Chapter 85 Congenital Deformities of the Knee
Congenital Dislocation of the Knee
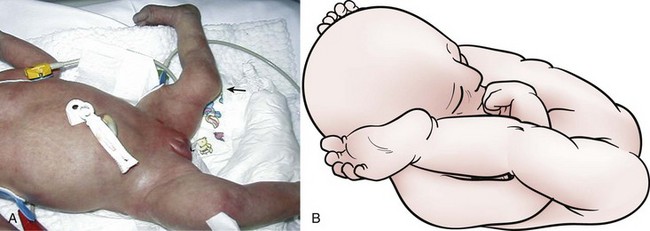
Few orthopedic birth abnormalities are as dramatic and obvious as congenital dislocation of the knee (CDK; Fig. 85-1A). Those unfamiliar with the deformity may describe the extremity as having the knee on backward because of the unstable excessive hyperextension combined with an element of angular deformity. CDK is rare, being only about 1% as common as congenital hip dislocation.28 Even if the milder form of congenital hyperextension deformity is included as CDK, the incidence is still less than 0.1%.8 It can be diagnosed prenatally by ultrasound.15
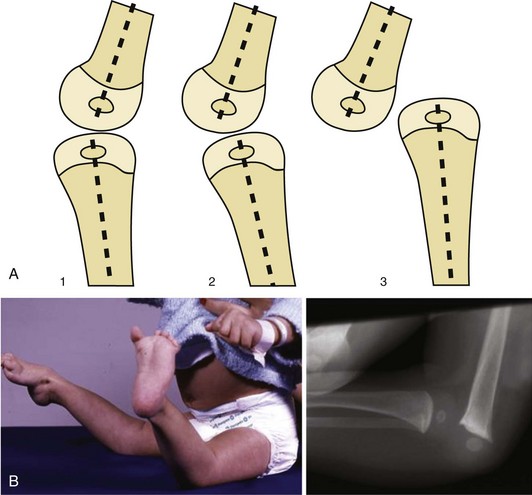
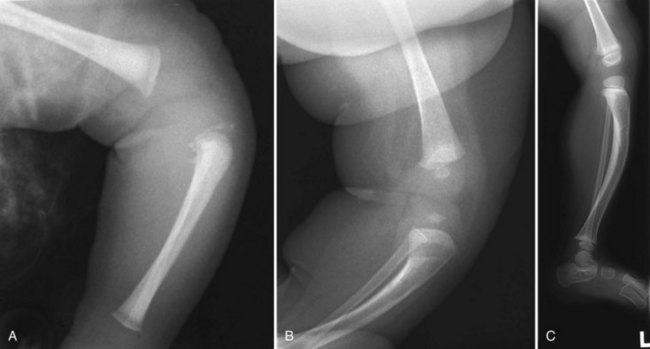
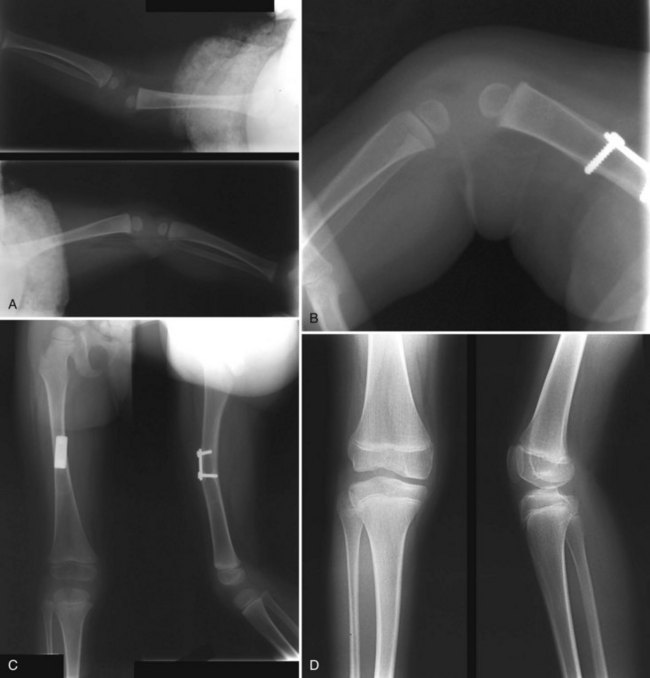
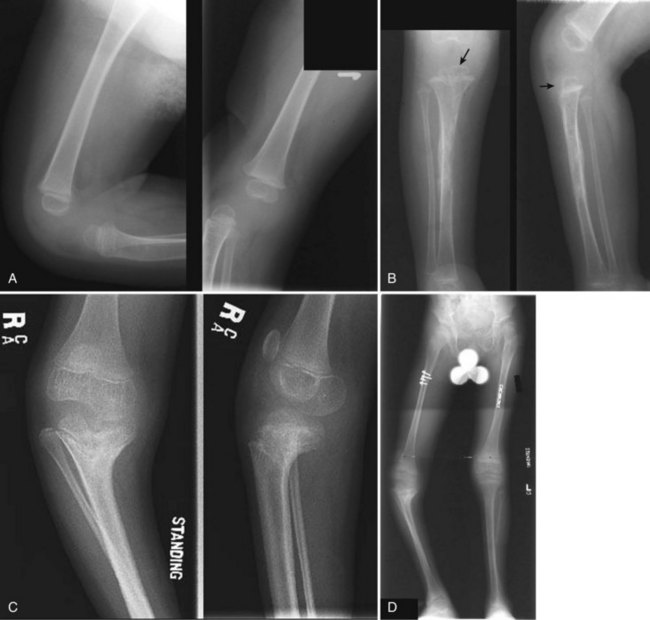
Clinically, the hyperextension deformity is unmistakable, with the femoral condyles often being prominent on the posterior distal thigh. The foot may present at the baby’s face or shoulders, and this marked hyperflexion of the hip (see Fig. 85-1B), reflecting the positioning in utero,48 raises the suspicion of concomitant congenital hip instability. Radiographically, the relationship between the distal femur and proximal tibia should be determined on a true lateral radiograph of the knee, defining that relationship as hyperextended, subluxated, or dislocated (Fig. 85-2). Next, the degree of passive flexion of the knee is important to determine prognosis, because it may be immediately apparent that the knee will flex and reduce with gentle stretching of the quadriceps, in which case the deformity can be classified clinically as grade 1 congenital hyperextension.10,39 On the other hand, any flexion of the knee may be impossible, and the tibia, which is anteriorly translated in the resting position, may subluxate laterally on the femur when more vigorous flexion is attempted, indicating a grade 3 irreducible dislocation. (Fig. 85-3). The latter is always associated with significant quadriceps fibrosis and shortening, which may be the cause of the deformity.43 An intermediate degree of contracture, a grade 2 subluxation, may be noted when the knee will not flex beyond neutral extension, but the femoral and tibial epiphyses are in contact and do not subluxate readily when flexion is attempted.

