WILLIAM G. BOISSONNAULT, PT, DHSc, FAAOMPT, FAPTA and DARCY A. UMPHRED, PT, PhD, FAPTA After reading this chapter the student or therapist will be able to: 1. Identify the difference between Differential Diagnosis Phase 1, medical screening, and Phase 2, diagnosis of impairments and functional limitations. 2. Analyze the concept of body system and subsystem screening. 3. Develop a mechanism for body system screening to be used with clients with preexisting neurological dysfunction. 4. Analyze the significance and importance of performing a medical screening for all clients who interact in a therapeutic environment with occupational or physical therapists. 5. Differentiate between direct causation of a clinical symptom as opposed to system causation of a clinical problem. For the professions of physical and occupational therapy the concepts associated with and use of the term differential diagnosis are still evolving and under debate. A recent editorial describes diagnosis in physical therapy as complex and controversial, with diverse views existing.1 For physical therapists (PTs), the guiding premise is that the differential diagnostic process fits within the Patient/Client Management Model described in the Guide to Physical Therapist Practice2 (Figure 7-1) and within The Guide to Occupational Therapy Practice.3 The therapist attempts to organize the history and physical examination (including tests and measures) findings into clusters, syndromes, or categories. There are certain clusters of findings that suggest the presence of disease or an adverse drug event and warrant communication with a physician. There are other symptoms and signs that are consistent with conditions that still fit into the older disablement framework. In the world today, the model of choice of all therapists is the World Health Organization (WHO) International Classification of Functioning, Disability and Health (ICF), which moves away from the consequences of disease classification to a health focus classification. Thus a shift in how one looks at disease and its impact on health and wellness not only has changed the words used by therapists but also incorporates external societal limitations that our clients face.4 These changes do not affect the way a therapist should medically screen before formulating a clinical diagnoses based on movement dysfunction. These conditions are inherent in the interrelationships among impairments, functional or activity limitations, and participation in life and are appropriate for physical or occupational therapy interventions.2,3,5,6 The process of differentiating the cluster of findings that warrant communication with a physician regarding concerns about a patient’s health status compared with those that do not will be called Differential Diagnosis Phase 1.7 In this scenario a physician will ultimately diagnose the patient’s illness, but the PT’s and occupational therapist’s (OT’s) examination findings and subsequent patient referral contribute to the diagnosis being generated. For many of these illnesses, the use of advanced imaging, laboratory testing, and/or tissue biopsy is necessary for the diagnosis to be made.8 Numerous examples exist in Physical Therapy Journal and Journal of Orthopaedic and Sports Physical Therapy of published case reports and case series describing such action taken by PTs. If the decision is reached that the symptoms and signs do fall within the scope of practice of PTs and OTs, a second level of differential diagnosis occurs. Now the therapist attempts to categorize the examination findings into the specific diagnostic categories that will specifically guide the choice of treatment interventions and the development of a prognosis. This second level of diagnosis is called Differential Diagnosis Phase 27 and is the focus of Chapters 8 and 9. Figure 7-2 illustrates where Differential Diagnosis Phase 1 and Phase 2 fit into the Patient/Client Management Model. The Guide to Physical Therapy Practice2,9 and The Guide to Occupational Therapy Practice3 clearly describe the therapists’ responsibility to refer patients/clients with health concerns to other practitioners. The emphasis of the following discussion is detecting clinical manifestations that suggest the specific need for physician intervention. Typically the initial warning signs associated with these scenarios include a recent onset or exacerbation of symptoms such as pain, weakness, numbness, dizziness, falls, confusion, and so on—common complaints of patients with neurological disorders. Therapists may also detect symptoms or signs unrelated to the primary medical neurological condition but that could be related to an existing comorbidity or a medication side effect. In addition, a general health and wellness screen may reveal a need for a psychological, dermatological, or other nonneurological medical consultation. The purpose of the therapist’s medical screening is to (1) identify existing medical conditions, (2) identify symptoms and signs suggesting that an existing medical condition may be worsening, (3) identify neurological manifestations that suggest an acute or life-threatening crisis, and (4) identify symptoms and signs suggestive of the presence of an occult disorder or medication side effect. This medical screening has always taken place within the clinical framework of PTs’ and OTs’ practices, but as practitioners become more autonomous, this screening must become more comprehensive, requiring tools and documented evaluation results. Figure 7-3 is an example of an examination scheme leading to the decision to treat the patient, to treat and refer the patient, or to refer the patient. Phase 2 may also include the decision to refer the patient to another practitioner (e.g., dietician, social worker, clinical psychologist) for services augmenting the therapy or to social programs such as wellness clinics that will encourage the patient to participate in movement activities even though he may need individualized therapeutic intervention. The following material focuses on the components of this scheme most directly related to the medical screening process leading to a patient referral. Of these, a personal history of a current or recent medical condition, current medication use, and a positive family history (e.g., mother and aunt with a history of breast cancer, father diagnosed with prostate cancer at the age of 58 years) are the most relevant risk factors for the potential presence of an occult condition. For example, the history of a previous episode of depression significantly increases the risk of a second episode compared with the risk that someone who has never had an episode of depression will have his or her first such episode.10 The greater the number of existing risk factors, the more vigilant the therapist should be for the presence of warning signs suggestive of disease and the more extensive the other medical screening components will need to be. Those increased risk factors, whether within one system or multiple systems, can lead to clinical behaviors that are the summation of the systems problems and their interactions that affect movement. Physicians should be able to depend on the therapist to recognize these interactive symptoms and refer the patient back to either the referring physician or to another specialist. There are different methods to collect this medical history and patient profile information, including a review of the medical record and use of a self-administered questionnaire, depending on the practice setting and patient population. Figure 7-4 is an example of a self-administered questionnaire that could be completed by the adult patient, a family member, or a caregiver. As noted in Figure 7-3, a quick scanning review of this information should occur, if possible, before the patient interview is begun. The therapist will have a head start in organizing the history and physical examination, knowing what to prioritize and at least initially what parts of the examination can be deemphasized. The utility and accuracy of a self-administered questionnaire in patient populations germane to therapists’ practice, similar to the one illustrated in Figure 7-4, have been described, with the conclusion that such a tool can be a valuable adjunct to the oral patient interview.11 Affirmative answers to previous or current illness questions should direct the therapist to consider what the potential impact may be on the patient’s symptoms, choice of examination and treatment techniques, rehabilitation potential, and risk for additional illness. For example, the presence of existing chronic kidney disease (e.g., renal failure) should alert the therapist to numerous potential complications including patient fatigue, weakness, and impaired concentration, all of which could interfere with rehabilitation efforts. Chronic renal failure is also marked by paresthesia and muscle weakness, which could mistakenly be associated with other neurological conditions. Renal osteodystrophy is yet another complication associated with chronic renal failure. The concern of compromised bone density should direct the therapist to use techniques that carry a reduced risk of skeletal injury. A series of follow-up questions for the affirmative answers will assist the therapist in determining the relevance (if any) of each item (see Figure 7-5 for examples of follow-up questions for selected information categories). The chief presenting symptoms or functional restriction typically provides the reason for therapy services being sought and can provide the initial warning sign(s) of potential medical issues needing to be addressed. Despite pain not typically being the chief complaint of many patients with primary neurological conditions, a relatively mild pain is often the initial complaint associated with a serious pathological condition; a dull diffuse ache is often the initial presenting complaint associated with tumors of the musculoskeletal (MSK) system.12 This relatively minor complaint can easily be overlooked by therapists working with patients who have neurological involvement and signs and symptoms (e.g., weakness, numbness) that are much more debilitating and cause more functional limitations than the pain complaints do. Although investigating pain complaints may not be the initial priority for these therapists, at a later visit such questioning is very important, especially if it continues, increases in intensity, shifts, or enlarges its region with no causation. Effective medical screening involves the interpretation of a patient’s description of symptoms, functional limitations, and the corresponding physical examination findings. Descriptions of symptoms associated with neuromusculoskeletal impairments (loss or abnormality of physiological, psychological, or anatomical structure or function) generally reveal a fairly consistent and predictable pattern of onset and change over a defined period of time. In addition, the neurological and MSK impairments noted during the physical examination should match with the functional limitations described by the patient or the caregiver. If these expectations are not met, it does not necessarily mean the patient has cancer or an infection, but doubt should be raised on the therapist’s part whether therapy is indicated. A body diagram can be a valuable tool to document the location of symptoms expressed verbally or nonverbally by patients with identified neurological deficits. Besides pain and altered sensation, patterns of abnormal tone, asymmetrical posturing, and areas of weakness can also be noted on the body diagram (Figure 7-6). Numerous body structures are potential pain generators, including visceral structures. Figure 7-7 and Table 7-1 illustrate local and referred pain patterns from various visceral organs. Although the presented pain patterns illustrate those most commonly noted, clinicians should be aware of other potential patterns. For example, ischemic heart disease—the complaint of left chest wall and left upper extremity pain, pressure, or tightness—is not the classic presentation for women and many of the elderly. Besides what is noted in Figure 7-7 and Table 7-1, pain from the heart can also be experienced in the right shoulder or biceps, jaw and tooth, epigastric, and interscapular regions.13,13a TABLE 7-1 Modified from Boissonnault WG, Bass C: Pathological origins of trunk and neck pain, I. Pelvic and abdominal visceral disorders. J Orthop Sports Phys Ther 12:192–207, 1990, with permission of the Orthopaedic and Sports Sections of the American Physical Therapy Association. Because there is so much overlap between pain locations associated with visceral disease and neuromusculoskeletal conditions, the results obtained in and of themselves have minimal use in differentiating MSK from non-MSK conditions. Being familiar with the visceral pain patterns will be extremely important, however, when deciding which body systems to screen during the review of systems. Besides noting where symptoms are located, it is equally important to document areas of no complaints (see Figure 7-6). Once the patient has reported symptoms (e.g., low back and right buttock aching, see Figure 7-6), therapists should clarify. Screening to eliminate the possibility of symptoms being present down the back and up the front of the legs; in the pelvis, stomach, chest, neck and face areas; or between the shoulder blades and in the arms is critical. If there is one body area so involved that all the patient’s and practitioner’s attention is focused on it, a relatively mild but potentially serious symptom may be overlooked elsewhere. Placing a checkmark over each body region devoid of symptoms or other abnormal findings is one way to document such information and record change over time. Aspects of the patient’s chief complaint other than symptom location are very relevant to the process of differential diagnosis, in particular a description of how and when the symptoms changed over a defined period of time. Complaints of pain, paresthesia, and numbness associated with primary MSK conditions typically change in a consistent manner over a 24-hour period. The patient will report that the symptom intensity increases with the assumption of specific postures such as left side lying or sitting or with specific activities such as walking, driving, or 2 hours of computer work. Conversely, patients typically can relate paresthesia or pain relief with avoiding certain postures or activities, the assumption of certain postures, wearing an arm sling, and so on. Night pain investigation also falls under this subcategory of patient data. Pain that wakes an individual from sleep and for which changing positions in bed does not provide relief is more concerning than if the pain is positionally related. If the pattern of symptom aggravation and alleviation is that there is no consistent pattern, such as pain that comes and goes independently of the patient’s posture, activities, or time of day; night pain is the patient’s most intense pain; or paresthesia or pain moves from one body region to another inconsistently with common pain referral patterns or identified medical conditions, then the therapist should start thinking whether physical or occupational therapy is what the patient truly needs.14
Differential diagnosis phase 1: medical screening by the therapist
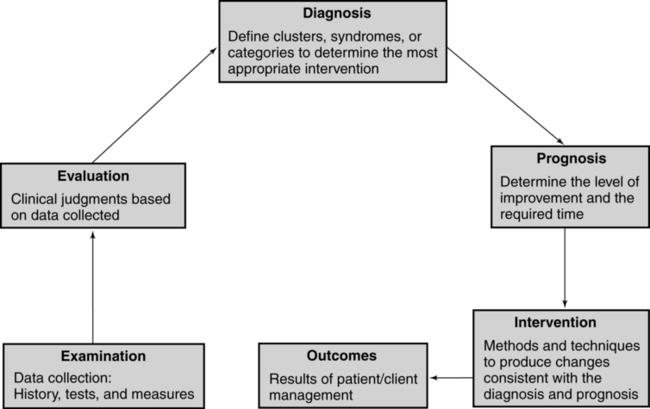
 Patient/client management model. (Adapted from American Physical Therapy Association: Guide to physical therapist practice. Phys Ther 81:43, 2001, with permission of the American Physical Therapy Association.)
Patient/client management model. (Adapted from American Physical Therapy Association: Guide to physical therapist practice. Phys Ther 81:43, 2001, with permission of the American Physical Therapy Association.)

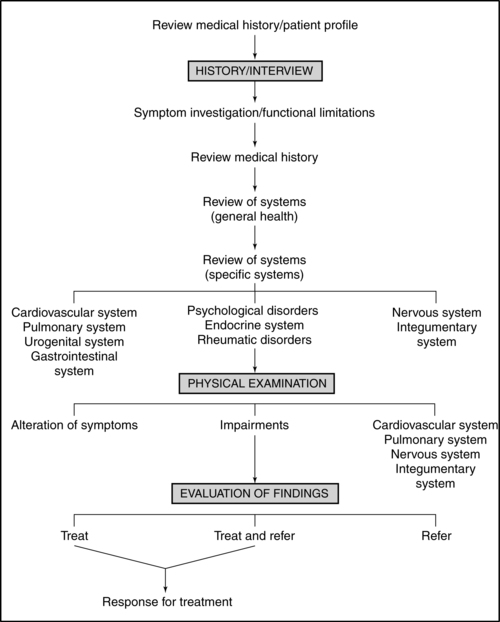
 Patient/client management model showing Differential Diagnosis Phase 1 and Phase 2. (Modified from Umphred DA [Chair]: Diagnostic Task Force, State of California, 1996–2000, California Chapter of American Physical Therapy Association.)
Patient/client management model showing Differential Diagnosis Phase 1 and Phase 2. (Modified from Umphred DA [Chair]: Diagnostic Task Force, State of California, 1996–2000, California Chapter of American Physical Therapy Association.)
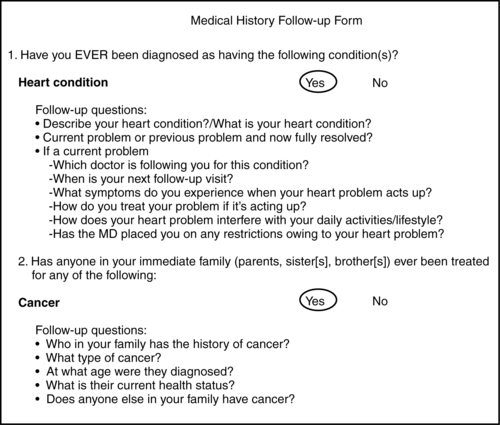
Differential diagnosis phase 1: medical screening
Identifying patients’ health risk factors and previous conditions
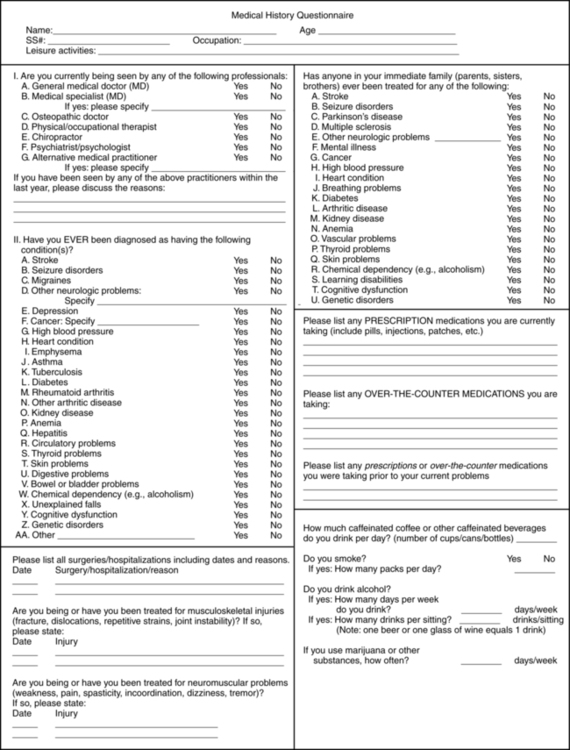
 Self-administered questionnaire to collect medical history information. (Modified from Boissonnault WG, Koopmeiners MB: Medical history profile: orthopaedic physical therapy outpatients. J Orthop Sports Phys Ther 20:2–10, 1994, with permission of the Orthopaedic and Sports Sections of the American Physical Therapy Association.)
Self-administered questionnaire to collect medical history information. (Modified from Boissonnault WG, Koopmeiners MB: Medical history profile: orthopaedic physical therapy outpatients. J Orthop Sports Phys Ther 20:2–10, 1994, with permission of the Orthopaedic and Sports Sections of the American Physical Therapy Association.)
Symptomatic investigation of functional restriction
Location of symptoms

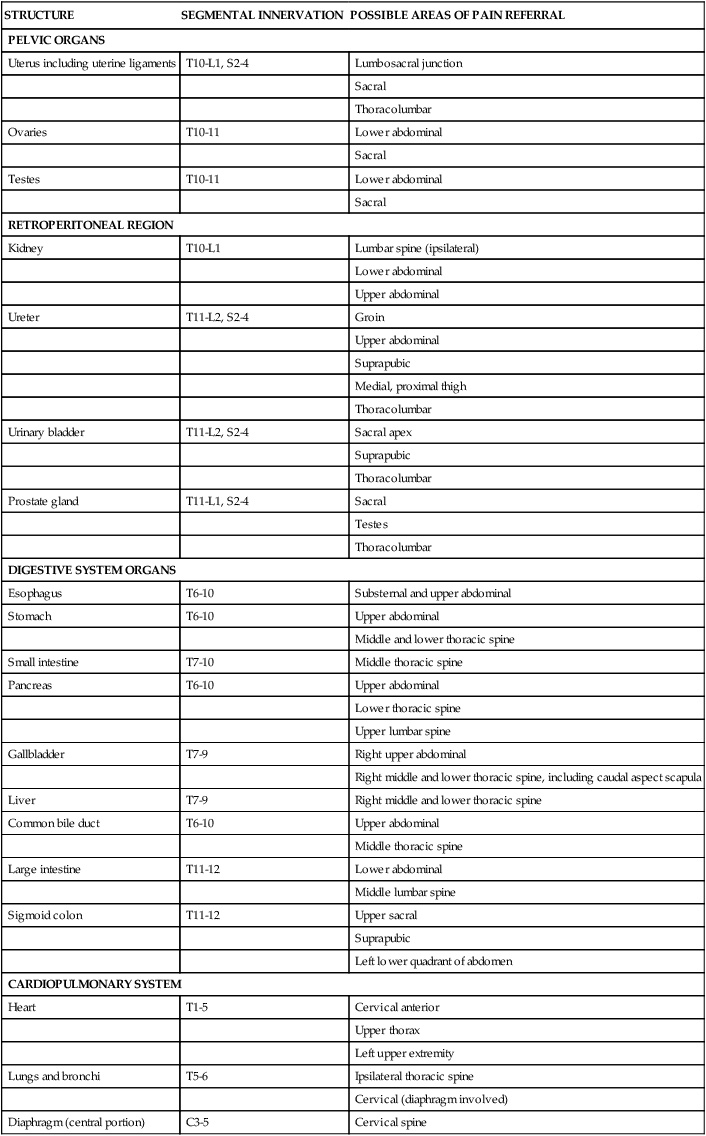
STRUCTURE
SEGMENTAL INNERVATION
POSSIBLE AREAS OF PAIN REFERRAL
PELVIC ORGANS
Uterus including uterine ligaments
T10-L1, S2-4
Lumbosacral junction
Sacral
Thoracolumbar
Ovaries
T10-11
Lower abdominal
Sacral
Testes
T10-11
Lower abdominal
Sacral
RETROPERITONEAL REGION
Kidney
T10-L1
Lumbar spine (ipsilateral)
Lower abdominal
Upper abdominal
Ureter
T11-L2, S2-4
Groin
Upper abdominal
Suprapubic
Medial, proximal thigh
Thoracolumbar
Urinary bladder
T11-L2, S2-4
Sacral apex
Suprapubic
Thoracolumbar
Prostate gland
T11-L1, S2-4
Sacral
Testes
Thoracolumbar
DIGESTIVE SYSTEM ORGANS
Esophagus
T6-10
Substernal and upper abdominal
Stomach
T6-10
Upper abdominal
Middle and lower thoracic spine
Small intestine
T7-10
Middle thoracic spine
Pancreas
T6-10
Upper abdominal
Lower thoracic spine
Upper lumbar spine
Gallbladder
T7-9
Right upper abdominal
Right middle and lower thoracic spine, including caudal aspect scapula
Liver
T7-9
Right middle and lower thoracic spine
Common bile duct
T6-10
Upper abdominal
Middle thoracic spine
Large intestine
T11-12
Lower abdominal
Middle lumbar spine
Sigmoid colon
T11-12
Upper sacral
Suprapubic
Left lower quadrant of abdomen
CARDIOPULMONARY SYSTEM
Heart
T1-5
Cervical anterior
Upper thorax
Left upper extremity
Lungs and bronchi
T5-6
Ipsilateral thoracic spine
Cervical (diaphragm involved)
Diaphragm (central portion)
C3-5
Cervical spine
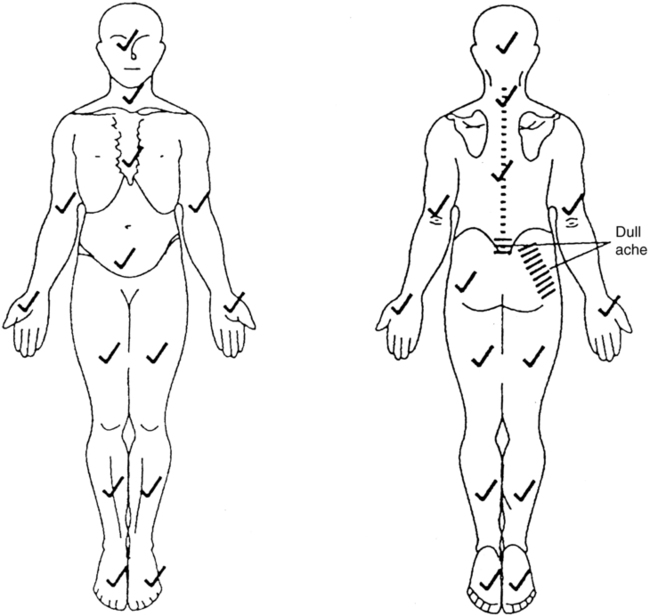
 Body diagram illustrating symptom location. Body areas with no known symptoms or abnormalities are marked with a checkmark. (From Boissonnault WG, editor: Examination in physical therapy practice—screening for medical disease, ed 2, New York, 1995, Churchill Livingstone.)
Body diagram illustrating symptom location. Body areas with no known symptoms or abnormalities are marked with a checkmark. (From Boissonnault WG, editor: Examination in physical therapy practice—screening for medical disease, ed 2, New York, 1995, Churchill Livingstone.)
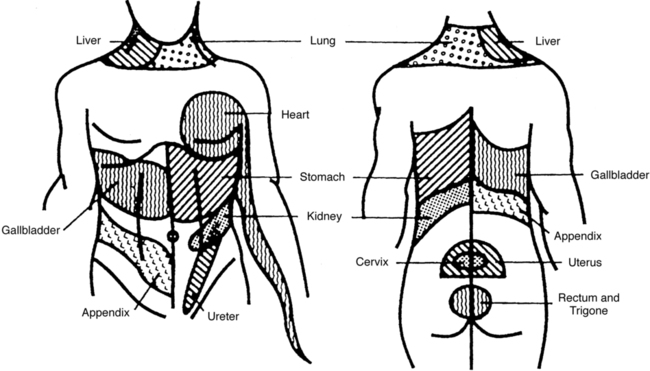
 Possible local and referred pain patterns of visceral structures. (From Boissonnault WG, editor: Examination in physical therapy practice—screening for medical disease, ed 2, New York, 1995, Churchill Livingstone.)
Possible local and referred pain patterns of visceral structures. (From Boissonnault WG, editor: Examination in physical therapy practice—screening for medical disease, ed 2, New York, 1995, Churchill Livingstone.)
Symptom pattern
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Differential diagnosis phase 1: medical screening by the therapist
Only gold members can continue reading. Log In or Register to continue