Chapter 9
Contracture management
Contractures, or loss of joint mobility, are a common complication of spinal cord injury (see Figures 9.1 and 9.2).1–5 Neurally mediated contractures are due to spasticity (see Chapter 1)6–11 and non-neurally mediated contractures are due to structural changes in soft tissues overlying joints.

Contractures are undesirable for several reasons but primarily because they prevent the performance of motor tasks.2,12–14 For example, hip flexor contractures can impede walking in patients with paraplegia (see Figure 9.1). However, contractures also create unsightly deformities and are thought to predispose patients to pressure ulcers, pain and sleep disturbances.1–3,13,15–17
Subtle losses of extensibility in muscles acting across two joints are common sequelae of spinal cord injury but do not always result in disfiguring and obvious contracture. Such losses of extensibility can, however, have important implications for function. For example, even a modest loss of extensibility in the hamstring muscles can prevent a patient with C6 tetraplegia from sitting unsupported on a bed with the knees extended (see Figure 3.2, p. 59). Similarly, a small loss of extensibility in the gastrocnemius muscles can limit the gait of a patient with the potential to walk.
Contractures, like other impairments, need to be linked to activity and participation goals during the goal planning process (see Chapter 2). In the above examples, hip flexor contractures would be linked to walking-related goals and loss of hamstring muscle extensibility would be linked to sitting-related goals. The linking of contractures to activity and participation goals ensures that interventions are concentrated where they really matter. It is also important during the goal planning process to anticipate contractures which may develop in the future, and which may ultimately limit activity and participation, so strategies can be put in place to prevent them.
Assessment
Measurements of passive joint range of motion are used to quantify the severity of contractures. A baseline assessment of all joints is required to identify existing problems and monitor change over time. These measurements are typically done with a goniometer. To identify the loss of extensibility in muscles crossing two joints, it is important to ensure appropriate positioning of the second joint. For example, measurements of hip flexion with the knee flexed reflect the extensibility of the tissues on the extensor aspect of the hip and measurements of hip flexion with the knee extended specifically reflect the extensibility of the hamstring muscles. Similarly, measurements of wrist extension with the fingers extended reflect the extensibility of the extrinsic finger flexor muscles.18
Joint angle is a direct function of the torque applied to a joint (usually through the hands of therapists, and sometimes from the weight of a limb). Joint range of motion measured with a larger torque will be greater than joint range of motion measured with a smaller one.19 Consequently, if comparisons are to be made of repeated measures, it is important that the same torque is applied on each occasion. It is often difficult for therapists to manually apply a consistent torque when testing joint range of motion, especially when measurements are taken weeks or months apart. In this situation, changes in joint range of motion are not necessarily indicative of underlying changes in tissue extensibility. There are various devices which can be used to standardize torque to overcome this problem.18,20–22 The use of these devices is warranted when accurate measurements are important (e.g. to determine the effectiveness of costly, time-consuming, inconvenient or surgical interventions).
It is useful to try and distinguish between neurally mediated and non-neurally mediated contractures because treatment may differ.23 For example, anti-spasticity medication is appropriate for management of neurally but not non-neurally mediated contractures. In practice, however, contractures are often due to both factors and a distinction between the relative importance of each factor is difficult. A contracture is likely to have a neurally mediated component if there are signs of spasticity such as clonus or a velocity-dependent increase in resistance to stretch. Measurements of joint range of motion are more reproducible when spasticity is not a key feature. Spasticity can be dampened by measuring joint range of motion after a sustained 2- or 3-minute stretch. However, the only definite way to determine the contribution of neurally mediated factors to a contracture is to measure passive joint range of motion when spasticity is pharmacologically blocked (e.g. when patients are anaesthetized). There are standardized measures of spasticity, although their clinical usefulness is disputed (see Chapter 1).
Treatment and prevention of contractures
Stretch and passive movements
Stretch and passive movements have become the cornerstone of physiotherapy management directed at the treatment and prevention of contractures in patients with spinal cord injury.24–28 In many spinal cord injury units it has become accepted practice for therapists to routinely administer between 2 and 10 minutes of passive movements and stretch a day to each affected joint of each patient, particularly patients confined to bed in the period immediately following injury.25,29 These types of interventions are labour intensive and can equate to an hour of treatment per patient per day.
While clinical lore supports the efficacy of passive movements and stretch, the science is less convincing. There is still much uncertainty about whether these interventions are truly effective and, if they are, how long stretches need to be maintained and how frequently passive movements need to be administered. The optimal stretch torque is also unknown although one study, at least, indicates that therapists have differing ideas of what constitutes a therapeutic stretch.30 Some therapists apply stretches to the hamstring muscles of patients with spinal cord injury well in excess of that which would be tolerated by able-bodied people with normal sensation. It is also unclear whether passive movements and stretch primarily target the neurally mediated or non-neurally mediated determinants of contractures. Definitive answers to these questions are unknown but some of the current controversies are outlined in the next section.
Evidence from animal studies
The use of passive movements and stretch-based interventions to treat and prevent contractures is usually justified by animal studies.31–33 Animal studies indicate that soft tissues undergo deleterious changes in response to prolonged immobilization, especially immobilization in shortened positions.34–36 For example, 10 days immobilization of the ankles of rabbits in a plantarflexed position (the shortened position of the plantarflexor muscles) results in approximately a 10% reduction in resting length of soleus muscle–tendon units,36 which produces functionally significant loss of ankle joint mobility. Muscle shortening is associated with decreases in the number of sarcomeres,34,35,37 changes in the extent and arrangement of collagen38,39 and concentration of glycosaminoglycans,40 and decreases in tendon resting length.5,31,34–36,38,41–50 These deleterious structural and morphological changes associated with immobilization can be prevented36or reversed34 by prolonged and uninterrupted stretch. In animals, prolonged stretch is typically applied with plaster casts for many days. Stretch is believed to provide a sufficiently strong stimulus to trigger appropriate remodelling of soft tissues. Similar findings have been found in denervated muscles, although the response appears to be slower.51–53
While animal studies show that continuous and uninterrupted stretch can prevent or reverse deleterious soft tissue adaptations associated with immobilization, the effectiveness of short periods of stretch are less clear.43,54 Most of what is known about the effects of short periods of stretch comes from one important study in mice, which found that just 15 minutes of stretch each day partly prevented loss of sarcomeres in the plantarflexor muscles of ankles immobilized in a shortened position, and 30 minutes of stretch were sufficient to completely prevent loss of sarcomeres.54 The effectiveness of less than 15 minutes of stretch a day, such as typically administered in the clinical setting, is unknown. The results of animal studies need to be interpreted with caution because animal muscles respond to stimuli such as stretch more rapidly than human muscles. A 15-minute stretch which prevents loss of sarcomeres in the plantarflexor muscles of small animals will not necessarily produce the same effects in humans with spinal cord injury.
Evidence from clinical trials
A large number of trials have examined the effects of stretch on tissue extensibility in various populations. Most of these trials have been carried out in able-bodied individuals.55,56 Two methodological issues limit the usefulness of many trials. First, most trials measure the effects of stretch soon after the last stretch intervention. Measurements at this time reflect the transient effects of stretch due to viscous deformation.57–61 They do not provide good evidence of the lasting effects of stretch ontissue extensibility and remodelling31 essential for the treatment and prevention of contracture. A second limitation is that most trials do not standardize the torque used to measure joint range of motion. They are therefore unable to differentiate between underlying changes in tissue extensibility and changes in patients’ tolerance to uncomfortable stretch when sensation is present.62,63
A few randomized trials of the effects of stretch have been conducted in patients with spinal cord injury.27,64–67 All involved the application of 30 minutes of stretch three to five times a week over a 4-week or 3-month period to either the plantarflexor,64,66 shoulder27, thumb67 or hamstring muscles65 of patients with spinal cord injury. In four of the five studies outcomes were measured using standardized torques at least 1 day after the application of the last stretch. All five studies showed that regular stretch had little or no effect on joint range of motion. These results are consistent with randomized controlled trials in patients with other types of neurological disabilities68–73 and indicate that therapists’ confidence about the effectiveness of stretch is not yet justified.
Ways of administering sustained stretches
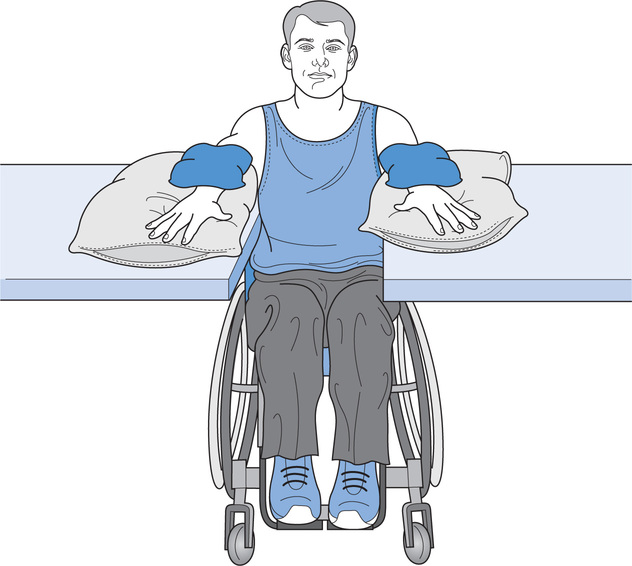
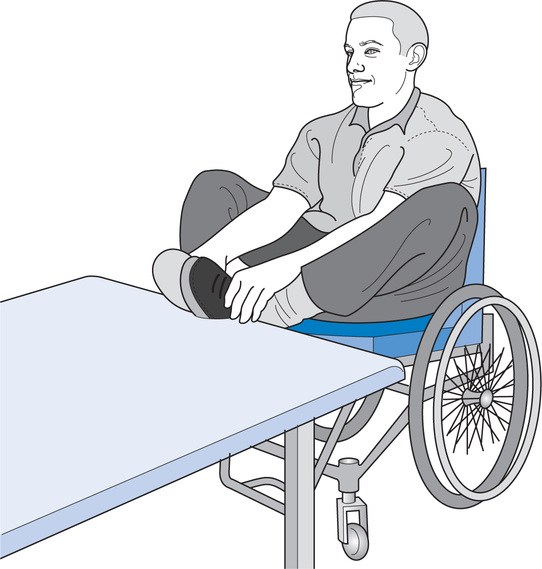
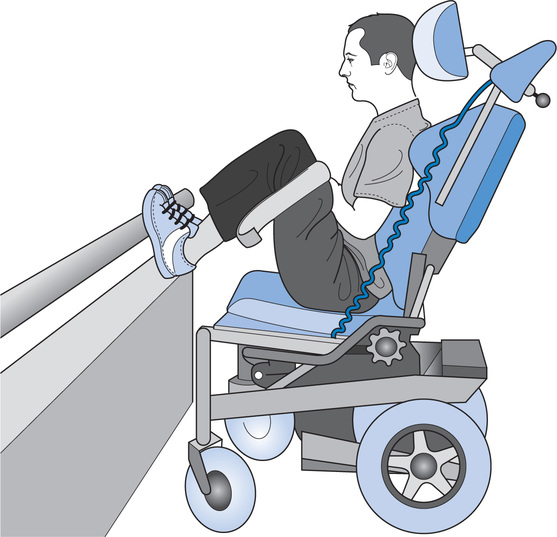
If stretches are to be sustained for more than a few minutes a day, they cannot be applied manually by therapists. Instead, stretches need to be applied with positioning, splinting74 and standing75 programmes. These programmes should be incorporated into patients’ daily routines and continued after discharge. Often only simple strategies are needed, especially if stretches are instigated before contractures have developed (see section below on Preventing and anticipating contractures). For example, the shoulder extensor, hamstring, hip internal and hip extensor muscles can all easily be stretched by placing the arms or legs on stools or tables (see Figures 9.3–9.6).

More sustained stretches can be applied with serial casts to immobilize joints in their stretched positions. The casts are reapplied every few days to maintain the stretch. Serial casts should only be considered for severe and disabling contractures because they can impede independence, be uncomfortable and are time-consuming to apply. They are also associated with a substantial risk of skin breakdown.70,76
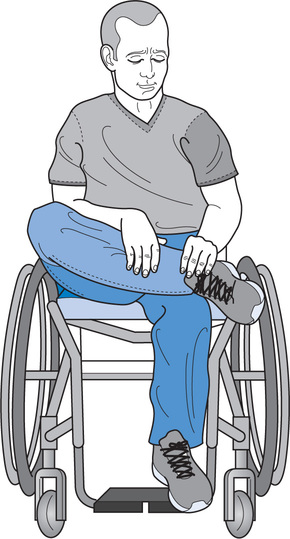
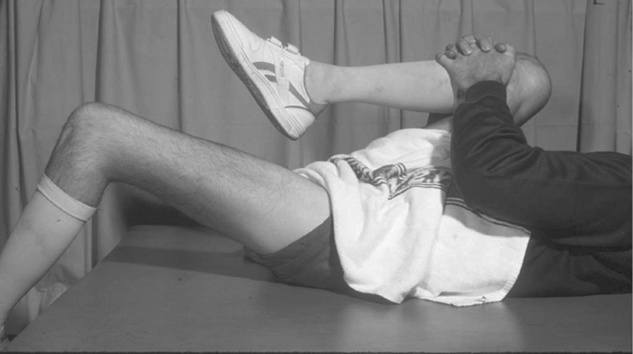
Patients also need to be educated about methods of self-administering stretches. For example, the hip internal rotator muscles can be stretched by sitting with one foot on the opposite leg (see Figure 9.7). Patients with lower levels of tetraplegia can self-stretch the interphalangeal joints (IP) of the fingers into extension while sitting in a wheelchair by using the rim of the wheel as a pivot bar (see Figure 9.8). Similarly, they can stretch the metacarpophalangeal (MCP) joints of the hand into flexion by appropriately placing the hand on a hard surface (see Figure 9.9). All these types of strategies can be incorporated into patients’ lives with minimal inconvenience and reliance on others. For similar stretch ideas, readers are referred to www.physiotherapyexercises.com.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree