2.7 Diagnosis, Evaluation, and Treatment of Reflex Incontinence
 Diagnosis and Evaluation
Diagnosis and Evaluation
The goal is to identify dysfunctions (inhibiting factors) in the motor system. The need to protect such factors leads the central nervous system to limit activity of the pelvic floor muscles. This analysis will include dysfunctions derived from the patient’s general history.
 Functional History
Functional History
The functional history is the general analysis of current daily activities, which has the goal of discovering causes of dysfunction (maladaptive or excessive stresses) in daily activities (work, sport, hobbies, home). The analysis includes four types of function:
- Quantitative analysis of function: how often are certain positions, movements, and functions carried out?
- Qualitative analysis of functions: are the actual movements:
- – Monotonous and static?
- – Monotonous and dynamic?
- – Dynamic and varied?
- – Monotonous and static?
- Which function dominates: quantitative and qualitative analysis reveal:
- – Which functions are used predominantly.
- – Where functional contractures and stress edema originate.
- – Which functions are used predominantly.
- Limitations of function: which movements or functions are impaired subjectively and/or objectively, and in what way?
Example case
Mrs. F. Computer specialist, aged 57, married, 2 children (normal births), right-handed.
Medical diagnosis: Stress incontinence with painful pelvic floor hypertony.
Secondary diagnoses: Pain in the left sacroiliac joint; aching pain radiating into the left buttock; pain in the left hip and the proximal external surface of the thigh on getting out of a car; pain in the lumbar spine; pain between the shoulder blades.
Quantitative assessment of activities sits 90 % of time at work; sits driving to work; bicycles ca. three times a week for about 1.5 h; works on computer at home about 2 h/day; reads about 1 h/day, sitting in strain posture; housework ca. 2 h/day; stands or moves in small steps in strain posture.
Qualitative assessment of activities
- Work: 80 % monotonous and static: includes 70 % computer, 10 % typewriter and 20 % handwriting; 10% monotonous and dynamic (moving in a very small space); 10% varied dynamic.
- Household: varied and dynamic in strain posture.
- Leisure/computer: monotonous and static in strain posture.
- Leisure/bicycling: monotonous and dynamic in strain posture.
- Leisure/reading: monotonous and static in strain posture.
Assessment of predominant function (assessment of limitation); (– reduced, – – moderately reduced, – – – severely reduced; + mildly, ++ moderately, +++ considerably increased from the norm).
Trunk, most prominent deviations:
- Pelvis: upright (dorsal torsion), (–) rotation
- Thorax: descent, (–) rotation
- Cervical spine/head: Backward tilt of the atlanto-occipital joint with ventral translation, marked lordosis of the cervical spine and (+) rotation of the head.
Upper extremities:
- Flexion (finger, hand, elbow, shoulder): right more than left
- Thumb and fifth finger opposition: right more than left
- Internal rotation/abduction (shoulder): right more than left
- Abduction/elevation /internal rotation (scapula): right more than left
Lower extremities:
- Plantar flexion supination/internal rotation (foot): left more than right
- Flexion/internal rotation (knee) left more than right
- Flexion/adduction/internal rotation (hip): left more than right
Limitation of function (assessment of disability)
- Urinary incontinence when using stairs (especially going down) and when lifting moderately heavy loads (shopping bags, grandchildren).
- Painful fatigue between the shoulder blades, beginning about noon and increasing toward evening (strain-dependent pain).
- Sacroiliac pain is present daily, fairly constant, but can increase during lifting.
- Almost daily, deep lumbar pain (painful stiffness), with some radiation into the buttocks, especially when getting up in the morning.
Handicap: Patient cannot do her work full time. She feels insecure at social events and avoids them. The patient cannot lift her grandchildren and has difficulty hiking and bicycling.
Analysis of the patient’s history
- Functional disorder of the motor system due to misdirected effort and poor posture.
- Excessive strain due to monotonous sitting in strain posture without adequate compensation during leisure activities; on the contrary, the latter sustain the strain posture adopted at work.
- Monotonous activities of the extremities with marked flexion components.
- Functional disorders of the extremities and the trunk lead to a centrally maintained hypertonus of the pelvic floor, and this in turn leads to incontinence.
 Inspection/Evaluation
Inspection/Evaluation
Findings on inspection determine transitory (e. g., constricting clothing and shoes, poor seating furniture), persistent (e. g., surgical scars, injuries) and infrastructural (e. g., malperfusion, edema formation, edema due to stress) disturbing factors, which need to be addressed during treatment.
Example case
Mrs. F. Transitory disorders
- Cotton body stocking too short, prevents extension of the spine.
- Pants have constricting waistband and too narrow legs: backward torsion of pelvis with corresponding flexed position of the trunk; adducted hips.
- Shoes with high heels and shoes with rigid soles: feet in plantar flexion and supination position.
Persistent disturbing factors
- Edema due to overuse, especially between the shoulder blades and in the thenar and hypothenar areas and in the areas of all the functional contractures.
Analysis of the inspection findings
- The transitory disturbing factors promote the strain posture or inhibit upright body posture.
- The persistent disturbing factors express and maintain a chronic faulty strain on the motor system and its infrastructural functioning (see also section 1.3).
General Functional Diagnosis
General functional diagnosis consists of the evaluation of habitual and corrected motor behavior and its comparison with the physiological norm. This type of comparison leads to an initial prognosis of the extent of the functional disorders.
Analysis of Habitual Postural and Movement Programs
To what extent do posture (lying, sitting, standing) and movement (gait, transfer movements such as bending down, for example, specific movement programs such as writing or grasping, for example) deviate from movement when upright?
The evaluation concerns the degree of strain posture (+ mildly, ++moderately, +++ considerably increased from the norm).
Example case
Mrs. F. Evaluation of habitual sitting, since this is the position she adopts predominantly.
- Pelvic extension ++(+)
- Thoracic descent +++
- Reclining +(+), cervical spine lordosis ++(+), ventral translation of the cervical spine and head ++(+)
Analysis of the Corrected Posture and the Resulting Movement Programs
How well can the posture be corrected? The evaluation compares the deficit to the normal upright posture with Brügger thoracolumbar lordosis (— mildly reduced, – – moderately reduced, -– – severely reduced from the norm). How are the movement programs changed?
Example case
Mrs. F. Initial position: corrected sitting position with arms hanging down.
Trunk
- Pelvis: flexed (tilted): – (-), (-) rotation
- Thorax elevated: – –(-)
- Inclination: – , extension of cervical spine: -, posterior translation of cervical spine: –
- Most prominent feature: lack of thoracic elevation
- Most prominent feature of lower extremity: plantar flexion/supination of left foot
- Most prominent feature of upper extremity: position of thumb-fifth finger opposition in the right hand.
Analysis of corrected upright sitting position
- Predominant functions from normal are more marked in the extremities than in the trunk (extremity dominance).
- Deviations in the trunk are primarily elicited by activity of the extremities.
- More prominent disturbing factors originate in the upper extremities than in the lower.
- Hierarchy of the disturbing factors: right thumb-fifth finger opposition before left plantar flexion/supination, before thoracic descent.
Function Tests
Function tests are carried out while the patient is sitting, standing or moving. Tests performed with the patient lying down are only used to supplement these, since they do not involve straightening against gravity and therefore their results have little relevance to everyday activities. Tests performed while the patient is supine are therefore not suitable for task-related and context-specific therapy. Which function tests are selected depends on the actual questions raised.
The same function test should be used throughout therapy as a constant parameter.
T5 rocking [Brügger 1996a]. T5 rocking is a functional test that is carried out with the patient in the corrected upright sitting position. In sequence, the following three test are applied:
- Mobility/stiffness of the spine
- Ability to pelvic tilt
- Ability to lift the thorax and reposition the shoulders
Beginning below T5, segmental movement impulses into extension are applied in order to test the way in which the impulse is received and the way in which it continues down to the sacrum. It is important not to block the movement by preventing the patient from moving or by making the patient feel insecure.
The following diagnostic questions arise:
- How well and where does spinal extension/ lordosis occur?
- In which spinal section are the compensatory movements for deficits?
- How does the movement impulse continue (extend) into the trunk and extremities?
- Are inhibiting impulses originating from the trunk transmitted to the extremities, or do the extremities block movement impulses reaching the trunk?
- Are the disturbing factors coming from the optical system (how is the test carried out with the eyes open, closed, or wearing glasses)?
- How prominent is the extensor deficit in the upright posture?
- Does the test cause pain or elicit symptoms?
T5 rocking is an ideal function test, which assesses posture-specific changes in the mobility of the trunk (spine, pelvis, thorax, head) and their interaction with the extremities. This assessment allows conclusions to be drawn about the functionality of the transversus abdominis, and with it that of the muscles of the pelvic floor.
Example case
Mrs. F. Test for spinal rigidity: The spine shows slight mobility confined to the junction of the lower thoracic spine and the upper lumbar spine. The remaining spine is rigid.
Test for pelvic tilt: The pelvis moves minimally. Contact with the tuberosities is barely attained.
Test for elevation of the thorax with shoulder retropositioning: Elevation of the thorax with shoulder retropositioning is blocked.
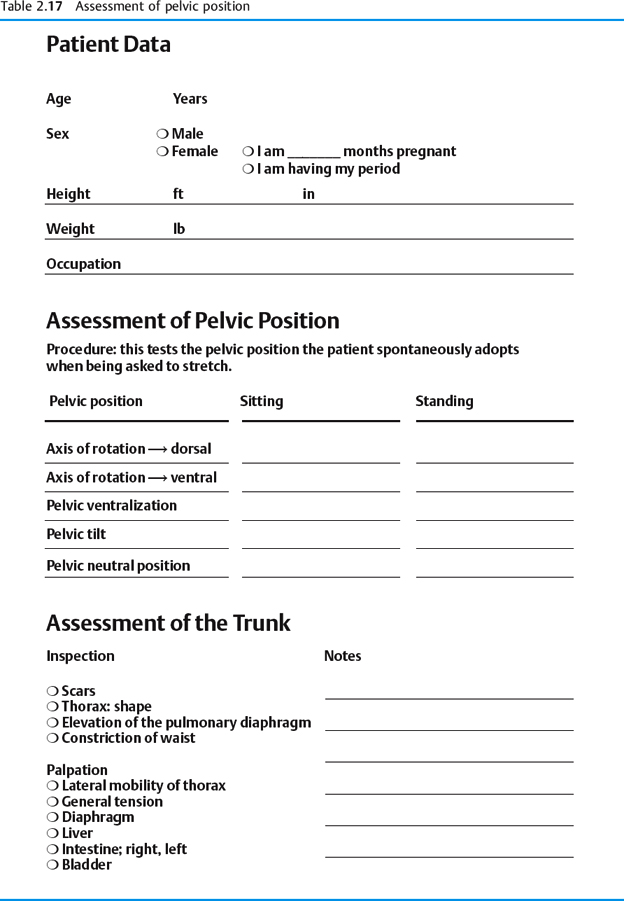
Assessment of pelvic position. The position of the pelvis directly influences the quality and quantity of the activities of the transversus abdominis and the muscles of the pelvic floor (see section 1.6) (Table 2.17).
Consequently deviations of the position of the pelvis from the physiological position, in which the pelvis is tilted slightly anteriorly, allow conclusions to be drawn about functional disorders in the pelvic floor.
The assessment addresses the position of the pelvis and its center of movement during sitting and standing.
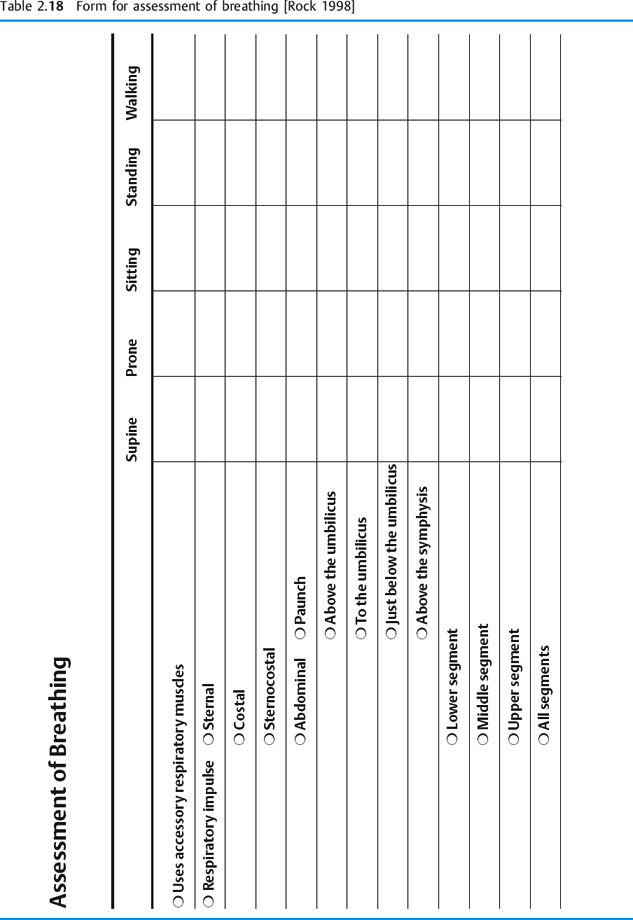
Assessment of breathing. The site of the primary breathing impulse and the spread of each breath are assessed (Table 2.18).
Since the pulmonary diaphragm is closely linked to the transversus abdominis (see sections 1.6 and 1.5), assessment of breathing can indicate disorders in the functioning of the pulmonary diaphragm and the transversus abdominis, hence also reflex functional limitations of the pelvic floor.
Assessment of pelvic floor activity. In prone position, the activity of the pelvic floor is assessed in response to respiration and during voluntary contraction to determine its mid-position, its response to pain, its strength, and the direction in which it moves.
 Example case
Example case
Mrs. F. (Table 2.19)
- The left side of the pelvic floor shows little movement during either eccentric or concentric contraction.
- On the left side, respiratory concentric activity is better than voluntary concentric contraction from mid-position.
- When voluntary contraction begins with expiration, the ability to contract from mid-position diminishes bilaterally.
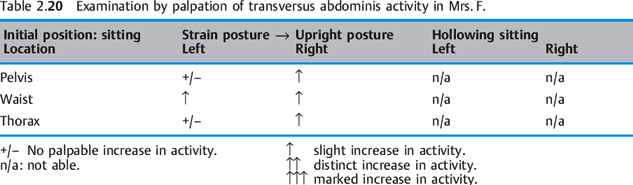
Assessment of transversus activity. Assessment of active contraction of the transversus abdominis when changing from the strain position to the upright position and “hollowing” in corrected position. “Hollowing” refers to gentle drawing in of the abdominal wall while the waist circumference becomes smaller and the distance between the sternum and symphysis pubis remains stable. Hollowing happens reactively while exhaling, when there are no disturbing factors. It also can be done consciously during expiration and can then be held for several seconds.
Example case
Mrs. F. (Table 2.20)
- The left side of the transversus shows slight increase in activity only at the waist.
- On the right side, a slight increase in activity can be felt in all areas.
- Hollowing cannot be performed correctly while sitting.
Special Functional Diagnosis
For special functional diagnosis, additional diagnostic procedures are selected specifically to address incontinence. Their documentation during initial, interval, and termination testing serves for quality assurance in physiotherapy during the course of treatment for incontinence.
Voiding Diary
Using special forms, the diary documents what the patient drinks and the bladder output for a number of days. The voiding diary also helps determine the type of incontinence.
Example case
Mrs. F. (Table 2.21)
- The patient is drinking enough, but could increase her fluid intake in the afternoon.
- The patient drinks one cup of coffee, and otherwise caffeine-free teas and water at room temperature.
- Urine volume shows normal bladder capacity (400—500 mL).
- Urine volume is greatest in strain posture with higher impact.
Cough—Paper Towel Test
While wearing a paper towel in her panties, the patient coughs with a full bladder, for example, or walks down a set number of stairs. The amount of leakage is determined by the size of the wet spot on the paper towel. If a patient is leaking larger amounts of urine, a pad is used instead of a paper towel and the pad is weighed before and after the test.
| Pelvic floor reaction during respiration Pelvic floor reaction during respiration Inspiration → expiration | Pelvic floor reaction during voluntary contraction | Pelvic floor reaction in voluntary contraction during expiration |
|---|---|---|
| Palpation ↓↓left | Right↑↑concentric↑↑ | Right↑concentric↑↑ |
| Left +/– concentric ↑ | Left +/– concentric ↑ | |
| Mid-position | Mid-position | Mid-position |
| ↓↓↓ right ↓↓ eccentric↑↑ concentric↑↑↑ | Right↑↑ concentric↑↑↑ | |
| ↓↓ left↓ eccentric↑ concentric↑↑ | left↑ concentric↑↑ |
Initial test Mrs. F.; final test Mrs. F. Starting position: corrected prone position +/– no palpable contraction
Eccentric contractions:↓ slight,↓↓distinct, ↓↓↓strong. Concentric contractions:↑slight,↑↑ distinct,↑↑↑strong. Pain (tenderness):↓ mild, ↓↓ moderate,↓↓↓ intense.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree