Chapter 55 Decision Making and Surgical Treatment of Posterior Cruciate Ligament Ruptures
The proper management of injuries to the posterior cruciate ligament (PCL) and other ligaments of the knee involves a series of decisions based on knowledge of diagnosis, reconstruction options and techniques, and rehabilitation concepts.70,76 The clinician must be able to diagnose and treat a spectrum of knee injuries, from an isolated PCL rupture to a combined injury involving other knee ligaments (Box 55-1). This chapter will review the current knowledge of the function of the PCL—both alone and in concert with other ligament systems—that form the basis for the diagnosis of abnormal translations and rotations that result in different types of knee subluxations requiring surgical restoration (Box 55-2). Legitimate controversy exists about the treatment of complete PCL ruptures because of the absence of a true natural history study, short-term clinical results of PCL reconstructions, and lack of randomized controlled trials of sufficient numbers of patients to form conclusions.
Box 55-1 Spectrum of Posterior Cruciate Ligament Injuries
Posterior Cruciate Ligament Rupture Combined With Other Knee Joint Abnormality
Box 55-2
From Noyes FR, Barber-Westin SD: Posterior cruciate ligament: diagnosis, operative techniques, and clinical outcomes. In Noyes FR (ed): Noyes’ knee disorders: surgery, rehabilitation, clinical outcomes, Philadelphia, 2009, Saunders, pp 503–576.
Clinical Effects of Posterior Tibial Subluxation of the Posterior Cruciate Ligament–Deficient Knee
This chapter will also review advances from our center in PCL graft selection and surgical techniques designed to reduce the morbidity of the procedure. There are different surgical approaches available for acute knee injuries, dislocated knees with multiple ligament ruptures, chronic knees, and revision knees. Important decisions must be made regarding the placement of single- and two-strand graft constructs. In addition, differences exist in the postoperative rehabilitation program, depending on the surgical procedure(s) performed.82 A detailed analysis and surgical treatment of other knee disorders that accompany PCL ruptures has been previously published; this chapter represents a synopsis of this work.76
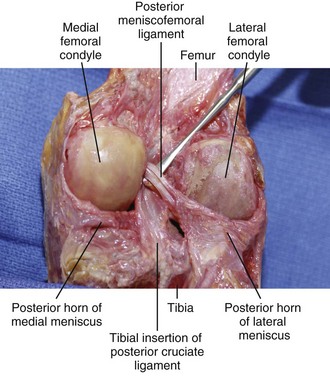
Posterior Cruciate Ligament Anatomy
The PCL arises from a depression posterior to the intra-articular upper surface of the tibia and courses anteromedially behind the ACL to the lateral surface of the medial femoral condyle (Fig. 55-1).122 The PCL has an average length of 38 mm and width of 13 mm.36,131 The cross-sectional area of the PCL varies and increases from tibial to femoral insertions.42 The PCL is approximately 50% larger than the ACL at its femoral origin and 20% larger at its tibial insertion. The anterior meniscofemoral ligament (ligament of Humphry) courses anterior to the PCL, and the posterior meniscofemoral ligament (ligament of Wrisberg) runs obliquely behind the PCL. At least one meniscofemoral ligament is present in 91% of knees, and both ligaments may be found in 50% of knees in young individuals (Box 55-3).41,42,65
Box 55-3
From Noyes FR, Barber-Westin SD: Posterior cruciate ligament: diagnosis, operative techniques, and clinical outcomes. In Noyes FR (ed): Noyes’ knee disorders: Surgery, rehabilitation, clinical outcomes, Philadelphia, 2009, Saunders, pp 503–576.
Meniscofemoral Ligaments
Free nerve endings and mechanoreceptors that are believed to have a proprioceptive function in the knee49 have been identified in the femoral and tibial attachment sites and on the surface of the PCL.47,106
The traditional division of the PCL into separate anterolateral and posteromedial bundles oversimplifies PCL fiber function. The PCL is a complex anatomic structure comprised of a continuum of fibers of different lengths and attachment characteristics. The length-tension behaviors of the fibers that resist posterior tibial translation (with knee flexion) are controlled primarily by femoral attachment regions.* The distal fibers lengthen with increasing knee flexion and the proximal fibers shorten with knee flexion.65,105
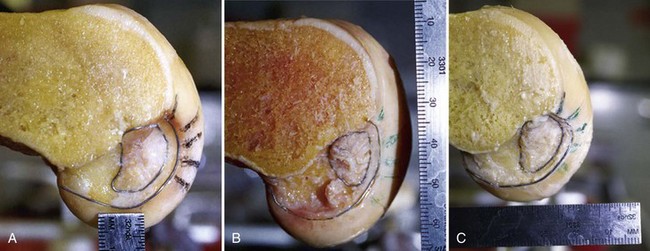
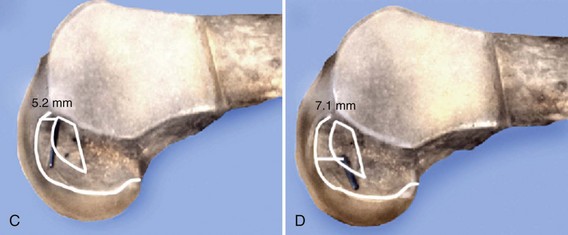
Variation exists among knees in the shape of the PCL femoral attachment, from the common elliptical shape to a more rounded and thicker shape (Fig. 55-2).65 The most accurate measurement system that describes the femoral attachment site uses a clock reference position, with one set of measurement lines perpendicular to the articular cartilage edge and the other set parallel to the femoral shaft.
The distance of the distal edge of the attachment to the articular cartilage margin is 3.2 ± 0.8 mm at the roof, 5.8 ± 2.2 mm at its midportion, and 7.9 ± 2.2 mm at its “lowest” extent.105 The proximal edge of the PCL is usually straight or partially oval, with the attachment tapered in width along its posterior portion.
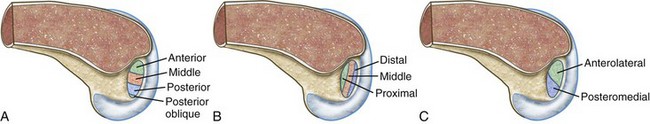
A clear understanding of the anatomy of the native PCL is critical in determining what portion of the ligament will be reconstructed. The terms high, low, shallow, and deep are only general descriptors. Because there may be confusion regarding femoral graft tunnel placement during PCL reconstruction, the PCL femoral attachment is described using the rule of thirds (Fig. 55-3A, B) to define the proximal-middle-distal thirds (deep to shallow in the femoral notch), and anterior-middle-posterior thirds (high to low), with a small posterior oblique portion in the sagittal plane.65,67 This provides a grid for the identification of the tunnel locations for the graft strands and is preferred over the historical division of an anterolateral or posteromedial bundle (see Fig. 55-3C).
Vascular Anatomy and Variations
This normal vascular pattern has been reported to occur in approximately 88% of knees.20,63 In approximately 5% to 7%, the popliteal artery will divide at least 1 inch or more proximal to the distal border of the popliteus muscle.14 In slightly less than half of these knees, with a high division of the popliteal artery, the anterior tibial artery passes anteriorly, not posteriorly, to the popliteus muscle belly.129 A number of variations of the anterior tibial artery were described by Mauro and colleagues.63 Therefore, with a tibial inlay approach, the dissection is always performed proximal to the popliteus muscle using a meticulous technique, because the anterior tibial artery is at risk for transection in approximately 3% to 4% of knees.
An unusual variation in the vascular pattern involves the popliteal artery passing medially and then beneath the medial head of the gastrocnemius. Various subtypes of this abnormal pattern have been described. An abnormal vascular pattern may manifest clinically as the popliteal artery entrapment syndrome, which is characterized by vascular claudication symptoms.52,102,118 Arterial insufficiency occurs most commonly with entrapment of the artery deep to the medial gastrocnemius muscle, but may also occur when the artery is entrapped deep to the popliteus muscle (persistence of ventral component of artery), or entrapped deep to an abnormal accessory head of the gastrocnemius. A history of pain in the lower extremity with activity but none at rest, particularly in a young patient, should alert the surgeon to the possibility that an abnormal vascular pattern may exist. Further evaluation with magnetic resonance imaging (MRI) or angiography may be warranted.30,55
Posterior Cruciate Ligament Fiber Function
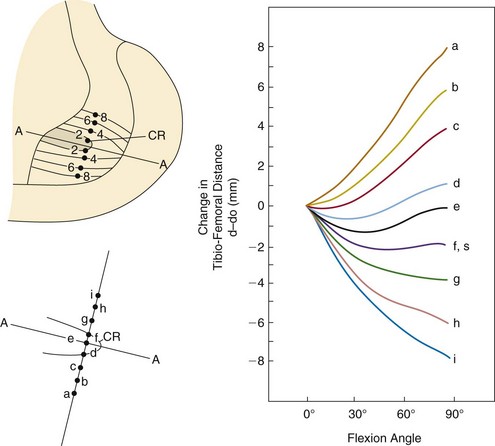
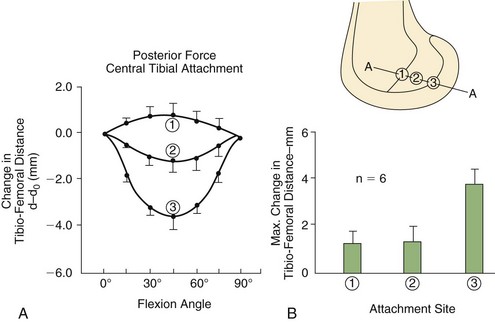
The femoral attachment location of a PCL graft strongly influences graft tension and the ability of the reconstruction to restore posterior stability.* Investigations by Grood and associates38 and Sidles and coworkers115 have demonstrated that the femoral attachment location, and not the tibial attachment location, determines the graft tibiofemoral separation distance with knee flexion-extension.
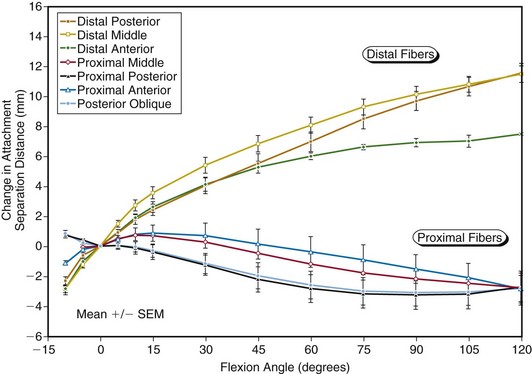
On the femur, the proximal-distal location of a graft has a greater effect on the attachment separation distance than the anterior-posterior location (Figs. 55-4 and 55-5), which forms the basis for the rule of thirds. A graft placed in the distal and middle thirds lengthens with knee flexion, whereas a graft placed in the proximal third lengthens with knee extension.
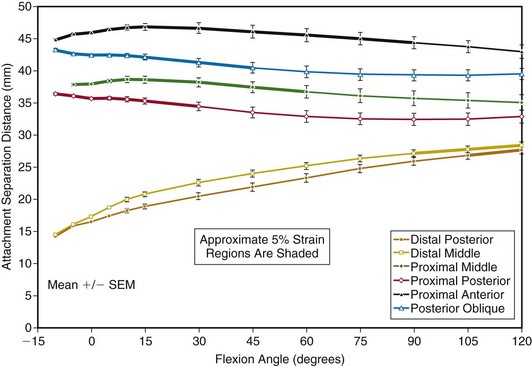
In an investigation at our laboratory,105 the changes in tibiofemoral length for seven peripheral attachment sites at the proximal and distal origins located around the circumference of the PCL femoral attachment were studied. The data confirm that proximal PCL fibers lengthen with knee extension and distal fibers lengthen with knee flexion (Fig. 55-6). In Figure 55-7, the flexion angles in which the fiber length elongations were the least (within 5% of the maximum length and, therefore, the functional zone) are graphed for each attachment point. The data as a whole show a progressive loading of fibers from distal to proximal within the PCL attachment with increasing knee flexion. There is a smaller effect proceeding from anterior to posterior. These data contradict the description of PCL fiber function that divides the PCL into an anterolateral bundle (which lengthen with knee flexion) and posteromedial bundle (which shorten with knee flexion).
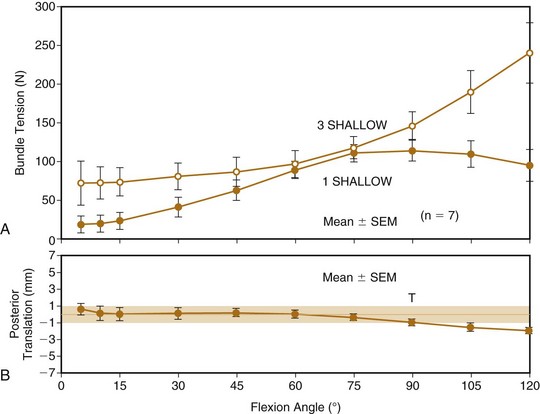
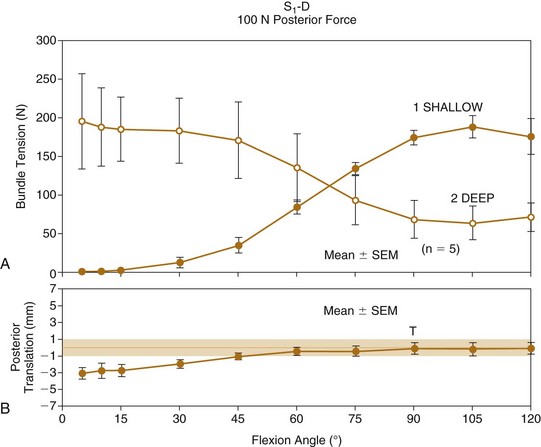
The surgeon has the option of placing a PCL graft strand into different regions of the PCL femoral attachment site that determine the functional range of the graft with knee flexion and the knee flexion position to tension the graft. In a study from our laboratory,57 one- and two-stand PCL reconstructions were attached in three different locations within the PCL femoral footprint. A 50-N posterior force was applied to the tibia for the single-stand construct and a 100-N force was applied to the two-strand PCL reconstruction. The tension in the graft stands was adjusted to restore posterior translation to within ±1 mm of the intact knee. The complex behavior of a two-strand PCL reconstruction is shown in Figure 55-8, in which the two strands were placed into the more distal locations and tensioned at 90 degrees. Both strands shared the applied load as shown. In contrast, a two-strand construct, in which one strand was placed anterior and the second strand was placed more proximally, resulted in a reciprocal loading relationship between strands (Fig. 55-9). In both situations, posterior translation limits were restored to normal.
Another investigation at our laboratory110 confirmed that a proximal to distal change in the femoral position of the second bundle of a two-bundle construct markedly affects bundle tension and function. A middle placement of the second bundle produced load sharing, which is more ideal in terms of graft function in the long term for preventing posterior tibial subluxation with increasing knee flexion. These concepts are used to select PCL graft attachment locations and tensioning, described in the operative techniques section (see later). The surgeon should select graft attachment locations that have the least amount of change in tibiofemoral length, and tension the graft at the knee flexion position at which the graft length is the longest (and therefore functional). If a graft is tensioned at a knee flexion angle at which the tibiofemoral fiber length is at its shortest, the graft will initially constrain knee flexion or extension and fail as the graft (tibiofemoral distance) lengthens with further knee flexion or extension.
Diagnosis of Posterior Cruciate Ligament Function and Knee Joint Subluxations
Posterior Translation
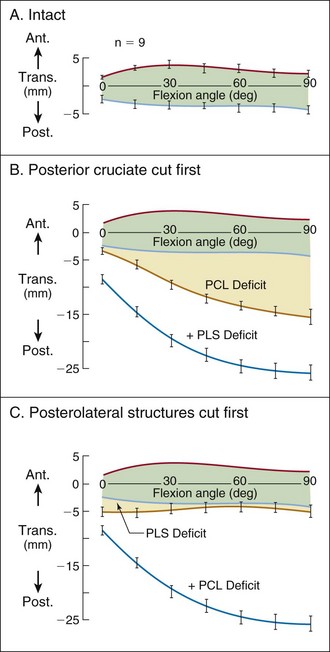
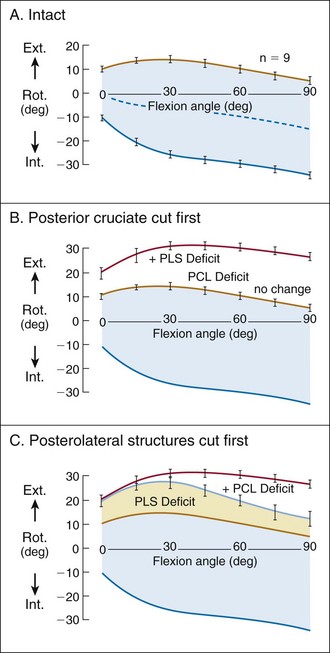
The normal anterior and posterior translation knee limits are shown in Figure 55-10A.40 The increase in these limits when the PCL is cut is shown in Figure 55-10B and the further increase in these limits when the PLS is also sectioned is shown in Figure 55-10C.
The PLS represents one of the most important secondary restraints and has a major effect on lateral tibiofemoral compartment translation. There are marked differences in the amount of posterior tibial translation between isolated and combined PCL injuries. Although the amount of posterior translation may vary among knees,40 it is generally appreciated clinically that a 10-mm or greater abnormal displacement at 90 degrees flexion indicates some deficiency of the secondary restraints in addition to the PCL. Furthermore, the posterior tibial displacement progressively increases at low flexion angles with injury or stretching of the secondary ligament restraints. The abnormal forces placed on the patellofemoral and tibiofemoral compartments are expected to increase as greater posterior tibial displacements occur.116 Clinically, it is advantageous to reconstruct the PCL before the loss of these secondary restraints. Otherwise, the PCL graft is placed under greater forces because the secondary restraints are not able to share a portion of the load in resisting posterior tibial subluxation. In chronic cases, in which the secondary restraints are deficient, we recommend surgical reconstruction of these structures during the PCL reconstruction to allow load sharing and protection of the PCL graft during the healing process. The individual function of each of the posterolateral structures has been previously published.71
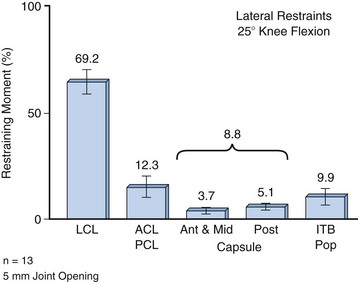
Varus and Valgus Rotations
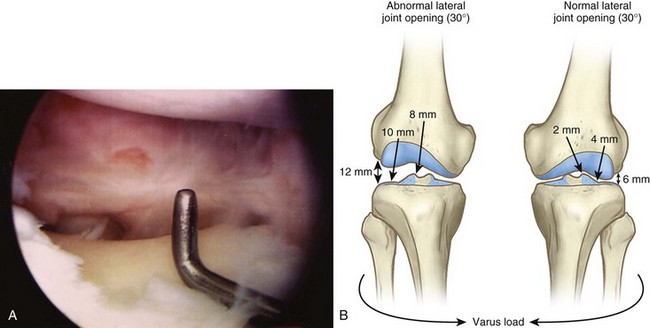
Injury to the fibular collateral ligament (FCL) and posterolateral structures (popliteus muscle–tendon–ligament unit [PMTL], popliteofibular ligament [PFL], and posterolateral capsule) results in increases in lateral joint opening under varus loads and increases in posterior subluxation of the lateral tibial plateau with external tibial rotation. With these ligament injuries, the PCL is placed under higher than normal loading conditions. Figures 55-11 and 55-12 show the relationship of the primary ligamentous restraints to medial and lateral joint opening and the PCL.39 Normally, a small force is present in the PCL to both varus and valgus loads.61 With injury to medial or lateral structures, the PCL and anterior cruciate ligament (ACL) may be placed in the role of a primary restraint that is not ideal, because their mechanical advantage in the center of the knee joint is not suited to resist medial and lateral joint openings. These biomechanical findings indicate the importance of determining an abnormal medial or lateral joint opening (subluxation) that requires surgical reconstruction. The failure to correct such associated subluxations places the PCL graft reconstruction under high in vivo forces postoperatively and risks graft failure.
Careful examination of the knee preoperatively and under anesthesia is required to determine whether abnormal motions and other ligament injuries are present that require reconstruction at the same time as the PCL. During the arthroscopic examination, the gap test confirms that excessive medial or lateral joint opening is not present, which would place abnormal loads on a PCL graft (Fig. 55-13). The goal is to restore function of any insufficient ligamentous structure in one surgical setting. Both the ACL and PCL function in combination with the medial and lateral ligamentous structures in a complex system of primary and secondary restraints that establish the limits to rotations and translations that normally occur in the knee joint. Any insufficiency of two ligamentous structures results in a combination of subluxations involving the medial and lateral tibiofemoral compartments (see later).
Tibiofemoral Rotational Subluxations
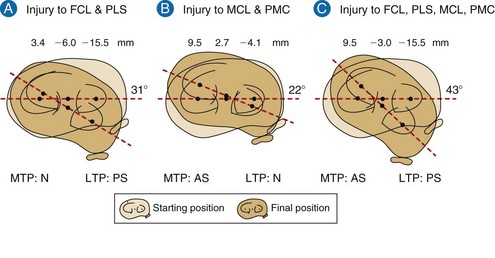
Injury to the FCL and PLS produces an increase in external tibial rotation and a posterior subluxation of the lateral tibial plateau. There are two primary restraints to external tibial rotation, the PLS at low flexion angles and both the PLS and PCL at high flexion angles (Fig. 55-14). Careful examination of knees with suspected injury to these structures may show a marked increase in external tibial rotation and posterior translation of the lateral tibial plateau or only a slight increase in these abnormal knee motions.91 The clinician’s first goal is to diagnose all the possible knee subluxations and define the extent of injury to the PLS. In 1989, we first reported on a modification of existing rotation tests to diagnose tibial rotatory subluxations of the medial and lateral tibiofemoral compartments more accurately (dial or spin rotation test).88 We then studied the amount of increased posterior subluxation of the medial and lateral tibial plateaus that result from injury to the PCL and PLS.91 We found that sectioning of the PLS results in a significant mean increase in posterior translation of the lateral tibial plateau of 8.0 mm at 30 degrees of flexion over the intact state (P < .01). No significant increase of the lateral tibial plateau occurred at 90 degrees of flexion. There was no significant increase in posterior translation of the medial tibial plateau at either flexion angle. After sectioning both the PCL and PLS, significant increases in posterior translation of the medial and lateral tibial plateaus occurred at 30 and 90 degrees of flexion (P < .01). The increase in posterior translation of the lateral tibial plateau averaged 17.8 and 23.5 mm at 30 and 90 degrees of flexion, respectively, and the increase in posterior translation of the medial tibial plateau averaged 7.6 and 12.3 mm at 30 and 90 degrees, respectively.
From the results of this study, we concluded that the diagnosis of injury to the PLS should be made based on the final position of the lateral tibial plateau and not on the amount of increased external tibial rotation alone. An increase in external tibial rotation can occur with anterior subluxation of the medial tibial plateau, posterior subluxation of the lateral tibial plateau, or a combination of both subluxations. In a prior investigation,86 we found that clinicians often misdiagnose injuries to the PLS because of misinterpretation of the increase in external tibial rotation as a posterior subluxation of the lateral tibial plateau, when in fact there was a subluxation of the medial tibial plateau caused by injury to the medial collateral ligament (MCL) alone or in combination with the ACL.
We have recommended that during the rotation tests to determine rotatory subluxations of the tibial plateaus, the examiner carefully palpate the position of each tibial plateau to determine qualitatively whether an anterior or posterior subluxation is present. We and others15,16 have reported that it is not possible to determine the actual millimeters of translation of the medial and lateral tibial plateaus in reference to the femoral condyle. Thus, a qualitative determination of whether the reference tibial plateau is anteriorly or posteriorly subluxated is recommended. The inability to measure tibiofemoral compartment translations precisely, and to quantify the amount of posterolateral subluxation, creates problems in deciding whether surgical correction is warranted.
A classification system of rotatory subluxations was previously described based on two concepts—determining the final position of the medial and lateral tibial plateaus under defined loading conditions (e.g., with either internal or external tibial rotation at a defined knee flexion angle) and classifying the position of each plateau.91 There are three possible positions for each plateau: anterior subluxation, normal position, or posterior subluxation. For each of these positions of the lateral tibial plateau, there are three corresponding positions for the medial tibial plateau (Fig. 55-15).
When a posterior subluxation of the lateral tibial plateau is positively identified by the described tibiofemoral rotation test, the examiner performs additional tests to determine whether ruptures exist to other ligamentous structures. The amount of lateral joint opening at 0 and 20 degrees of knee flexion should be determined (and quantified by stress radiography when possible) to determine the integrity of the FCL and PLS.40 The presence of a varus recurvatum in both the supine and standing positions must be carefully assessed. The difference in results of these tests between the injured and contralateral normal knee is compared because of inherent physiologic looseness that is present in some individuals. The different type of subluxations after posterolateral injuries depends on whether there is a concomitant rupture to the ACL or PCL.
Clinical Evaluation
Physical Examination
A comprehensive examination of the knee joint is required to detect all abnormalities (Fig. 55-16). This includes assessment of the following: (1) patellofemoral joint and extensor mechanism malalignment; (2) patellofemoral and tibiofemoral crepitus, indicative of articular cartilage damage; (3) gait abnormalities (excessive hyperextension or varus thrust) during walking and jogging87; and (4) abnormal knee motion limits and subluxations compared with the contralateral knee.88
Experienced clinicians are aware that patients with chronic deficiency of the PCL and PLS may develop an abnormal gait pattern, which is characterized by excessive knee hyperextension during the stance phase.87 Subjective complaints of knee instability and giving way during routine daily activities, along with severe quadriceps atrophy, often accompany this gait abnormality. Gait analysis and retraining are required in patients who demonstrate abnormal knee hyperextension patterns before proceeding with any ligament reconstruction. The failure to do so may lead to failure of reconstructed ligaments if the abnormal gait pattern is resumed postoperatively.
Diagnostic Clinical Tests
The exact determination of the extent of a PCL tear (partial versus complete) can be difficult, but is essential from a therapeutic standpoint. The clinical posterior drawer test can be highly subjective, with the forces applied too variable to allow accurate determination of the status of the PCL. MRI is not always accurate for diagnosing partial PCL tears. Frequently, this test may indicate that the ligament is completely ruptured; however, ligament continuity may still exist, with some portions functioning to limit posterior tibial subluxation to only a few millimeters.96
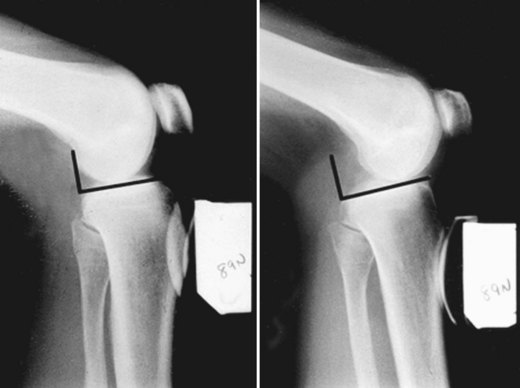
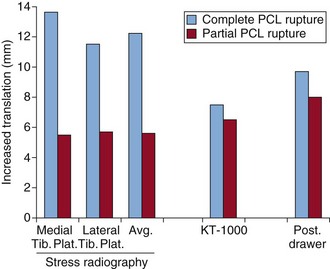
The quantitative measurement of posterior tibial subluxation in knees with PCL ruptures or reconstruction is therefore important.43 The knee arthrometer is the most frequently used device to measure posterior tibial translation following PCL injury and reconstruction. However, this device underestimates the true amount of posterior translation in PCL-deficient and reconstructed knees, often by several millimeters.58,121 Stress radiography is the most accurate and reproducible technique currently available.25,28,98,107 We recommend that PCL clinical investigations incorporate stress radiography to provide a more valid measure of posterior tibial translation (Figs. 55-17 and 55-18).
The tibiofemoral rotation dial test at 30 and 90 degrees is done to determine whether increases in external tibial rotation exist with posterior subluxation of the lateral tibial plateau (see earlier).88
The presence of a varus recurvatum in both the supine and standing positions is carefully assessed.
Imaging Studies
Posterior stress radiographs are done with an 89-N force applied to the proximal tibia (see Figs. 55-17 and 55-18).43 A lateral radiograph is taken of each knee at 90 degrees of flexion. The limb is placed in neutral rotation with the tibia unconstrained and the quadriceps relaxed. The difference in posterior tibial displacement between the injured knee and contralateral knee is recorded. More than 8 mm of increase in posterior tibial translation on stress testing indicates a complete PCL rupture.107
Full standing radiographs of both lower extremities, from the femoral heads to the ankle joints, are done in knees in which varus lower extremity alignment is detected on clinical examination. The mechanical axis and weight-bearing line are measured to determine whether a high tibial osteotomy (HTO) is indicated before PCL reconstruction.24,85 If the varus malalignment is not corrected, there is a risk that a PCL or ACL graft may fail because of the varus thrusting forces and concurrent increased lateral joint opening, producing high graft tension loads.74
Management Considerations
Posterior Cruciate Ligament Natural History
The treatment of complete isolated PCL ruptures remains controversial because of the unknown natural history of this injury in regard to long-term symptoms, functional limitations, and risk of joint arthritis. Although some studies that included patients with partial PCL deficiency have reported that patients do well when treated conservatively,* others6,19,23,48 have described noteworthy symptoms and functional limitations years after the injury, which can be disabling. A high percentage of knees with complete PCL ruptures develop articular cartilage deterioration over time; this usually occurs on the medial femoral condyle and patellofemoral surfaces because of increased joint pressures.6,34,35,123 Posterior tibial subluxation after PCL rupture has a deleterious effect to the knee, similar to that of a medial meniscectomy, because there is loss of medial meniscus function and increased joint contact stress. Posterior tibial subluxation results in a loss of normal joint kinematics (see Box 55-2) and in coupled external tibial rotation with joint loading. Accordingly, a PCL rupture has a more deleterious effect in a varus-angulated knee with associated loss of the medial meniscus and, in particular, larger athletes desiring a return to strenuous athletics. All these factors result in substantial medial tibiofemoral loads and risk of joint deterioration.
Treatment of Acute Posterior Cruciate Ligament Ruptures
Controversy exists in regard to the treatment of midsubstance complete PCL ruptures, primarily because of the lack of a scientifically proven operative procedure that can restore posterior stability and PCL function predictably. In comparison, surgical procedures to reattach the native PCL in cases of bony avulsion injuries or peel-off injuries directly at the PCL attachment site have more predictable healing rates.5,54,127,128 Even in cases of PCL rupture directly at the attachment site, there is usually sufficient ligament substance for a direct repair.
Augmentation of partial PCL tears is controversial.2,46,132 Graft reconstruction of the so-called posteromedial portion of the PCL has been described in which the anterolateral bundle is still intact and functional. The senior author (FN) has not performed augmentation procedures to date.
The treatment rationale for patients with acute PCL ruptures is shown in Figure 55-19.76 The algorithm is divided into three major sections based on the PCL tear (partial, complete, or combined with other ligament ruptures). The 10-mm division is somewhat arbitrary.
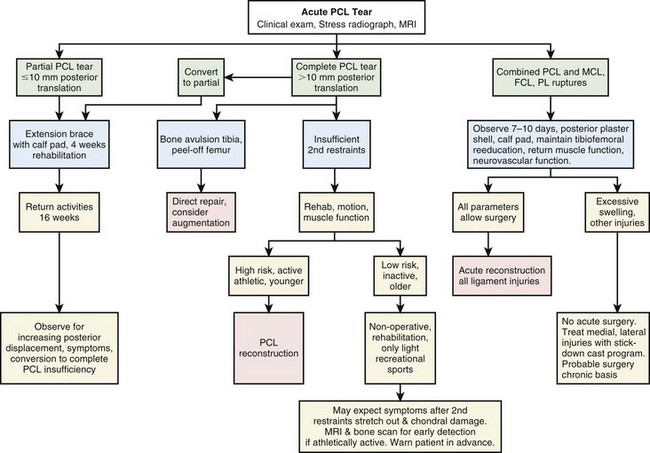
Figure 55-19 Treatment algorithm for acute PCL ruptures.
(From Noyes FR, Barber-Westin SD: Posterior cruciate ligament: diagnosis, operative techniques, and clinical outcomes. In Noyes FR [ed]: Noyes’ knee disorders: surgery, rehabilitation, clinical outcomes, Philadelphia, 2009, Saunders, pp 503–576.)
The rules to treat partial or acute isolated PCL tears are shown in Box 55-4. In our experience, 4 weeks of protection to allow initial healing of a complete PCL rupture will frequently restore partial PCL function, with less than 10-mm residual posterior tibial subluxation. The initial PCL healing process involves low tensile strength and an additional 4 to 6 weeks of protection is recommended, including avoiding athletics, running, walking on downhill grades, walking down stairs, or other high knee flexion activities that load the PCL. Even in knees with a complete PCL tear and more than 10 mm of increased posterior tibial displacement, healing of the disrupted PCL fibers may still occur, although a residual posterior tibial subluxation of a few millimeters (with a hard end point) will remain. Knees in which partial PCL function has been restored should be routinely followed, with repeat stress radiographs obtained at 6 months and over the next few years to determine PCL function. These partial PCL tears seldom require reconstruction. A repeat MRI with fast spin-echo cartilage sequences101 helps determine the integrity of the articular cartilage and provides important information for counseling the patient on athletic activities to decrease the risk of future joint arthritis.
Box 55-4
From Noyes FR, Barber-Westin SD: Posterior cruciate ligament: diagnosis, operative techniques, and clinical outcomes. In Noyes FR (ed): Noyes’ knee disorders: surgery, rehabilitation, clinical outcomes, Philadelphia, 2009, Saunders, pp 503–576.
Rules to Treat Partial or Acute Isolated Posterior Cruciate Ligament Tears
In cases of complete isolated midsubstance PCL ruptures that have more than 10 mm of increased posterior tibial displacement, and the patient is seen late after the injury and the above program cannot be instituted, one treatment approach in athletes and strenuous occupations is PCL graft reconstruction before the secondary restraints stretch out, with subsequent reinjuries. We believe that in athletic individuals, PCL reconstructive procedures have advanced to the point where more predictable results can be expected to restore sufficient PCL function to prevent gross posterior tibial subluxation. Studies have demonstrated, at least in the short term, that most patients with acute PCL ruptures treated with reconstruction are able to return to various levels of sports activities.73 Additional factors to be weighed in the decision to perform early surgery on an isolated PCL rupture (with >10 mm posterior displacement at 90 degrees flexion) include athletic goals, body weight, medial meniscus or tibiofemoral joint damage, patellofemoral joint damage, and varus malalignment, because these factors add to the effects of the residual posterior subluxation in increasing knee joint loads and subsequent joint deterioration. Sedentary patients with a complete PCL rupture and more than 10 mm of posterior translation (90 degrees flexion) are not considered surgical candidates; however, they are followed as described earlier.
Too frequently, major ligament surgery in dislocated knees performed under acute conditions results in joint arthrofibrosis, compromising the result. Patients should be carefully selected for acute multiligament repairs, realizing that there are proven techniques for reconstruction of the ruptured ligaments performed later under more ideal conditions. When surgery is performed on acute combined PCL and posterolateral ruptures, the procedure includes the use of appropriate grafts to restore lateral stability and allow an early protected range of knee motion program.77 Most acute knee dislocations should be treated in a staged approach, first by treating the acute injury and then determining whether a ligament reconstruction should be performed within the 10- to 14-day envelope or delayed. When early surgery is not advisable, the knee is protected for the first 4 weeks to prevent posterior tibial subluxation, as described earlier for acute isolated PCL ruptures. A lateral radiograph is obtained with the knee placed in a posterior plaster shell and a soft bolster positioned beneath the calf to prevent posterior tibial subluxation. The capsular tissues heal in 7 to 10 days to provide enough stability to prevent recurrence of dislocation.
Treatment of Chronic Posterior Cruciate Ligament Ruptures
The algorithm for the treatment of chronic PCL ruptures is shown in Figure 55-20. The symptoms and clinical examination determine the functional limitations, particularly the component of symptoms caused by medial tibiofemoral or patellofemoral arthritis, because these problems are likely to persist after surgical stabilization. Knees with chronic PCL ruptures are arbitrarily divided into three categories—those with varus osseous malalignment (and, rarely, valgus malalignment) in which an osteotomy must be considered, those with an isolated PCL rupture in which reconstruction may or may not be necessary, and those with significant combined ligament injuries that require reconstruction.
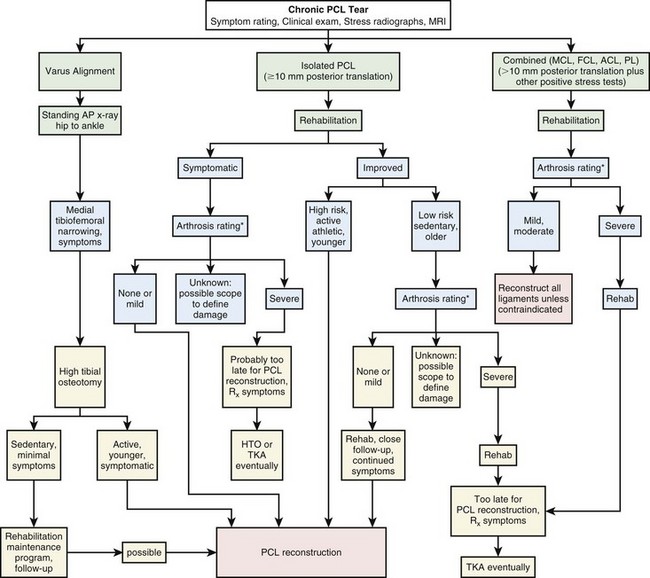
Figure 55-20 Treatment algorithm for chronic PCL ruptures.
(From Noyes FR, Barber-Westin SD: Posterior cruciate ligament: diagnosis, operative techniques, and clinical outcomes. In Noyes FR [ed]: Noyes’ knee disorders: surgery, rehabilitation, clinical outcomes, Philadelphia, 2009, Saunders, pp 503–576.)
Patients with chronic PCL deficiency who have severe muscle atrophy, loss of knee motion, or hyperextension gait abnormalities require extensive rehabilitation and gait retraining before reconstruction.87
The results of PCL reconstruction in knees with chronic ruptures are not as favorable as those that undergo reconstruction for acute injuries. This is because patients present with pain and swelling caused by joint deterioration, which often persists, even though some benefit may be gained from improved knee stability obtained from the operative procedure.73 In these knees, areas of exposed bone are frequently encountered in the medial tibiofemoral compartment, along with diffuse cartilage fragmentation in the patellofemoral joint. In these individuals, even mildly strenuous exercises aggravate the joint arthritis symptoms and cannot be performed. The patient’s initial experience with rehabilitation, and the inability to perform the required rehabilitation exercises, provides important information regarding the amount of joint arthritis that is present and joint symptoms, which are likely permanent.
If a nonoperative approach is elected, the clinician should warn the patient that the return to athletic activities may carry an uncertain prognosis and that although sports may be resumed in the short term, some form of joint arthritis will eventually ensue. It is therefore important to follow the patient at regular intervals. A bone scan may be used to provide some indication of abnormal blood flow dynamics; however, it is our experience that the onset of pain and swelling usually indicates more advanced joint damage and a poor prognosis after PCL reconstruction. An MRI scan with fast spin-echo101 sequences provides a baseline for repeated studies at 1- to 2-year intervals. The nonoperative treatment protocol of chronic PCL injuries involves educating the patient to avoid activities such as lunges and other high knee flexion activities that increase posterior tibial subluxation.
Operative Techniques: Current Concepts
PCL operative techniques continue to evolve and clinical outcome studies remain limited to allow precise decision making. The senior author’s (FN) recommended surgical approaches and relative advantages and disadvantages of each procedure are shown in Box 55-5.
Box 55-5
Adapted from Noyes FR, Barber-Westin SD: Posterior cruciate ligament: diagnosis, operative techniques, and clinical outcomes. In Noyes FR (ed): Noyes’ knee disorders: surgery, rehabilitation, clinical outcomes, Philadelphia, 2009, Saunders, pp 503–576.
Recommended Surgical Approaches
Tibial Inlay
Reserved for revision knees to bypass misplaced tibial tunnel (staged bone graft may be required)
The fourth principle is to use an autogenous graft in isolated PCL surgical procedures, when possible, because of higher success rates and healing compared with allografts.72,73 In multiligament knee injuries, allograft tissues are usually required, although an autogenous graft may be harvested from the contralateral side in select knees. In combined ligament reconstructions, a quadriceps tendon–patellar bone (QT-PT) autograft is not removed from the same knee, because this adds to the morbidity of the operative procedure.
Surgical Options
Tibial Attachment Techniques: Arthroscopic All-Inside versus Open Tibial Inlay Approach
The open posteromedial tibial inlay technique places a tibial inlay graft securely into the posterior PCL tibial attachment site. This approach may be selected when only the PCL requires reconstruction. The tibial inlay graft provides ideal graft fixation and early healing. A two-strand autogenous QT-PB graft with two femoral tunnels has been described.68,69
Biomechanical studies of PCL reconstructions have also shown the potential for graft abrasion and failure at the femoral attachment.109 Operative techniques to protect against graft failure and abrasion are therefore required at both tibial and femoral attachment sites.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree