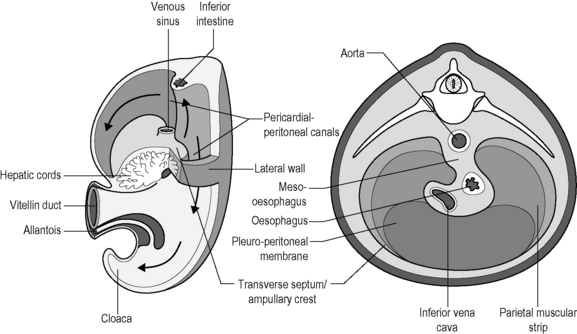
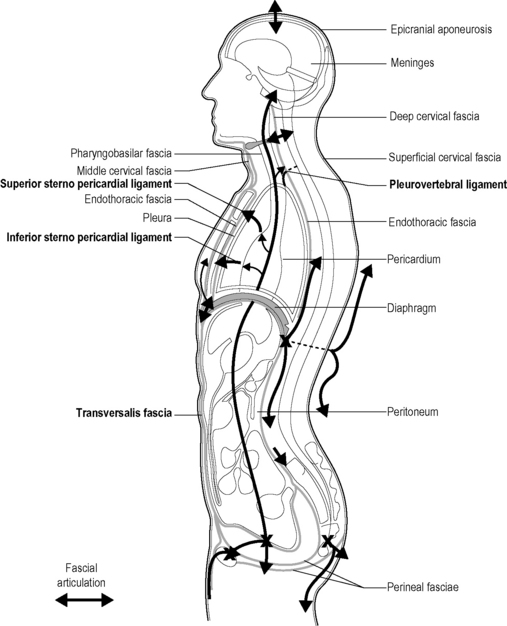
1.10 Diaphragmatic structures In week 4 we see the appearance in the embryo of three sections, which will divide the body cavity into the pleural, pericardial, and peritoneal cavities. The first to form is a horizontal layer: the transverse septum of our future diaphragm. It divides the body cavity into a primitive pericardial cavity, the future chest, and in the peritoneal cavity, the future abdomen (see Fig. 1.10.1). The frontal pleuropericardial folds appear on the lateral wall of the primitive pericardial cavity and grow in a medial direction to unite with each other, as well as with the anterior facet of the mesoblast of the anterior intestine to form the definitive pericardial cavity and the pleural cavities. The muscle fibers participate in the formation of the lower part of the esophagus (Botros et al. 1983). Note that these two cavities initially communicate with the peritoneal cavity through the pleuroperitoneal canals passing behind the transverse septum/ampullary crest. At this stage there is fascial continuity between the chest and the abdomen. Thereafter, a pair of transverse pleuroperitoneal membranes develops in an anterior direction to join with the transverse septum/ampullary crest and form with this the definitive diaphragm which closes the pleuroperitoneal canals in the 7th week (Greer et al. 2000). The left pleuropericardial canal is wider than the right one and closes later. The mesenchyme associated with the anterior intestine contracts to form the right and left crura. This closure does not constitute an interruption between the thoracic and abdominal cavities; the diaphragm merely represents an intermediary point between the pleuropericardial and abdominal structures. This continuity is an important element in the transmission of forces and pressures between the regions above and below the diaphragm, particularly during movement of the diaphragm. During embryonic development, the nonclosure of the pleuroperitoneal canals is the cause of congenital diaphragmatic hernias, which have a frequency of 1/2000 to 1/4000 births. This nonclosure is more often partial than total and the left side is more often affected than the right, in a proportion of four to eight times, probably because the right cavity is wider, closes later, and contains the liver, the capsule of which is dependent on the diaphragm. Genetic factors also play a part in diaphragmatic hernias (Holder et al. 2007). Three parts can be distinguished at the level of the diaphragm (see Fig. 1.10.2). It is formed from two types of fibers arranged in three groups (Menck et al. 1990): fundamental fibers directed sagittally in the anterior leaflet, oblique fibers in the lateral leaflets, as well as the connecting inferior and superior semicircular bands. As they cross, they circumscribe a nonstretchable fibrous opening for the passage of the inferior vena cava. This multidirectional, multilayered conformation reinforces the diaphragm’s strength and distributes the forces over the whole surrounding area to reduce the exertion of the vertical components on the abdominal mass. The fibers of the central tendon are made up of three groups. This part is formed by the crura of the diaphragm and the arcuate ligaments. The other one is the lateral arcuate ligament or lumbocostal arch: This extends from the transverse apophysis of L1 to the apex of the 11th and 12th ribs. It matches the aponeurosis of the transverse and forms a fascial continuation with the abdomen via the transversalis fascia, which itself continues along the pelvic fascia (Lierse 1990). It constitutes the costolumbar hiatus.
Embryology
Organization
Central part
Posterior part
The two arcuate ligaments
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Diaphragmatic structures