motion during an athletic activity, and prominent pain is common over the lateral aspect of the knee, along with a prominent fibular head.* Pain commonly causes the patient to be unable to bear weight on the affected leg; range of motion in the knee is limited, especially knee extension, and motion of the ankle may cause more pain.46,51 Patients often present with pain along the biceps femoris tendon, which appears as a tense, curved cord. Pain that is increased by extending the flexed knee and by dorsiflexing and everting the foot is also seen.29
Posteromedial dislocations are common after direct trauma to the knee with pain secondary to that trauma. Common peroneal nerve injury can be seen with these injuries, even though symptoms are usually transient.5
Subluxation is seen most commonly in adolescents, can be bilateral, and usually presents with pain on the lateral side of the knee that is increased by direct pressure over the fibular head.29,30 Instability of the knee can be demonstrated by moving the fibular head anteriorly and laterally by relaxing the lateral collateral ligament and the biceps femoris tendon with the knee flexed 90 degrees.14 Muscular dystrophy, Ehlers-Danlos syndrome, and generalized ligamentous laxity can be associated with subluxation.29,30,39,41 Prepubescent females commonly exhibit laxity and usually experience a decrease in symptoms as they reach skeletal maturity.29–31,41,42 Other associated events include osteomyelitis, rheumatoid arthritis, septic arthritis, previous below-the-knee amputations, osteochondroma, and growth disturbances around the knee, as well as runners who have recently increased their mileage.3,23,29,35,39
Recurrence of chronic dislocation of the proximal tibiofibular joint is often missed because its symptoms mirror a wide range of other knee conditions. Most patients usually live their daily lives without symptoms until they become involved in activities that require sudden changes in direction, such as athletic movement.12 It is common for patients to complain of sensations of knee instability or giving way, especially while climbing stairs.42 The nature and location of this injury often mimic those of other knee pathologies, such as injury to the lateral collateral ligament or biceps femoris tendon, posterolateral rotatory instability, iliotibial band syndrome, or tendinitis of the popliteus tendon or biceps femoris tendon.39 Associated symptoms of instability with clicking or popping also mimic a lateral meniscus injury, exostosis, or intra-articular loose bodies in the popliteus tendon sheath.†
Superior dislocations are rare and usually present after high-energy trauma with lateral knee pain and the displaced fibular head as a lateral mass.29,35 They commonly occur with associated tibial and ankle fractures and often require surgery for correction.29 Inferior dislocations have been described in the literature as having a very poor prognosis; four of five cases result in above-knee or below-knee amputation.26 Posterolateral dislocation was described in the literature in one case and is not mentioned as one of the four types of dislocation by Ogden.43 It is not uncommon for patients with chronic instability of the proximal tibiofibular joint to be diagnosed with Charcot-Marie-Tooth (CMT) disease or to undergo diagnostic knee arthroscopy for this problem, so this condition should be considered in the differential diagnosis in patients with lateral knee pain.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree