Chapter 6
Standing and walking with lower limb paralysis
Approximately 50% of people with spinal cord injury walk.1–6 For some, walking is their primary form of mobility and for others it is used only for therapeutic purposes, or only for specific tasks which require being upright. Neurological status is the strongest predictor of walking. The level of ambulation typically attained can be summarized as follows:
People with tetraplegia. People with tetraplegia and total paralysis of the lower limbs (i.e. ASIA A or B) can stand with frames, tilt tables or standing wheelchairs. The primary purpose for standing is to obtain the therapeutic benefits associated with being upright and weight bearing through the legs (p. 109).
People with thoracic paraplegia. People with thoracic paraplegia and total paralysis of the lower limbs (i.e. ASIA A or B) can ambulate with walking aids on level ground provided they have good upper limb strength and extensive orthotic support. Gait is slow and the energy cost of walking is high.7–10 These people usually find it difficult to perform associated tasks such as walking up and down slopes, negotiating steps and uneven terrain, putting the orthoses on and off, and turning in tight spaces.6,8,11–13 The reliance on walking aids is particularly limiting because it largely prevents the use of the hands when upright for tasks such as cooking and carrying bags.14 In addition, some do not like the appearance and bulkiness of the orthoses. For all these reasons, most people with thoracic paraplegia and total paralysis of the lower limbs stand only for exercise or specific purposes (e.g. while teaching).7,14–24 Few people with thoracic paraplegia walk as their primary form of mobility.
People with motor incomplete lesions and lumbosacral paraplegia. Most people with motor incomplete lesions (i.e. ASIA C, D or E) and lumbosacral paraplegia can walk for at least limited distances. The usefulness of walking largely depends on the extent of paralysis because this determines the need for orthoses and aids, and the speed and energy cost of walking.25 As a guiding rule, people with composite ASIA lower extremity motor scores less than 20/50 generally use wheelchairs as their primary form of mobility.19,25 They may, however, walk around the home or exercise with orthoses and aids.26,27 Walking is only a realistic and functional alternative to a wheelchair if people have at least sufficient strength in one leg to avoid the need for bilateral splinting of the ankles and knees with knee–ankle–foot orthoses.4,19,28 People with ASIA lower extremity motor scores more than 20/50 generally attain the capacity for community ambulation and are capable of walking at reasonable speeds (e.g. 1.0 m.sec–1; this compares to a comfortable walking speed of between 1.0 and 1.7 m.sec–1 for able-bodied individuals). The ability to hitch and control the pelvis increases the likelihood of attaining a functional level of ambulation.4,6 People with incomplete tetraplegia who are dependent on walking aids generally require more strength in their lower extremities than those with paraplegia in order to adequately compensate for their upper limb weakness.26
Any degree of lower limb paralysis clearly makes walking more difficult than normal. The more extensive the paralysis the more difficult walking becomes and the more likely success will be limited by upper limb weakness, lack of proprioception, excessive weight, or presence of spasticity or contracture.6,29,30
People may be able to walk effectively in one context but not in another. For example, a person who is capable of walking unencumbered across the floor of a physiotherapy gymnasium will not necessarily be able to carry bags from a supermarket to a car park. Effective walking depends on attaining some level of automaticity so that attention can be simultaneously directed at other activities while upright.31,32 It also depends on the ability to ascend slopes, stand up from sitting, and negotiate stairs and uneven ground.13,33 People eventually tend to choose the most practical and functional way of moving about in the community and they will not opt to walk unless it is as efficient, fast and functional as getting about in a wheelchair. Some are surprised to find that, in many environments, a wheelchair is an efficient form of transport. Of course some environments, such as rugged and mountainous places in developing countries, have such poor wheelchair accessibility that walking provides the only option for mobility.
There are and always will be people who defy the odds and attain remarkable levels of upright mobility despite severe paralysis and dependency on extensive orthotic support and aids. Children generally attain a higher level of upright mobility than adults although it is not clear whether this is solely due to the biomechanical advantages of being a child34,35 or the extensive support provided by children’s schools, parents and therapists.7,23,36
Standing for therapeutic purposes
The most convenient way of enabling patients with tetraplegia to stand is with a tilt table. Alternatively, electronic standing wheelchairs and frames can be used.37,38 The patient is strapped to the tilt table, standing chair or frame to prevent knee, hip and trunk flexion (see Figure 6.1). Patients with thoracic paraplegia and good upper limb strength can stand in relatively simple frames which block knee flexion. A strap behind the hip prevents hip flexion (see Figure 6.2). They can also use knee extension splints and pull up into standing between parallel bars (see Figure 6.3). At home, appropriately placed benches or sinks can be used.

Patients can stand without a strap behind the hips provided they push down through the hands to hold the body upright. Alternatively, they can lean backwards and hyper-extend the lumbar spine. This posture creates a passive hip extension torque that keeps the trunk upright despite paralysis of the hip extensor muscles (see p. 113).
The decision about whether to continue standing after the initial rehabilitation phase is more complex. Some authorities recommended that patients stand for at least 20 minutes, three to five times a week, on an ongoing basis. It is often claimed that regular standing improves psychological status,39,40 renal function41 and bone density.17,42–46 It is also said to help spasticity,47,48 orthostatic hypotension49 and joint range of motion.6,17,50–52 While there is a good theoretical basis to believe that standing has all these beneficial effects, sound evidence is lacking.37,53 Most work directed at quantifying the benefits of regular standing has been carried out in children6,54 or is inconclusive.55,56 The important question as to whether possible benefits justify the inconvenience, effort and cost is yet to be answered.23 Possibly, to reap therapeutic benefits, patients need to stand more frequently and for longer periods than is generally recommended.
Walking with thoracic paraplegia
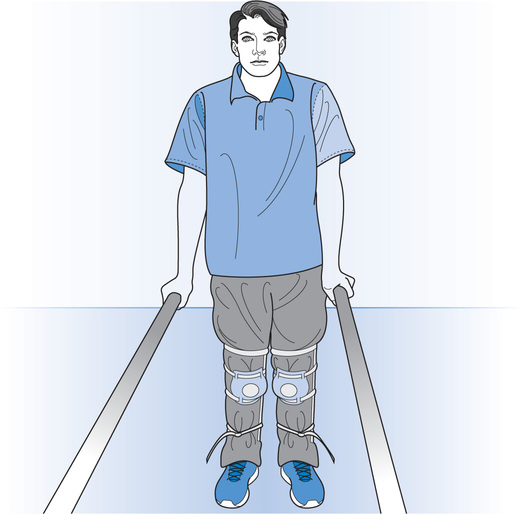
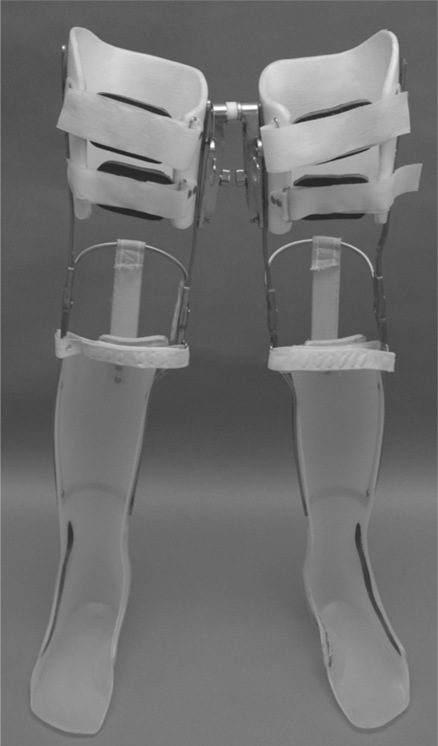
Bilateral knee–ankle–foot orthoses
Bilateral knee–ankle–foot orthoses provide the cheapest and simplest way to enable patients with thoracic paraplegia to walk. There are various types of knee–ankle–foot orthoses but most incorporate double metal uprights bars and plastic moulded calf and thigh sections (see Figure 6.4).57 They all stabilize the knee in full extension and ankle in 5–10° dorsiflexion.6 Different types of knee joints can be used. Most can be unlocked so the knee can be flexed when sitting.57,58
Knee–ankle–foot orthoses only compensate for paralysis around the ankle and knee. They provide no stability around the hip or trunk, nor do they provide assistance for hip flexion during swing. They do not stop the pelvis from tilting downwards on the unweighted swing leg. This, combined with fact that the knee is held in extension, makes foot clearance during swing difficult. To overcome problems of foot clearance patients exert downward forces through crutches to ‘hitch’ (elevate) the pelvis on the swing leg or depress the shoulders.26,59 Foot clearance during swing is particularly problematic when walking up slopes or stairs.
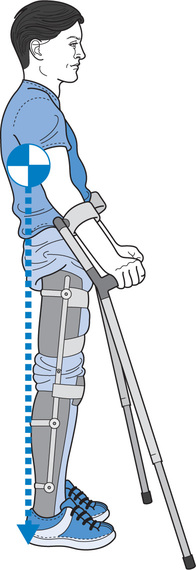
Walking with knee–ankle–foot orthoses
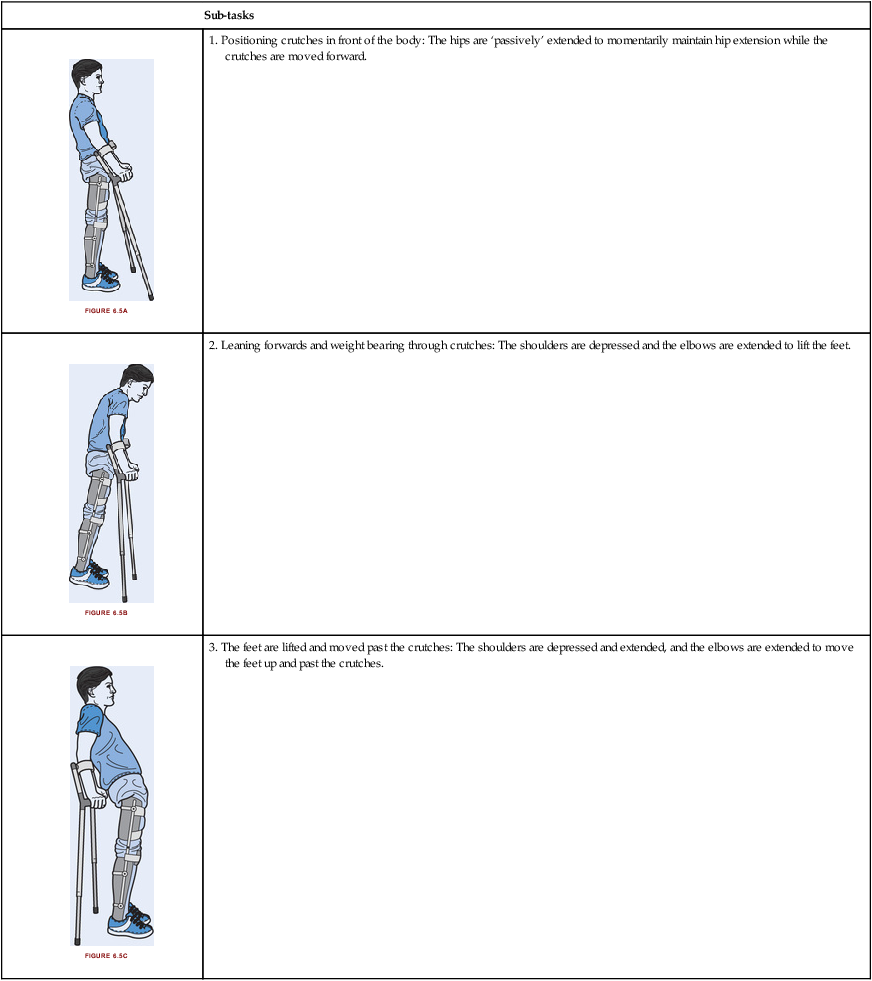
The jumping gait pattern (see Table 6.1) involves placing both crutches in front of the feet and then swinging both legs through simultaneously15,60 by extending the shoulders. If the feet are moved up to the crutches the gait is called a ‘swing-to’ pattern. Alternatively, if the feet are moved past the crutches the gait is called a ‘swing-through’ pattern.61 Both swing patterns are physically demanding17,19,26 but provide a quick way of getting around (up to 1.8 m.sec–1 in children62). In contrast, the reciprocal gait pattern involves moving the feet forwards one at a time. Each leg is swung forwards by elevating the pelvis on the swing side and circumducting the leg (i.e. hip abduction and external rotation combined with pelvic elevation). One crutch is placed in front of the body while the opposite foot is moved forwards. This is a relatively slow way to ambulate.
Table 6.1
A patient with thoracic paraplegia walking with a swing-through gait pattern using bilateralknee–ankle–foot orthoses60
| Sub-tasks | |
 | 1. Positioning crutches in front of the body: The hips are ‘passively’ extended to momentarily maintain hip extension while the crutches are moved forward. |
 | 2. Leaning forwards and weight bearing through crutches: The shoulders are depressed and the elbows are extended to lift the feet. |
 | 3. The feet are lifted and moved past the crutches: The shoulders are depressed and extended, and the elbows are extended to move the feet up and past the crutches. |
Hip extension can be maintained without using the hands by leaning the trunk backwards and extending the lumbar spine. This positions the centre of mass of the trunk and head behind the hips, creating a torque which passively extends the hips (see Figure 6.6). Excessive hip extension is prevented by the soft tissues spanning the front of the hips. If the centre of mass of the trunk and head moves anterior to the hips with the crutches off the ground, the hips will rapidly flex. The feet can only remain flat on the ground when patients lean backwards if the ankles are dorsiflexed. For this reason the ankles of knee–ankle–foot orthoses are commonly fixed in 5–10° dorsiflexion.58 Slight modifications to ankle position can make a substantial difference to the ease of standing.58
Moving from sit to stand with knee–ankle–foot orthoses
It is difficult to get from sitting to standing with knee–ankle–foot orthoses (see Table 6.2). Most patients place the hands behind the body and lift up into standing with the knee joints locked in extension. The centre of mass must initially move forwards over the feet. However, the feet cannot be tucked under the chair because the knees are extended. Consequently, the centre of mass needs to move much further forward than it would otherwise if the knees were flexed. The centre of mass cannot be moved sufficiently forward through hip flexion alone. Instead the centre of mass is moved forwards by pushing backwards and downwards through crutches or the arms of a chair. Not surprisingly, patients require good upper limb strength.
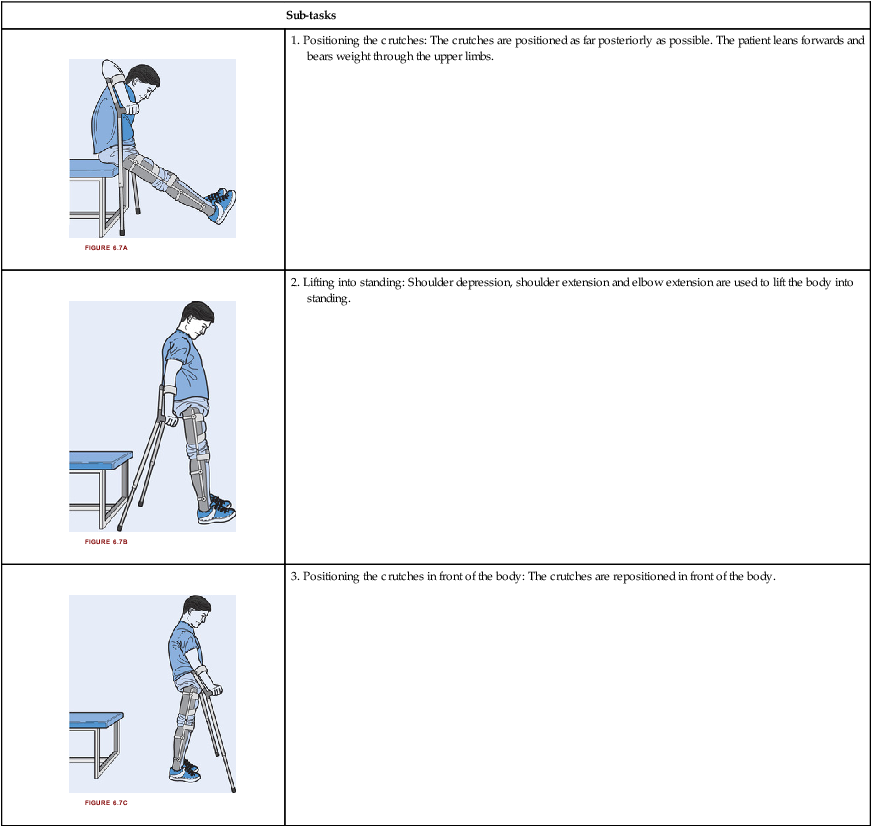
Table 6.2
A patient with thoracic paraplegia moving from sitting to standing using bilateral knee–ankle–foot orthoses
| Sub-tasks | |
 | 1. Positioning the crutches: The crutches are positioned as far posteriorly as possible. The patient leans forwards and bears weight through the upper limbs. |
 | 2. Lifting into standing: Shoulder depression, shoulder extension and elbow extension are used to lift the body into standing. |
 | 3. Positioning the crutches in front of the body: The crutches are repositioned in front of the body. |
There are other strategies which can be used to stand up. For example, some patients find it easier to stand up using the armrests of a chair, rotating in to face the chair as they stand. In this latter technique, patients end up facing the chair in a semi-standing position before grasping walking aids to move into an upright position.63 It is also possible to stand up with the knee joints unlocked. This requires very good upper limb strength to lift the body into standing. Weight cannot be borne through the feet until the knee joints are locked. A special type of ratchet joint can be built into orthotic knee joints to prevent knee collapse and enable weight to be borne through a flexed knee.6 These type of joints are not widely used because they are expensive and add weight and complexity to orthoses. Electrical stimulation of the quadriceps and hip extensor muscles can overcome some of these problems and help patients move from sitting to standing.64
Hip–knee–ankle–foot orthoses
Hip–knee–ankle–foot orthoses are bilateral knee–ankle–foot orthoses joined together with hip joints.6 The orthotic hip joints can be placed between the legs or connected laterally to a pelvic or lumbar band or a lumbosacral corset. Orthoses which include extensive trunk bracing are sometimes referred to as trunk–hip–knee–ankle–foot orthoses.36
By joining two knee–ankle–foot orthoses together, hip–knee–ankle–foot orthoses substitute for paralysis of the hip abductor muscles and provide medio-lateral stability during stance. In addition, they prevent the pelvis from tilting downwards on the unweighted swing leg. This assists foot clearance during swing and reduces the need for the upper limbs to lift the swing leg. However, the torques tending to tilt the pelvis downwards during swing are large, especially in heavy patients. To resist these torques, hip–knee–ankle–foot orthoses need good lateral rigidity.5,34,35,65–67 If the orthosis is insufficiently rigid, swing leg clearance is difficult.
The three most common types of hip–knee–ankle–foot orthoses are the hip guidance orthosis (HGO; see Figure 6.8), the reciprocating gait orthosis (RGO; see Figure 6.9) and the medial-linkage orthosis (MLO; see Figure 6.10).6,11,24,64,65,68–75 Various types of hip and knee joints can be used in all three orthoses.7,65,73,76–78 A summary of each is given below.
The hip guidance orthosis
The hip guidance orthosis, also called the ParaWalker, was first introduced for children with spina bifida in the 1970s (see Figure 6.8).79 It consists of two knee–ankle–foot orthoses attached to a rigid body brace with laterally placed hip joints. The hip joints are low friction and restrict flexion and extension, although they can be released to enable sitting. During the swing phase of gait, the leg flexes like a pendulum. That is, hip flexion is achieved solely by the effects of gravity on the unweighted leg. Gravity will only act to flex the hip when the leg is extended with the mass of the leg behind the hip joint.80
The reciprocating gait orthosis
The reciprocating gait orthosis joins two knee–ankle–foot orthoses to a trunk corset with laterally placed joints (see Figure 6.9). A key feature of the reciprocating gait orthosis is the coupling together of the hip joints, preventing bilateral hip flexion in stance. The hip mechanism was designed so hip extension on one leg could assist hip flexion on the other leg when stepping. However, the effectiveness of this mechanism may be overstated.81 The hip joints can be unlocked to flex simultaneously.10,82,83 This is important for sitting.
Early versions of reciprocating gait orthoses coupled the two hip joints together with cables.84 The cables were attached under high tension so that forces from extension in one leg were transmitted to flexion of the other. In more recent years a pivot bar has replaced the cables.85 The pivot bar is positioned centrally and at the back of the corset in the lumbar region.80 Reciprocating gait orthoses incorporating pivot bars are called isocentric reciprocating gait orthoses. A variation is the advanced reciprocating gait orthosis.65
The medial-linkage orthosis
The medial linkage orthosis, also known as the walkabout orthosis, has a hinge-like joint positioned between the legs (see Figure 6.10). The joint limits hip flexion and extension but does not mechanically assist either. Instead, gravity flexes the hip and moves the unweighted leg forward. Hip extension is achieved by leaning the trunk backwards and extending the lumbar spine (see Figure 6.6). Consequently, even slight loss of passive hip extension can be a problem, increasing patients’ reliance on their upper limbs to hold the trunk upright. The medial-linkage orthosis is aesthetically more appealing than other types of hip–knee–ankle–foot orthoses but it provides a slower and more energy-consuming gait.10,11,71,72,86,87
Walking with hip–knee–ankle–foot orthoses
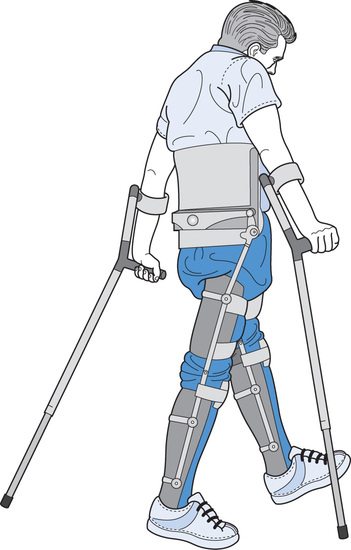
Typically, patients use a reciprocal gait pattern with either crutches or a frame.24,65,68,73,74,81,83,88,89 There are various strategies used to walk depending on the type of orthosis and walking aid, and extent of trunk paralysis; however, the underlying principles of all strategies are similar. Initially, weight needs to be shifted from the back leg forwards and laterally onto the front leg. This is achieved by pushing the body forwards and laterally through a posteriorly-placed walking aid (see Figure 6.11). Further unweighting of the back leg is achieved by shoulder depression and pelvic hitch. Once all weight is removed from the back leg, it can be moved forwards either in response to gravity or in response to trunk extension.81,90
Moving from the floor or a seated position into standing with hip–knee–ankle–foot orthoses is done in a similar way to standing up with knee–ankle–foot orthoses (see Table 6.2). However, the additional weight and bulk of hip–knee–ankle–foot orthoses makes both these tasks particularly difficult and most patients require assistance.7,8,70
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree