Chapter 11
Respiratory management
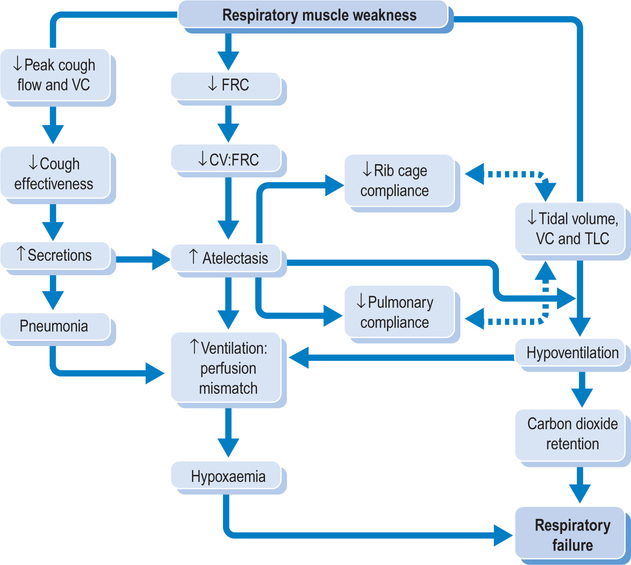
Respiratory complications are a common cause of morbidity and mortality in patients with spinal cord injury.1–21 They occur throughout patients’ lives and are a leading cause of hospitalization. Patients are particularly susceptible to respiratory complications in the first few weeks after spinal cord injury. At this time, respiratory complications are the second leading cause of death.2,21 The common respiratory complications are hypoventilation, atelectasis, secretion retention and pneumonia.2,22,23 Each leads to a mismatch between ventilation and perfusion, resulting in hypoxaemia and, if untreated, respiratory failure.10,15,24 Not surprisingly, patients with tetraplegia are particularly vulnerable.1,2,21
The respiratory function of patients with spinal cord injury is primarily determined by neurological status (see Table 11.1 for level of innervations of the key respiratory muscles)25 and can be summarized as follows:
Table 11.1
Levels of innervation for the sternocleidomastoid, diaphragm, scalene, pectoralis, intercostal and abdominal muscles
| Cranial nerve XI | Sternocleidomastoid |
| C3–C5 | Diaphragm |
| C3–C8 | Scalene |
| C5–T1 | Pectoralis |
| T1–T11 | Intercostals |
| T6–T12 | Abdominals |
See Appendix 1 for more details.25
C1 and C2 tetraplegia. Patients with lesions at C1 and C2 have total paralysis of the diaphragm, intercostals and abdominal muscles and are therefore ventilatory-dependent. They, however, retain some voluntary control of accessory respiratory muscles such as the sternocleidomastoid muscles. These muscles receive innervation from cranial nerves and contribute to respiration in a small way, although they have little functional importance in patients with such high levels of tetraplegia requiring mechanical ventilation.26
C3 tetraplegia. Patients with lesions at C3 have marked but not total paralysis of the diaphragm. They have some voluntary control of the scalene muscles which assist respiration. Most, however, require long-term mechanical ventilation.27
C4 tetraplegia. Patients with lesions at C4 have partial paralysis of the diaphragm and total paralysis of the intercostal and abdominal muscles. Most can breathe independently, typically after short periods of invasive mechanical ventilation following injury. They have little ability to cough and a vital capacity less than one third of predicted.23,28 They have minimal expiratory reserve.
C5–C8 tetraplegia. Patients with lesions at C5–C8 have full voluntary control of the diaphragm, partial voluntary control of the scalene and pectoralis muscles and full paralysis of the intercostal and abdominal muscles. They have a poor cough and a vital capacity of between one third and one half of predicted.23,28 The pectoralis muscles are significant because they contribute to expiration.29–31
Thoracic paraplegia. Patients with thoracic paraplegia have full voluntary control of the diaphragm, scalene and pectoralis muscles but varying amounts of paralysis of the intercostal and abdominal muscles. Some have a normal vital capacity23,28 but a weak cough. It is not until the lesion is below T12 that respiratory function can be deemed normal.32
The direct and indirect effects of respiratory muscle weakness
Patients with spinal cord injury have a restrictive pattern of breathing with marked reductions in all lung volumes and capacities (except residual volume; see Table 11.2 and Figure 11.1).11,12,15,18,19,26,28,33–46 Expiratory flow and peak cough flow rates are also adversely affected. All these changes are due to the direct and indirect effects of respiratory muscle weakness. They explain patients’ heightened susceptibility to hypoventilation, atelectasis, secretion retention and pneumonia.
Table 11.2
Definition of lung volumes, capacities and flows
| Parameter | Definition |
| Tidal volume | The volume of air inspired (or expired) in a quiet breath40,46 |
| Vital capacity | The volume of air expired after a maximal inspiration41–43 |
| Inspiratory capacity | The volume of air inspired after a normal expiration42,43 |
| Inspiratory reserve | The maximum volume of air inspired after a tidal volume inhalation46 |
| Expiratory reserve | The maximum volume of air expired after a tidal volume exhalation46 |
| Total lung capacity | The total volume of air contained in the lungs at maximal inspiration41–43 |
| Residual volume | The volume of air remaining in the lungs after a maximal expiration41–43 |
| Closing capacity | The volume of air trapped by the closure of airways on expiration after a maximal inspiration41,43 |
| Functional residual capacity | The volume of air remaining in the lungs after a normal expiration41–43 |
| Peak expiratory flow rate | The maximal flow rate generated on expiration after a maximal inspiration42 |
| Peak cough flow rate | The maximal flow rate generated during a cough after a maximal inspiration45,77 Under normal circumstances, peak cough flow rates are higher than peak expiratory flow rates44,45 |
| Forced expiratory volume in 1 second (FEV1) | The volume of air expelled in the first second of a maximal forced expiration after a maximal inspiration40,46 |
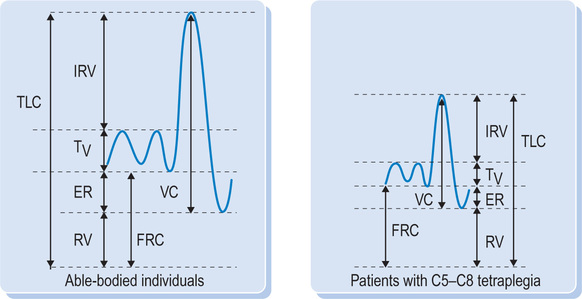
Tidal volume, vital capacity and total lung capacity
In the laboratory, respiratory muscle strength is quantified by measuring mouth or pleural pressures during maximal static inspiratory and expiratory efforts, respectively.9,47,48 Not surprisingly, there is a marked reduction in maximal inspiratory and expiratory pressures of patients with tetraplegia reflecting respiratory muscle weakness.9,33,35,47–51 Poor inspiratory and expiratory muscle strength directly limits vital capacity, total lung capacity and their determinants.9,10,16 Tidal volume is also reduced but this is compensated for by an increase in respiratory rate.
The decreases in lung parameters are greater than expected from muscle weakness alone.10,33,48 For example, it has been calculated that the direct effects of inspiratory muscle weakness explain some, but not all, of the observed loss in total lung capacity.47 This disparity is due to the indirect effects of respiratory muscle weakness and, in particular, the effects of respiratory muscle weakness on pulmonary and rib cage compliance.9,10,33,47,49
Pulmonary compliance reflects lung stiffness. It is reduced by approximately 30% in people with tetraplegia.20,33,52,53 Decreases in pulmonary compliance are undesirable because as pulmonary compliance decreases it becomes more difficult to inflate the lungs. This is a problem for patients already having difficulty inflating the lungs due to inspiratory muscle weakness. Decreases in pulmonary compliance are typically attributed to chronic atelectasis.54,55 Chronic atelectasis directly increases the surface tension of alveoli. It also leads to a reduction in surfactant. Both factors adversely affect the distensibility of alveoli.56,57 However, decreases in pulmonary compliance may also be due to changes in the elasticity of lung tissue.58 Not surprisingly, while pulmonary compliance is always reduced in patients with tetraplegia, it is further reduced during periods of acute respiratory illness characterized by secretion retention and atelectasis.9,10,47,48,59
Rib cage compliance reflects the stiffness of the rib cage and its resistance to movement during respiration.20,35,49 It is decreased in people with tetraplegia, exacerbating losses in lung volumes.10,35,49 The decrease in rib cage compliance occurs over time secondary to poor rib cage expansion. Rib cage expansion is limited because of respiratory muscle paralysis and because patients are physically inactive.35,49 Without regular expansion and movement of the rib cage, the thoracovertebral and costosternal joints become stiff.10,29,35,49 Rib cage expansion may also be limited by spasticity although the link between spasticity and rib cage compliance is disputed.10,33,35,49,58,60
The direct and indirect effects of respiratory muscle weakness on tidal volume, vital capacity, total lung capacity, and pulmonary and rib cage compliance are undesirable for many reasons (see Figure 11.2). If severe, they lead to hypoventilation characterized by carbon dioxide retention and hypoxaemia.32,61 In addition, they lead to poorly ventilated areas of the lung which are highly susceptible to atelectasis. Atelectasis decreases pulmonary compliance, creating a snowball effect where the effects of atelectasis on pulmonary compliance causes further atelectasis. Atelectasis is also due to other factors such as decreases in functional residual capacity and secretion retention (see below). Atelectasis is common and can cause bacterial overgrowth leading to pneumonia,2 pleural effusion and empyema (infection within a pleural effusion).22,23
Functional residual capacity
Functional residual capacity is also reduced in patients with tetraplegia, especially during periods of acute respiratory illness.9,12,20,33–36,47–49,62 Functional residual capacity is the volume of air in the lungs after a normal relaxed expiration and is determined by the balance between the tendency of the lungs to recoil inwards and the chest wall to pull outwards.10,33,47,48,60,63 Decreases in functional residual capacity are primarily due to decreases in the outward pull of the chest wall. Changes in chest wall recoil occur over time in people with tetraplegia and are due to patients’ inability to regularly expand the chest wall to large lung volumes (see discussion above).9,33,47–49,60 During periods of acute respiratory illness reductions in functional residual capacity are common and due to underlying lung pathology.
Reductions in functional residual capacity predispose patients to atelectasis. If closing capacity is higher than functional residual capacity, the alveoli in dependent regions of the lung collapse on expiration. This occurs during normal tidal breathing, trapping air and precipitating atelectasis.41
Expiratory flow rates
Respiratory muscle weakness directly affects the ability to forcibly expire and generate high expiratory flow rates. This is reflected by marked reductions in forced expiratory volume in 1 second, maximal expiratory flow rate and peak cough flow.4,10,13 These reductions are primarily due to the direct effects of abdominal and intercostal muscle weakness.
A forced expiration is dependent on generating high intrathoracic positivepressures.64 In able-bodied individuals, these are generated when the abdominal muscles contract and pull the abdominal contents inwards and upwards, thereby increasing intrathoracic positive pressures and decreasing lung volumes.65 The intrathoracic positive pressures are further increased by the action of the intercostal muscles on the rib cage. Without intercostal and abdominal muscle activity, large positive intrathoracic pressures cannot be generated and, consequently, expiration is largely passive and dependent on the elastic recoil of the lungs. Forced expiration is further restricted by poor inspiration. Without large volumes of air in the lungs at the commencement of expiration, the ability to generate high expiratory flow rates is further reduced.5,8,10,13,15,17,26,29,30,36,44,64,66–70
The inability to forcibly expire prevents an effective cough. High flow rates are required to generate turbulent air flow through the trachea and large bronchi.64,69,71–74 This in turn creates shear forces on the walls of the airways which entrain secretions and move them up to the pharynx.71,75 Typically, in able-bodied individuals, flow rates of between 6 and 20 l.sec21 are generated during coughing,44,64 although peak flow rates as low as 2.7 l.sec21 can help move secretions within the airways.44,68,73,76 As a general rule patients unable to generate maximal expiratory flow rates of at least 4.5 l.sec21 and with vital capacity less than 1.5 l during health will be unable to generate the critical flow rates required during periods of acute respiratory illness.44,73,77
Without an effective cough, patients are highly susceptible to secretion retention. The accumulation of secretions and in particular secretion plugging causes atelectasis.5,17,30,44,66 Secretions also contribute to decreases in pulmonary compliance. Secretions act as a direct physical barrier to the ventilation of distal regions of the lungs and increase the risk of pneumonia.5,10,17,30,44,66,72,74 Secretions are a noted problem during acute respiratory illnesses when secretion production is increased.69,78 The loss of sympathetic supraspinal control and the resultant unchecked parasympathetic activity also increases the production of secretions.2 Patients with C5 and below tetraplegia are less vulnerable to problems associated with sputum retention than patients with C4 tetraplegia because they retain voluntary control of the clavicular portion of the pectoralis muscles.30,79 In the absence of intercostals and abdominal muscles, the pectoralis muscles play an important role in assisting cough and forced expiration.29–31
Residual volume
Residual volume is the only lung volume that is not decreased with respiratory muscle weakness. Residual volume is the amount of air left in the lungs at the end of a maximal expiration and is typically increased due to the inability to forcibly expire and remove air from the lungs.10,34,47,80 However, residual volume can be unchanged despite expiratory muscle weakness.33,48 This occurs if there is a corresponding decrease in the tendency for the chest wall to recoil out to functional residual capacity. Residual volume is determined by competing factors: the strength of the expiratory muscles and the inwards pull of the lungs tending to decrease residual volume, and the outward pull of the chest wall tending to increase residual volume.10,20,47,60 Increases in residual volume are not associated with increases in total lung capacity.
Rib cage distortion
There are several patterns of rib cage distortion seen during breathing in patients with tetraplegia.58,81 The precise pattern is determined by factors such as the level of the lesion, strength of accessory respiratory muscles, rib cage compliance and extent of spasticity. Some patients demonstrate paradoxical breathing where the negative intrathoracic pressures associated with inspiration ‘suck’ the upper ribs inwards. This phenomenon is paradoxical because in able-bodied individuals the upper ribs move up and outwards during inspiration in response to intercostal muscle activity. Patients with lesions at and below C5 have less pronounced upper rib cage indrawing because of preserved function in the scalene and other respiratory accessory muscles.58 Rib cage indrawing is less pronounced in the lower ribs because they are ‘pulled’ outwards by the direct action of the diaphragm.
Respiratory complications in the period immediately after injury
While patients with tetraplegia are always susceptible to respiratory complications, they are far more susceptible in the period immediately after injury.5,8,10,12 The reasons for this are outlined below.
Prolonged bedrest
Prolonged bedrest is often required for the management of vertebral instability but it has a dampening effect on respiratory function.82–84 In particular, it decreases functional residual capacity16 and vital capacity, promotes atelectasis and increases susceptibility to pneumonia. While the period of bedrest can often be reduced ifvertebral instability is managed surgically, this approach exposes patients to the respiratory risks associated with anaesthesia.82,84–88 Often, medical staff weigh up the relative respiratory risk of conservative versus surgical management after taking into account all aspects of patients’ care.
Aspiration
Patients with recent tetraplegia are at increased risk of aspiration and subsequent pneumonia, particularly if they are elderly and have recently undergone anterior cervical spine surgery.23 Aspiration is also common in those susceptible to vomiting, especially if they are nursed in the supine position and unable to turn the head.
Paralytic ileus
The respiratory function of patients with recently-acquired tetraplegia is further compromised by the associated paralytic ileus. Paralytic ileus is a condition in which the gastrointestinal system temporarily ceases to function (see Chapter 1).82,84 The condition develops within the first 48 hours after injury and can usually last for a few days.82,84 The development of a paralytic ileus increases the risk of pulmonary complications because it distends the abdomen.4 Abdominal distension is undesirable because it impedes the movement of the diaphragm, increases the work of breathing and heightens susceptibility to basal atelectasis.4,22 In addition, a paralytic ileus predisposes patients to vomiting which can cause aspiration.4
Respiratory muscle fatigue
Immediately after injury the remaining non-paralysed respiratory muscles must compensate for the loss of other important respiratory muscles. This is a sudden change in function and the remaining non-paralysed respiratory muscles are not sufficiently adapted to perform the additional work of breathing.16,22,31,50,89 With time, non-paralysed respiratory muscles adapt and are better able to compensate for the loss of other respiratory muscles.90 That is, there is an improvement in respiratory muscle strength and endurance.90,91 The respiratory training effect which occurs in the early days and weeks after injury is accompanied by a gradual increase in vital capacity. For example, vital capacity can almost double in patients with C4–C6 tetraplegia over the first 3 months.15 Improvements in vital capacity are also due to other factors, including neurological recovery.2
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree