Chapter 15 Congenital Elbow Disorders
Introduction
Congenital elbow disorders can involve either the soft tissues, e.g. arthrogryposis, bone e.g. radio-ulnar synostosis, or the joint itself, producing instability. Ogino and Hikino1 classified congenital elbow deformities into three types based on the presence of associated anomalies:
Congenital elbow synostosis
Background and aetiology
A single mesodermal condensation is seen along the long axis of the limb bud at week 4. Pre-chondrogenic cells in these condensations then differentiate into chondrocytes under the influence of bone morphogenetic proteins (BMPs). Sequential chondrification and ossification subsequently follow, resulting in the formation of bones and joints in the upper limb. The elbow becomes visible at 34 days. The humerus, radius and ulna are continuous with each other and are joined by a common perichondrium at 5 weeks of gestation. The forearm is in a neutral position and subsequently by the 6th week condensation of the tissue separates the cartilaginous anlage of the three bones. The forearm pronates at the 8th week due to growth discrepancy between the arterial tree and the radius.2
Although most cases are sporadic, a positive family history in some cases of congenital radio-ulnar synostosis has suggested a genetic component. Inheritance may be autosomal dominant or recessive. Some of these cases, especially humeroradial synostosis may be syndromic as they are associated with other congenital syndromes like Carpenter syndrome, Apert syndrome, Antley–Bixler syndrome, Roberts syndrome,3,4 arthrogryposis and Cornelia de Lange syndrome. Chromosomal abnormalities such as Klinefelter syndrome5 may be associated with radio-ulnar synostosis.
Classification
Classically, synostosis has been divided anatomically into humeroradial, humero-ulnar, humeroradio-ulnar and radio-ulnar. Further subdivisions in the humeroradial group have been added based on the anatomical differences, namely classes 1 and 2:6
Table 15.1 Synostosis classification
| Anatomical | Humeroradial |
| Humero-ulnar | |
| Radio-ulnar | |
| Aetiological | Class 1 – bone hypoplasia group with synostosis of elbow |
| Class 2 – joint maldevelopment group with synostosis of elbow |
Proximal radio-ulnar synostosis has also been classified on the basis of the radiological appearance. Mital7 presented a two-group classification system:
This was modified by Cleary and Omer8 to a four-group system:
An aetiological classification of elbow synostosis was proposed by McIntyre and Benson.9 They divided synostosis around the elbow into two classes:
All the three anatomical types can occur within each class, may be sporadic or familial and, if familial, may be inherited as an autosomal dominant or recessive trait. The class I group is associated with musculoskeletal abnormalities outside the affected limb in 25–55% of cases.10 Class II familial cases may be syndromic and associated with multiple synostosis syndrome, Pfeiffer syndrome, Apert syndrome and Antley–Bixler syndrome.
Presentation, investigations and treatment options
Proximal radio-ulnar synostosis
Two major surgical procedures are available for this condition. One involves a mobilization procedure to separate the radio-ulnar synostosis and restore forearm rotation,11,12 while the other is an osteotomy to correct the forearm position, making it more suitable for the patient’s activities of daily living.
Another alternative that has been proposed to achieve and maintain motion is the swivel prosthesis designed by Kelikian and Doumanian.13 This is a stainless steel implant that is inserted into the intramedullary canal of the radius to restore motion. However, although it has been used in four cases of post-traumatic proximal radio-ulnar synostosis with good results, it has been shown to have poor results in cases of congenital radio-ulnar synostosis.14
Surgical techniques and rehabilitation
Mobilization procedure11
Kanaya described this procedure in the following four steps:
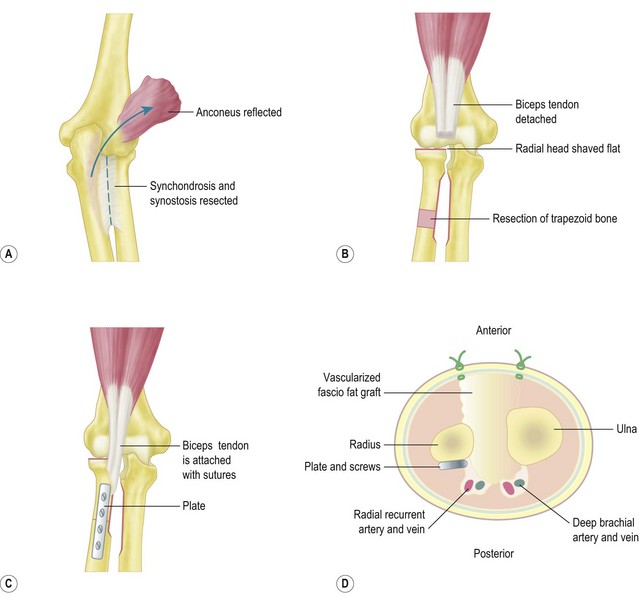
Vascularized fascio-fat graft
The wounds are closed and an above-elbow cast is applied with the forearm in neutral rotation and the elbow in 90° of flexion. The cast is maintained for 4 weeks (Fig. 15.1).
Rotational osteotomy
An alternative procedure to mobilize the synostosis is a rotational osteotomy.15,16
These have been described at two sites in the diaphysis of the radius and ulna17,18 or at one site in the distal diaphysis of the radius.19,20 An osteotomy at the synostosis is extremely complex, whereas an osteotomy at two sites in the diaphysis of the radius and ulna is easier, with fewer reported complications.
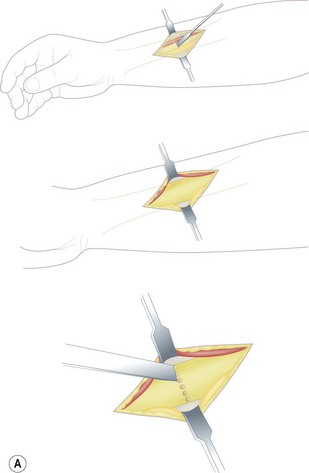
A single osteotomy of the distal radius is performed through a 4 cm skin incision made distally on the radiovolar aspect of the distal forearm. The diaphysis of the radius is exposed and the superficial radial nerve and the radial artery are identified and retracted ulnarward. A sharp longitudinal incision is made on the periosteum and reflected atraumatically from the radius to preserve the longitudinal continuity of the periosteum. Several drill holes are made in the transverse line to the radius using a K-wire and a transverse osteotomy is performed using a chisel (Fig. 15.2A). A meticulous periosteal repair is then performed and the distal forearm maximally supinated and immobilized in an above-elbow plaster cast (Fig. 15.2B).
Outcome including literature review
Operative procedures used in the treatment of congenital radio-ulnar synostosis fall into two major groups. Group 1 procedures are designed to restore rotation and remove the synostosis, while group 2 procedures restore the forearm to a fixed functional position. Several authors have reported poor results after separation of the synostosis and interposition of fat, muscle or silicone.11,21–23
Kanaya et al performed the mobilization procedure in seven boys (average age 8 years 2 months) who had isolated proximal radio-ulnar synostosis. All seven children had a dislocation of the radial head preoperatively. A shortening-wedge osteotomy of the radius was performed in four patients at the time of the index procedure, while in three patients the radial head was manually reduced without an osteotomy. The radial head subsequently redislocated in the latter three patients and one of them had an osteotomy 2 years and 8 months after the index procedure to reduce and maintain the radial head alignment. At follow-up the total range of forearm rotation achieved averaged 71° with average supination of 26° and average pronation of 45°. There were no cases of reankylosis at an average follow-up of 4 years 4 months.12 The group who had a radial osteotomy in addition to the index procedure had an average arc of 83° of forearm rotation compared to the second group, who had an average arc of rotation of 40°.
Kamineni et al24 have described a new technique of restoring forearm rotation in post-traumatic proximal radio-ulnar synostosis. This involves resecting a 1 cm thick section of bone from the proximal radial shaft distal to the synostosis. They performed this surgery on seven patients and reported an improvement in forearm rotation from an average fixed pronation of 5° to an average arc of 98°.
Osteotomies to achieve a more functional forearm position are suitable for patients with marked pronation deformity. Green and Mital16 have reported the best results with derotational osteotomies through the fusion mass. This has the advantages of achieving a better correction and rapid healing of the osteotomy owing to the good coaptation of the divided ends. In their series results were excellent in 50%, good in 33%, fair in 6% and poor in 6%. Ogino and Hikino1 also favoured an osteotomy through the fusion mass, but recommended resection of 0.5 cm of bone at the osteotomy site in order to shorten the forearm. All the patients in their series had complete relief of symptoms.
Goldner and Lipton recommended derotation in the distal forearm to minimize circulatory problems.25 The osteotomy was done in the distal radius alone for younger patients and in both the radius and ulna in older patients.
A single osteotomy technique distal to the synostosis was reported by Kashiwa et al in 199919 and subsequently modified by Fujimoto et al.20 This osteotomy is performed at the distal radial diaphysis. Fujimoto presented the results of this osteotomy in three patients (four forearms) with congenital radio-ulnar synostosis. Bony union was achieved in all cases. The period of immobilization in plaster varied from 6 to 9 weeks. All patients achieved good correction, with functional improvement in activities of daily living.
Bolano26 has shown good results with an osteotomy and gradual correction of the rotation using a ring fixator. This technique is useful as there is less risk to the neurovascular structures and it has the added advantage of allowing the patients to choose the most functional position of their forearm.
The ideal position to place the forearm after the osteotomy depends on several factors. If the synostosis is bilateral and both hands are in pronation, Simmons and Waters27 recommended 20° of pronation in the dominant hand and a neutral position for the non-dominant. In unilateral cases, Green and Mital16 recommended 20–25° of supination as the supinated forearm can attain some amount of functional pronation by internal rotation, flexion and abduction at the shoulder. Ogino and Hikino1 from Japan recommend at least 70° of palmar supination, especially in the non-dominant hand, to enable the use of chopsticks by their patients. Hence the amount of angular correction is dependent on customs, dominant hand and bilaterality.
Complications
Following excision of a synostosis and mobilization of the forearm, reankylosis can occur, giving poor results21,22 and a risk of radial head dislocation and posterior interosseous nerve palsy.
Complications reported following derotational osteotomies include neurovascular compromise. Green and Mital reported one case of severe Volkmann’s contracture and one case of posterior interosseous nerve palsy from their series of 13 patients. Ogino and Hikino1 reported two posterior interosseous nerve palsies in 13 operations, both of which spontaneously recovered.
Simmons and Waters27 reported a 36% complication rate with loss of correction in three out of 21 children and an 18% incidence of vascular compromise. A decreased range of elbow movement has also been reported.