Chapter 5
Hand function of people with tetraplegia
Loss of hand function is often more important to people with tetraplegia than loss of lower limb function and the inability to walk.1,2 This reflects the importance of hand function for independence. The purpose of this chapter is to describe how people with different patterns of paralysis use their hands and to outline some of the splints and adaptive equipment commonly prescribed. The use of surgery and electrical stimulation to improve hand function will also be discussed.
The same generic framework advocated for devising physiotherapy programmes in Chapter 2 can be used for hand management. Initially, goals of treatment are negotiated with the patient. Goals need to also be set in conjunction with occupational therapists and other team members who share responsibility for their attainment. Goals are expressed with respect to activity limitations such as taking a spoon to the mouth and using a keyboard. Goals can also be expressed with respect to participation restrictions such as dining out with friends or returning to work. Once realistic goals are defined, impairments preventing the attainment of each goal are identified but only with respect to impairments which physiotherapy can address. These typically include poor strength, joint mobility and skill.
The hand function of patients with tetraplegia is primarily limited by neurological status (see Appendix). Below is a summary of the hand function typically attained by a patient with different ASIA motor complete lesions.
Hand function and principles of therapy
C4 and above tetraplegia
Patients with C4 and higher levels of tetraplegia have no upper limb function.
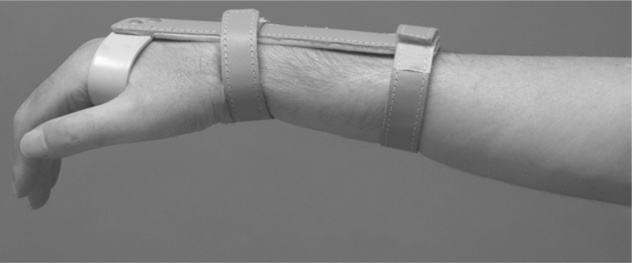
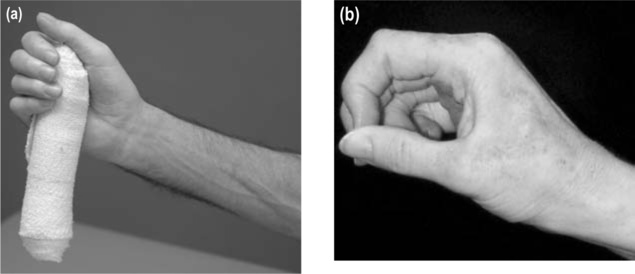
Therapy for these patients is directed at preventing contractures. It is important to prevent contractures because they can be unsightly and create problems with hygiene and personal care. Contractures of the hand are probably best avoided with prolonged stretch and regular passive movements (see Chapter 9). Prolonged stretch can be administered with splints. In patients without contractures, the appropriate type of splint is determined by the type of contractures patients are most likely to develop. For example, patients with total paralysis of the hands commonly develop metacarpophalangeal (MCP) joint hyper-extension and interphalangeal (IP) joint flexion contractures. Therefore the appropriate splint is one which immobilizes these joints in a stretched position, namely MCP joint flexion and IP joint extension (see Figure 5.1). A less aggressive ‘functional’ splint which places the hand in a neutral position does not stretch these joints and is probably less effective for preventing these types of contractures. In patients with existing contractures, the appropriate type of splint is determined on a case-by-case basis but the splint needs to provide a substantial stretch to affected joints.
C5 tetraplegia
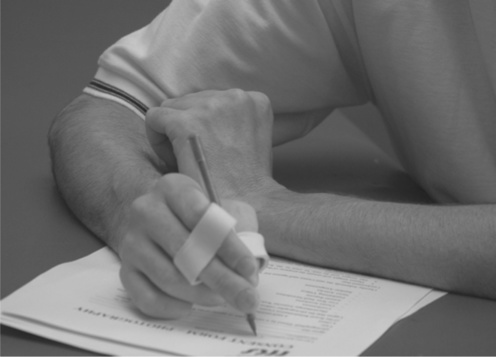
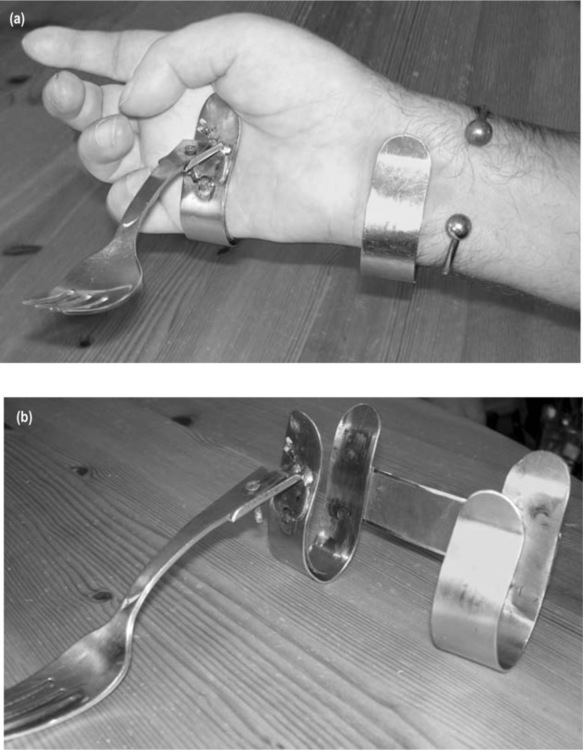
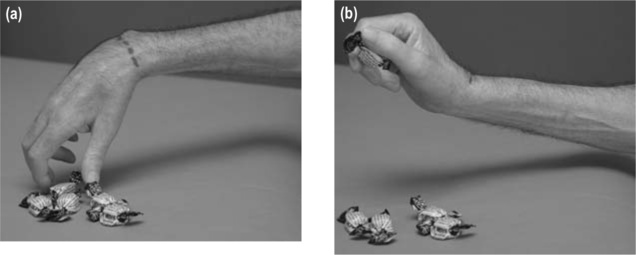
Patients with C5 tetraplegia have anti-gravity strength in their biceps muscles. Often, but not always, they have sufficient strength in their deltoids and other shoulder muscles to lift a hand to the face. However, these patients have paralysis of all wrist and hand muscles and consequently are unable to grasp objects. Instead, objects can be manipulated by clamping them between the wrists (see Figure 5.2), balancing them on an upturned hand (see Figure 5.3) or using orthoses which attach objects to the hand (see Figure 5.4). Splints are commonly used to support the wrist (see Figure 5.5).
Poor shoulder strength and passive joint mobility commonly limit the hand function of patients with C5 tetraplegia. In addition, hand function is limited by lack of skill, particularly in patients soon after spinal cord injury. That is, patients do not know how to use their paralysed hands in purposeful ways. Therapy is therefore directed at each of these three impairments using the principles outlined in Chapters 7–9.
An important additional aspect of hand management for these patients is the provision of appropriate aids, splints and orthoses (some examples of commonly prescribed hands splints are provided in Figures 5.3–5.5). This is generally the responsibility of occupational therapists. Hand function of some patients can also be improved with surgery or electrical stimulation (see p. 104).
C6 and C7 tetraplegia
Patients with C6 and C7 tetraplegia have reasonable shoulder strength and can readily bring the hand to the mouth. They have paralysis of all finger and thumb flexor muscles but they retain good strength in their wrist extensor muscles. Those with C7 tetraplegia also have some strength in their wrist flexor and finger extensor muscles. Most patients with C6 and C7 tetraplegia rely on a tenodesis grip for crude hand function (see below). Hand splints, aids, electrical stimulation and surgery are other important aspects of overall hand management (see Figures 5.6 and 5.7).3
Tenodesis grip
A tenodesis grip is a method of grasping used by patients with C6 and C7 tetraplegia who have paralysis of finger and thumb flexor muscles but active wrist extension. The tenodesis grip relies on passive tension generated in the paralysed extrinsic finger and thumb flexor muscles (flexor digitorum superficialis, flexor digitorum profundus and flexor pollicis longus) with wrist extension.3–8 The open hand is placed around an object with the wrist flexed. The wrist is then actively extended, increasing the passive tension in the paralysed finger and thumb flexor muscles and pulling the fingers and thumb into flexion. In this way, objects can be grasped between the paralysed thumb and index finger or in the palm of the hand (see Figures 5.8 and 5.9). A tenodesis grip provides crude but nonetheless useful hand function.7 Some patients can enhance the effectiveness of their tenodesis grip by eliciting spasm in the extrinsic thumb and finger flexor muscles with wrist extension.
The tenodesis grip can be used to grasp objects between the thumb and index finger using either a lateral key or pincer grip. In the lateral key grip the pad of the thumb contacts the side of the index finger (see Figure 5.8b) and in the pincer grip the tip of the thumb contacts the tip of the index finger (see Figure 5.9b). The type of grip attained is primarily determined by the extensibility of the thumb adductor muscles. A pincer grip is attained if the thumb adductors are extensible and a lateral key grip is attained if the thumb adductors are inextensible. The point of contact between the thumb and index finger also depends to a lesser degree on the relative lengths of the thumb and index finger, and the extensibility of the extrinsic finger flexor muscles.3,4
The passive tenodesis grip of people with C5 tetraplegia is of limited functional use and most patients gain superior upper limb function from splints which stabilize the wrist (see Figure 5.5). A passive tenodesis grip cannot be used in conjunction with these splints because the splints prevent passive wrist extension. However, strategies appropriate for promoting a tenodesis grip in patients with C6 and C7 tetraplegia are also appropriate for promoting a passive tenodesis grip in people with C5 tetraplegia.
Splinting and taping to promote a tenodesis grip
Splinting and taping are widely used to encourage loss of extensibility in the extrinsic finger and thumb flexor muscles and promote a tenodesis grip. However, it remains unclear whether either intervention can decrease the passive extensibility of the extrinsic finger and thumb flexor muscles and improve hand function.8,9 This controversy is discussed in more detail below.
Splinting and taping programmes to promote a tenodesis grip may need to be withheld if patients are likely to have hand surgery. Often the effectiveness of hand surgery relies on good extensibility in the finger and thumb flexor muscles. However, the difficulty with this approach is that often the decision about hand surgery is not made until 1 or 2 years after injury. Consequently, it is not always clear which patients will and will not ultimately be suitable candidates. In addition, some patients suitable for hand surgery do not elect to have it (see p. 104 for further discussion).2 The dilemma for therapists is whether they should compromise hand function by withholding strategies designed to promote a tenodesis grip on the basis that patients may have hand surgery in the future.
A theoretical basis for splints designed to promote a tenodesis grip
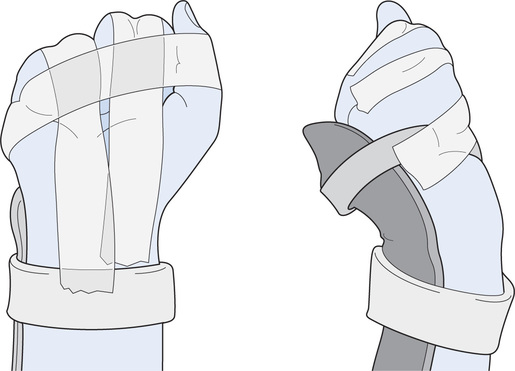
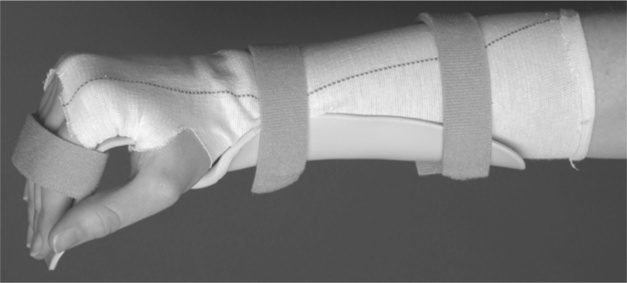
Animal studies have convincingly shown that immobilization of muscles at short lengths induces shortening (see Chapter 9). On this basis, it has been argued that the best way to promote a tenodesis grip is with a splinting or taping regime which immobilizes the extrinsic finger and thumb flexor muscles in their shortened positions. To achieve this, one of two splinting regimens is probably best adopted. The more conservative approach is to splint the hand in a relatively neutral position with the MCP joints fully flexed, the IP and wrist joints extended and the thumb flexed against the side of the index finger (see Figure 5.1). This type of splint immobilizes the extrinsic finger and thumb flexor muscles in a relatively shortened position but discourages extension contractures of the MCP joints and flexion contractures of the IP joints.
A second more aggressive approach is to flex the MCP and proximal IP joints of the fingers with the thumb positioned against the side of the index finger. This is typically done by applying tape across the back of the fingers and thumb (see Figure 5.10). The wrist is held in an extended position with a splint. The flexed position of the fingers places the extrinsic finger flexor muscles in a shortened position. However, it also substantially increases the risk of undesirable flexion contractures of the proximal IP joints. If this second approach is used, the hand needs to be carefully monitored and patients should spend at least some time of each day with the proximal IP joints in full extension. In addition, passive movements to the proximal IP joints should be regularly administered. Whenever the IP joints are extended, the wrist and MCP joints need to be flexed to avoid stretch of the extrinsic finger flexor muscles (see Figure 5.11).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree