, Katherine Edwards2, Amanda Marshall5, Brian A. Mosier6, Daniel T. Altman7 , Joyce M. Wilson3, Michael Pensak4 and Jennifer Moriatis Wolf4
(1)
Division Chief Oncology, UCLA Health System, Los Angeles, CA, USA
(2)
Department of Physical Medicine and Rehabilitation, University of Missouri, Columbia, Missouri, USA
(3)
Orthopedic Surgery, Jefferson City Medical Group, Jefferson City, Missouri, USA
(4)
Department of Orthopaedic Surgery, University of Connecticut, Farmington, Connecticut, USA
(5)
University of Texas Health Science Center at San Antonio, San Antonio, TX, USA
(6)
Department of Orthopaedic Surgery, Allegheny General Hospital, Pittsburgh, PA, USA
(7)
Orthopaedic Surgery, Allegheny General Hospital, 1307 Federal St, 2nd Floor, Pittsburgh, PA 15212, USA
1 Genetics
Susan V. Bukata8
(8)
Division Chief Oncology, UCLA Health System, Los Angeles, CA, USA
Take-Home Message
Genetic anomalies can result in significant musculoskeletal issues and perioperative complications and risks.
1.1 Modes of Inheritance
Autosomal Dominant
A single copy of the mutated gene is sufficient to create the disorder; if the gene is present, the disorder will occur.
Autosomal Recessive
Two copies of the mutated gene are for this person to be affected with the disease; single copy of the gene creates a gene carrier but that will not have the disease
X-Linked Dominant
A disorder of a gene on the X chromosome causes a disorder to be expressed in all individuals (both males and females)
Females more frequently affected; no male-to-male transmission.
X-Linked Recessive
Disorder in a gene on the X chromosome, but the disorder will only occur in males and females with two mutated copies of the gene; no male-to-male transmission
Variable Inheritance (Penetrance)
Spectrum of disease severity from a genetic mutation known to cause disease, ranging from no obvious disease to mild to severe. Even within the same family with the same gene mutation, significant variation in disease severity can occur.
Chromosomal Abnormalities
A structural anomaly in the chromosomes resulting in missing, abnormal, or excess DNA compared to normal chromosomes; can occur in all cells in the body or only in select cells (mosaicism)
1.2 Down Syndrome
Definition
Chromosomal anomaly associated with cognitive delay, muscle hypotonia, and other birth defects
Etiology
Trisomy 21 (extra copy of chromosome 21 from one parent), more common from egg but can be from sperm
Rate: 1 per 691 births in the USA.
Can also occur from unbalanced translocation of chromosome 21 and another chromosome. One or both parents may not be affected due to a balanced translocation, but this translocation can become unbalanced in their child(ren), leading to disease.
Pathophysiology
Distinctive facial appearance, 50 % have heart defect, joint instability (hip, patella, neck, and foot), muscle hypotonia in infants, and cataracts
Treatment
Supportive treatment for symptomatic defects, physical therapy, and surveillance
1.3 Turner Syndrome
Definition
Chromosomal anomaly in females that affects development
Etiology
Single X chromosome (50 % of cases) or severely dysfunctional second X chromosome in females
Rate: 1 per 2,500 in females, can present as mosaicism with only some cells affected
SHOX gene on X chromosome most associated with musculoskeletal anomalies in the syndrome
Pathophysiology
Normal intelligence, early ovarian failure (most do not undergo puberty and are infertile), webbed neck (30 %), low hairline, lymphedema of limbs (70 %), skeletal anomalies, renal defects, heart defects (30–50 %), and hypothyroid (10–30 %)
Increased risk of congenital hip dislocation, scoliosis (10 %), delayed skeletal maturation (85 %), short 4th metacarpal, and osteoporosis
Treatment
Hormone therapy to induce puberty, supportive care, physical therapy, and surveillance
1.4 Von Willebrand Disease
Definition
Bleeding disorder with slowed clotting process resulting in easy bruising and prolonged bleeding after injury
Etiology
Most common genetic bleeding disorder
Estimated incidence: 1 per 100 to 1 per 10,000 people
Diagnosis
Bleeding time, tests for von Willebrand factor (quantity and quality)
Pathophysiology
Mutations in the VWF gene reducing the amount of von Willebrand factor produced.
Von Willebrand factor essential for platelet adhesion and stabilizes other clotting proteins preventing their breakdown.
Impaired function prevents clots from forming normally.
Clinical Manifestations
Easy bruising, heavy or prolonged menstrual bleeding, prolonged bleeding after injury, nosebleeds, and excessive bleeding after dental work
Classification
Type I: decreased von Willebrand factor levels, most common type (75 % of patients), mildest form, variable quantities of von Willebrand factor in bloodstream, and autosomal dominant inheritance.
Type II: abnormally functioning von Willebrand factor, intermediate in severity, and autosomal recessive inheritance.
Type III: most severe form with no von Willebrand factor produced, extremely rare (1 per 500,000), autosomal recessive inheritance; mutation creates short nonfunctional protein.
Treatment
Desmopressin nasal spray stimulates release of von Willebrand factor from vascular endothelium.
For severe cases: von Willebrand factor and factor VIII transfusions
For surgery/procedures: may need to have blood products including von Willebrand factor available
1.5 Hemophilia
Definition
Factor deficiency that slows blood clotting process; its classic form is factor VIII deficiency.
Etiology
X-linked recessive mutation in F8 gene; rate: 1 in 5000 males
Produces abnormal version of coagulation protein
Leads to prolonged prothrombin time (PTT)
Pathophysiology
Continuous bleeding after injury, surgery, or dental work, sometimes spontaneous bleeding (joints, muscles, brain)
Treatment
IV replacements with recombinant factor VIII preoperatively, continue 5 days postoperatively, 21 days for bone procedures
Hemophilic Arthropathy
Synovitis and cartilage destruction in a joint due to repeated bleeds
Treatment
Factor replacement, physical therapy, bracing, arthroscopic synovectomy, or total knee replacement for more severe cases
1.6 Christmas Disease
Definition
Clotting disorder deficiencies in factor IX
Etiology
X-linked defect in F9 gene liposomal protein production, second most common form of hemophilia; rate: 1 per 20,000 in males
Pathophysiology
Form of hemophilia, similar effects and treatments as common hemophilia
Treatment
IV infusion factor IX (plasma or recombinant), desmopressin applied directly small wounds
1.7 Gaucher’s Disease
Definition
Cell storage disorder that affects beta-glucocerebrosidase enzyme activity and allows accumulation of glucocerebroside within cells to toxic levels.
Etiology
Autosomal recessive mutations in GBA gene; rate: 1 per 50,000–100,000
In people of Ashkenazi Jewish descent; rate: 1 per 500–1000
Pathophysiology
Hepatosplenomegaly, anemia, thrombocytopenia, bone pain and pathologic fractures, abnormal bone remodeling, delayed healing, arthritis, and lung disease
Increased perioperative bleeding and infection risk
Classification
Type I: most common form, non-neuropathic, more frequent with Ashkenazi Jewish descent
Type II: added effect on the central nervous system and brain, begins in infancy, with brain damage, seizures, and abnormal eye movements
Type III: also affect the central nervous system, slower progression than type II
Treatment
IV enzyme replacement for types 1 and 3
1.8 Sickle Cell Anemia
Definition
Disorder that affects hemoglobin protein and causes red blood cells to distort into crescent/sickle shape
Etiology
Autosomal recessive mutations in HBB gene affect beta-globin subunit of hemoglobin (hemoglobin S form)
Hemoglobin has four subunit: two alpha-globins and two beta-globins
Most common in those of African descent; rate: one for 70,000 in the USA, one in 500 African-Americans, and one in 1,000 Hispanic Americans
Classification
Sickle cell trait: at least one beta-globin subunit replaced by hemoglobin S
Sickle cell disease: globulin subunit replaced I hemoglobin S
Pathophysiology
Symptoms of sickle cell disease seen in early childhood
Anemia, pain episodes, repeated infection, shortness of breath, fatigue, delayed growth and development, osteonecrosis, and pulmonary hypertension
Pain episodes occur when cells undergoes cyclic and have trouble passing through blood vessels.
Treatment
Decitabine or hydroxyurea (induces production of fetal hemoglobin), pain medications, fluids, rest, oxygen if levels are low, and blood transfusion for severe anemia or perioperatively
1.9 Thalassemias
Definition
Disorder that reduces hemoglobin production resulting in difficulties carrying oxygen to cells of the body
Etiology
Defect in quantity in either the alpha or beta subunit of hemoglobin production resulting in low hemoglobin levels
Can occur as major form (both genes for the subunit effected, got one from each parent) or minor form (one gene for the subunit effected, other is normal)
Classification
Alpha thalassemia: involves the alpha subunit of hemoglobin, losses from two genes involved (HBA 1/HBA 2); two forms: HbBart (severe, with loss of all 4 alleles of HBA genes) and HbH (milder, loss of 3 of the 4 alleles; more common in Southeast Asia and Mediterranean countries; complex inheritance because it involves gene copy number
Beta thalassemia: involves the beta subunit of hemoglobin, common globally but most frequent with Mediterranean decent, involves mutations in the HBB gene that range from complete loss of beta-globin production to decreased quantity, generally autosomal recessive inheritance/rare autosomal dominance
Pathophysiology
Decrease oxygen delivery to tissues. Anemia, weakness, fatigue, increased risk of blood clots, jaundice, hepatosplenomegaly, osteoporosis and fragility fractures, and growth retardation
Treatment
Blood transfusions, folate supplementation, iron chelation, and perioperative caution with increased clotting risk
2 Calcium and Phosphate Metabolism
Kate Edwards9
(9)
University of Missouri, Department of Physical Medicine and Rehabilitation, Columbia, Missouri, USA
Take-Home Message
Calcium is an important mineral in the body that is tightly regulated by intact parathyroid hormone, vitamin D, and calcitonin. It is involved in many physiologic processes. Both too much and too little calcium can be pathologic.
Rickets – failure of osteoid to calcify in children resulting in bony abnormalities
Osteomalacia – incomplete mineralization of osteoid following growth plate closure
2.1 Calcium
Calcium is the most abundant mineral in the body with 98–99 % housed in the bone and teeth as hydroxyapatite. In the plasma, 50 % is ionized and active, while 45 % is protein bound (albumin) and 5 % is bound to phosphate and citrate. The total amount of calcium in the extracellular fluid is approximately 1 g. In contrast, the bone contains 1 kg of calcium!
Serum calcium concentration is 8.5–10.2 mg/dL.
To correct for a low albumin, use the following equation: ([4-plasma albumin in g/dL] × 0.8 + serum calcium).
Calcium is required for many physiologic processes including: muscle contraction, enzyme cofactor for hormonal secretion, vascular contraction and dilation, membrane stability, intracellular signaling, bone structure and mineralization, and nerve conduction.
Recommended amount of dietary calcium per the Institute of Medicine is 700–1,300 mg/day based on age with an upper limit of 1,000–3,000 mg/day.
The gut absorbs only 30–40 % of ingested calcium. In contrast, the kidneys are quite efficient and absorb 97–98 % of circulating calcium. Approximately 500 mg of calcium is exchanged daily in the bone with remodeling.
pH is important in calcium regulation. In states of acidemia, there is decreased calcium binding to albumin which increases ionized calcium, while the reverse is true for alkalemia.
Calcium is closely regulated by parathyroid hormone (PTH), vitamin D, and calcitonin. Calcium levels are also affected by magnesium and phosphorous.
2.2 PTH
Stimulates bone resorption
Stimulates calcium reabsorption at the distal tubule of the kidney
Stimulates phosphate excretion
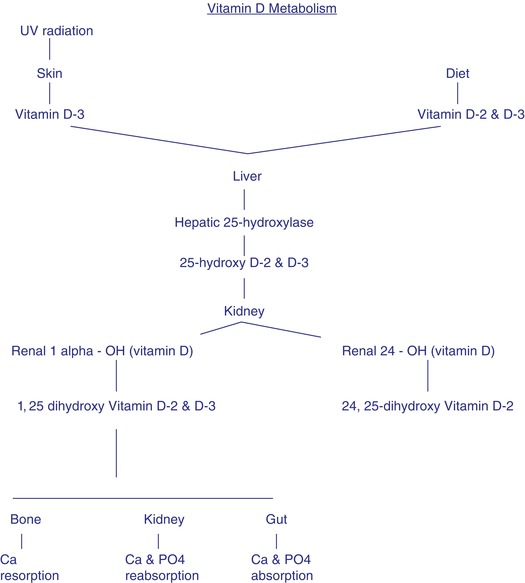
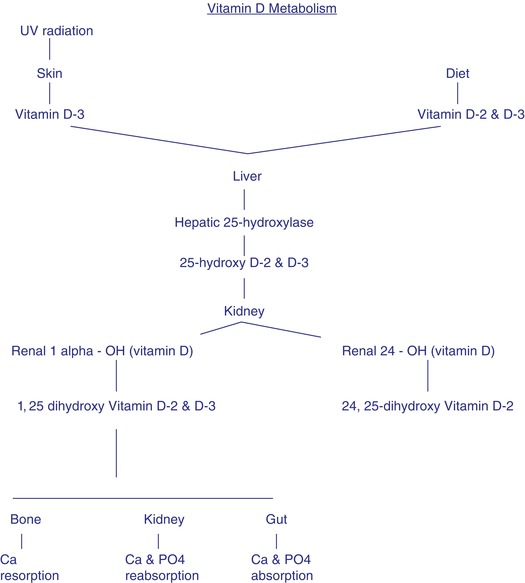
Stimulates conversion of 25 hydroxyvitamin D2 to 1,25 dihydroxyvitamin D3
Indirectly increases gut absorption due to the increased vitamin D
PTH has a very short half-life of 5 min.
PTH receptors are found on osteoblasts. It is thought that PTH inhibits osteoblast function and increases osteoclastic activity via cell-to-cell communication.
The parathyroid gland is extremely sensitive to changes in ionized calcium as detected by calcium-sensing receptors (CaSR) which ultimately regulates the release of PTH.
2.3 Calcitonin
Is a hormone released by the thyroid parafollicular cells in response to elevated calcium levels.
In the bone, it inhibits resorption of calcium, and in the kidney, it inhibits reabsorption of both calcium and phosphate.
2.4 Vitamin D
Stimulates calcium absorption in the gut
Stimulates bone resorption
Stimulates renal reabsorption of calcium
Regulates PTH release
Check serum 25(OH) level, desired level is >30 ng/dL
25(OH) has a longer half-life than the active form, 1,25 dihydroxyvitamin D3 (15 days vs. 4 h), and its concentration is 1,000-fold greater.
As far as oral supplementation, D2(ergocalciferol) and D3(cholecalciferol) are traditionally regarded as equivalents.
2.5 Phosphorous
Most phosphorous in the body is present as phosphate.
80–90 % of ingested phosphorous is absorbed by the gut.
Serum levels are primarily maintained by the rate of kidney excretion.
Serum concentration is 3–4 mg/dL.
Helps maintain physiologic pH.
Deficiency is uncommon except in genetic disorders of phosphate metabolism.
Calcium and phosphate are both deposited and resorbed from bone together.
2.6 Hypocalcemia
Definition
Serum calcium <10.5 mg/dL or ionized calcium <1.0 mmol/L
Causes
Renal failure, vitamin D deficiency, magnesium deficiency, acute pancreatitis, hypoparathyroidism, hyperphosphatemia, and medication effect
Very common in hospitalized patients
Symptoms
Acute – syncope, perioral numbness, fatigue, muscle cramps, and congestive heart failure
Chronic – psoriasis, dry skin, coarse hair, brittle nails, poor dentition, and cataracts
Severe hypocalcemia can but rarely causes tetany, arrhythmias, hypotension, and seizures as well as other signs/symptoms of neuromuscular irritability.
Diagnosis
Ionized calcium level
Check liver function test, albumin, iPTH, magnesium, BUN, and creatinine to assess for secondary causes.
Treatment is with oral versus IV supplementation.
2.7 Hypercalcemia
Definition
Serum calcium >10.5 mg/dL or ionized calcium >2.5 mmol/L
Causes
90 % caused by malignancy or hyperparathyroidism
10 % caused by increased vitamin D levels, thiazide diuretics, renal failure, rapid bone turnover, and familial causes
Symptoms
Anxiety, depression, coma, somnolence, arrhythmia, nephrolithiasis, hypertension, nausea, vomiting, anorexia, and osteoporosis (“stones, bones, abdominal groans, psychiatric moans”)
Treatment
IV fluids, loop diuretics, IV bisphosphonates, calcitonin, dialysis, and glucocorticoids
2.8 Rickets
Definition
Disease of growing bone affecting children
Causes
Failure of osteoid to calcify typically from prolonged vitamin D deficiency.
Vitamin D deficiency → decreased serum calcium → +PTH → increased renal phosphorous loss → decreased deposition of calcium in the bone
Demographics
More common in exclusively breastfed babies and those with little sunlight exposure. Also present in conditions that cause malabsorption such as celiac disease and seen in severe renal disease.
Physical Exam
Skeletal deformity (bow leg, knock knee, rachitic rosary), short stature, dental defects, kyphoscoliosis, and delay in closure of fontanels
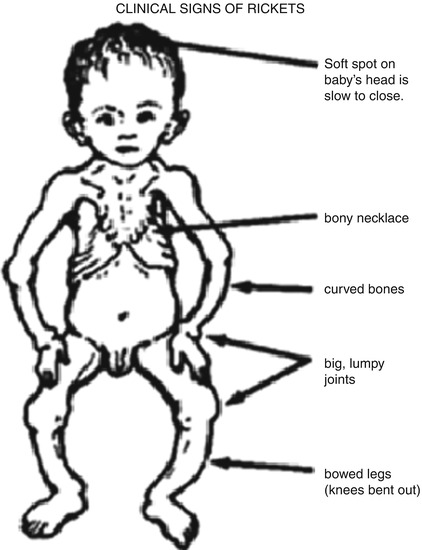
Laboratory
Low calcium, phosphorous, and vitamin D levels
Elevated alkaline phosphate and PTH
Radiography
Anterior view of the knee will show cupping and widening of the metaphyses
Treatment
Vitamin D and calcium supplementation, may need surgical intervention for skeletal deformities
2.9 Osteomalacia
Similar to rickets but occurs in adults
Definition
Incomplete mineralization of osteoid following growth plate closure. Normal amount of collagen, too little calcium.
Not to be confused with osteoporosis, which is a decrease in bone mass with NORMAL mineralization
Causes
Most commonly from vitamin D deficiency.
Can also be caused by celiac disease, anticonvulsants, kidney and liver disease, surgeries that remove part of the stomach or small intestine, low phosphorous intake, and cancer
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