Figure 85-3 A, Anteroposterior radiographs of a 3-year-old boy with Larsen syndrome and bilateral CDK. B, Clinical appearance, grade 3 dislocation on the left. C, The right knee reduces with flexion, grade 1 (see Fig. 85-14). D, The ACL is congenitally absent.
Equally important at the initial evaluation is the search for associated anomalies and syndromes. Both ipsilateral hip dysplasia and clubfoot are present 70% and 50% of the time, respectively,5,29 with other anomalies of the upper extremity, face, gastrointestinal (GI), and genitourinary (GU) systems not uncommon. Bilateral CDK is almost always syndromic, most commonly associated with laxity syndromes such as Larsen, Beals, or Ehlers-Danlos syndrome. Neurologic conditions, such as arthrogryposis or spinal dysraphism, may have bilateral CDK, or may have one extended (dislocated) knee and one with a flexion deformity. Whether isolated or syndromic, abnormal fetal positioning is likely the common mechanical cause. Lack of movement because of neuromuscular conditions (e.g., arthrogryposis), or hyperlaxity can easily be invoked as causative once the abnormal position (see Fig. 85-1B) occurs, with quadriceps fibrosis and atrophy developing when the knee cannot move and the muscle shortens in the extended position. Hypoplasia of the patella and contracture of the iliotibial band probably result from the same lack of joint and muscle movement.
Ligamentous laxity, with elongation, insufficiency, or absence of the cruciate ligaments, has long been known as a complicating feature of CDK,4,10,32,50 although it has been downplayed in importance in some reports.5,55 Cruciate absence is actually typical of bilateral, syndromic cases (see Fig. 85-3D), and should be addressed as part of the comprehensive surgical management (see later). Conversely, isolated CDK (with or without ipsilateral hip or foot deformity) is often unilateral, and once reduced the knee is relatively stable (anterior cruciate ligament [ACL] present), and thus can been termed stiff CDK as opposed to the lax syndromic variety.
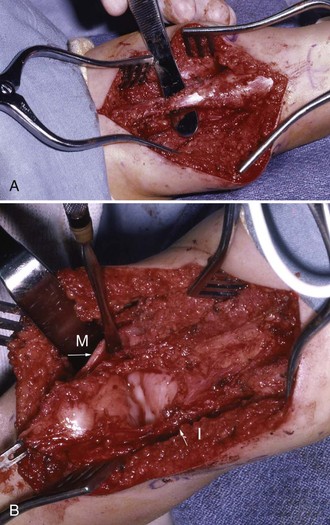
Other pathologic findings in grade 3 CDK include anterior subluxation of the posterolateral and posteromedial periarticular tissues, including hamstring tendons and the iliotibial (IT) band, because of the chronic hyperextension and anterior translation of the tibia on the femur (Fig. 85-4).5,10,29,64 The suprapatellar pouch may be atrophic or obliterated, with adhesions between the hypoplastic patella and the femur and IT band. All these intra-articular abnormalities will need to be addressed surgically in the irreducible CDK.
Treatment
Nonoperative Management
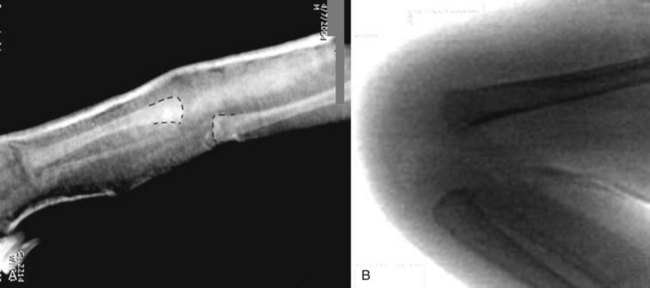
Nonoperative treatment should begin as soon as possible in infancy. After determining the radiographic position (see Fig. 85-2A), initial flexibility of the quadriceps contracture is assessed by applying gentle traction to the tibia and attempting flexion of the knee.34 The tibia, if anteriorly located, engages the distal femur and translates posteriorly with traction and, as the knee is flexed, a stable articulation can be palpated. In simple hyperextension cases, this may be readily achievable and usually maintained with an anterior plaster slab or a long-leg cast. The latter is actually more difficult to apply in the infant and maintain reduction. Obviously, forceful manipulation is contraindicated because of risk of pressure damage to cartilaginous epiphyses or fracture-separation of the proximal tibial physis (Fig. 85-5).59 Serial manipulations and splinting in increasing flexion proceed until the knee will flex more than 90 degrees, at which time a removable plastic splint can be used to maintain reduction while allowing some active motion. Alternatively, if the patient also has an ipsilateral CDH, the knee can be maintained in a Pavlik harness while the hip is simultaneously addressed.
In knees with more severe quadriceps contracture preventing effective gradual flexion, femoral nerve block or botulinum toxin can been effective. Botox injection of the quadriceps has the added advantage of longer term paralysis of the quadriceps, allowing gradual stretching to occur, even when initial flexibility seemed unfavorable for nonoperative reduction (Fig. 85-6). A trial of nonoperative management, with or without adjunctive neuromuscular blockade, is appropriate initial treatment in infants up to 12 months of age.
Surgical Management
Surgical treatment is indicated for cases not responding to nonoperative means, and has been advocated for infants as early as 6 months of age.4,5 Although earlier reduction of the knee may provide greater potential for remodeling of articular surfaces, patients as old as 4 years have had successful initial reduction, and patients as old as 16 years have had late gross instability with reducible but recurrent dislocation addressed. Considering the current use of femoral shortening to achieve reduction (see later), the earliest age for surgery should be when the surgeon thinks that the femur is robust enough to accept meaningful internal fixation to stabilize a shortening osteotomy.
Reduction and Flexion With Femoral Shortening
Classic surgical treatment of CDK has invariably used extensive V-Y quadriceps tendon lengthening (Fig. 85-7; see Fig. 85-4) to gain flexion, and hence reduction, of the joint. Outcomes of such lengthenings are poorly documented in many series, because simple documentation of reduction and reporting of passive range of motion is sometimes all that is recorded. Because many patients have other anomalies and comorbidities affecting outcome, the functional results of the knees themselves have rarely been reported. Actually, the extensive lengthening invariably leads to weakness and an extensor lag, and the extensive dissection required to obtain such length produces additional fibrosis, limiting flexion. Finally, wound healing over the anterior knee surface may be compromised because of ischemia produced by the flexion stretching the contracted anterior skin (see Fig. 85-7C).

Figure 85-7 A, Classic V-Y quadricepsplasty. B, The resulting repair of the quadriceps tendon (arrows) is tenuous at best because of the extensive lengthening required to gain knee reduction (same patient as in Fig. 85-4). C, Wound dehiscence-slough as a result of skin necrosis from knee flexion.
(A from Curtis B, Fisher R: Congenital hyperextension with anterior subluxation of the knee; surgical treatment and long-term observations. J Bone Joint Surg Am 41: 255, 1969.)
In addition to the quadricepsplasty, arthrotomy must be performed to mobilize the anteriorly subluxated medial and lateral periarticular structures and allow them to relocate to their normal anatomic position as the knee is flexed (see Fig. 85-4B). However, once the knee is reduced in flexion, the redundant posterior capsule resulting from that maneuver has rarely been addressed (by capsulorrhaphy), thus inviting a redislocation into the same incompetent posterior space. The irrationale of this oversight can be easily appreciated if one considers that a late open reduction of a congenital hip dislocation would never be completed without performing a capsulorrhaphy to obliterate a potential space into which the femoral head could redislocate. Thus, if the ACL is also congenitally absent in a CDK reduced without capsulorrhaphy, it is hardly surprising that chronic hyperlaxity-instability of the knee at a minimum, and frank redislocation at the other extreme, would be the common outcome of knees treated by such an approach, especially if flexion is limited by the scarred fibrotic quadriceps muscle, which has been extensively dissected.
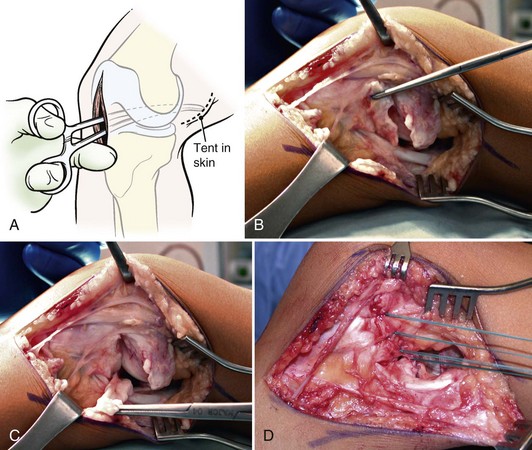
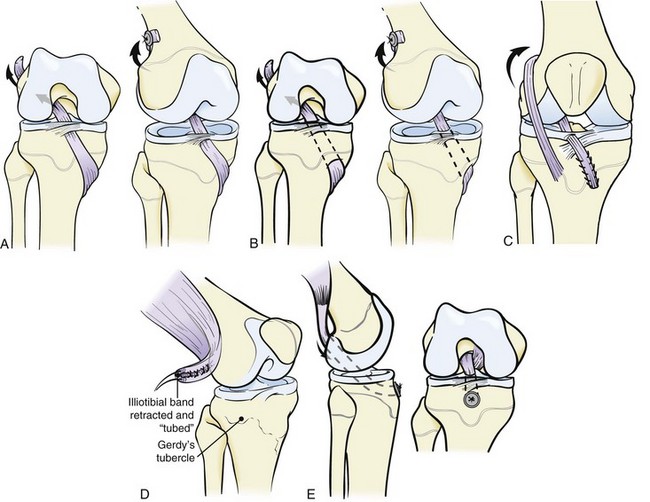
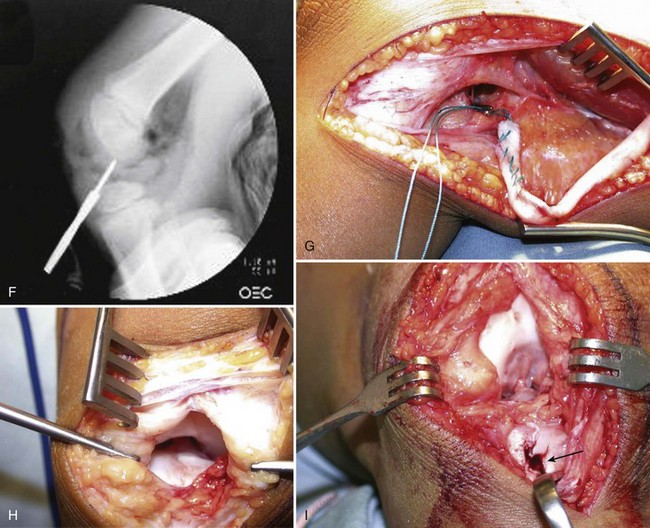
As a result, we strongly recommend that V-Y quadricepsplasty should be abandoned in favor of femoral shortening to minimize quadriceps dissection and weakening (Fig. 85-8). Acute femoral shortening decompresses the anterior skin and allows knee flexion without surgical lengthening of the muscle. The operative procedure begins with a lateral parapatellar arthrotomy incision that is extended proximally along the lateral femur to allow mobilization of the distal contracted lateral tissues (IT band, released from its distal insertion, and vastus lateralis from intermuscular septum) and provide subperiosteal access to the supracondylar region for the bone shortening (Fig. 85-9). The quadriceps tendon, patella, and patellar tendon are mobilized (skeletonized) as a continuous longitudinal structure via a medial arthrotomy to allow sharp dissection and elevation of medial periarticular structures (pes tendons), which are subluxated anteriorly. The intercondylar notch is inspected for the presence or absence of the anterior cruciate ligament. Once the femur is acutely shortened and plated—usually approximately 2.0 to 2.5 cm is removed—the knee will usually reduce with flexion, and the only repair necessary is to stabilize the patellar mechanism in the intercondylar groove, generaally by medial imbrication and advancement of the vastus medialis obliquus (see Fig. 85-9E and F). The lateral release is repaired only to the extent of covering the internal fixation.
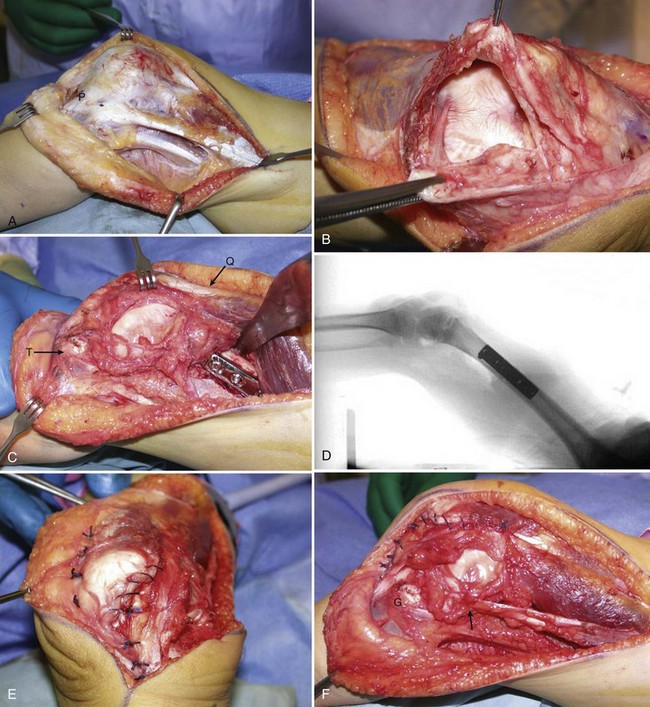
Figure 85-9 A, Lateral knee, distal femoral exposure. The tibia is dislocated posterolaterally (same patient as in Fig. 85-3, left knee). The IT band and biceps are seen prior to release of the former from its insertion. Anteriorly, the patellar tendon is marked. B, Medial arthrotomy. The vastus medialis and medial retinaculum are being separated from the quadriceps tendon (inferior clamp). C, The femur has been shortened and plated. The tibia (T) now reduces under direct vision. The quadriceps mechanism (Q) is in continuity. D, Intraoperative radiograph confirming reduction. E, Anterior view of advancement-imbrication of vastus medialis to hold patella centralized (medial to right). F, Lateral view of the imbrication. No attempt has been made to close the lateral arthrotomy. The vastus lateralis covers the plate. Posterolateral capsulorrhaphy has been performed deep to the IT band, which has been reattached to the posterolateral condyle (arrow). Reattachment to Gerdy’s tubercle (G) is both impossible and contraindicated.
Capsulorrhaphy is performed at the posterolateral corner of the lateral femoral condyle by bluntly dissecting the capsule, with the knee flexed, from the more superficial tissues with an elevator. The dissection is simplified once the it band and vastus lateralis have been released and mobilized. The lateral half of the posterior capsule is imbricated proximal to the distal edges following excision of 1 to 1.5 cm of redundant patulous capsule (Fig. 85-10). Shortening of the hamstrings4,5,29 may be done in conjunction with the capsulorrhaphy (and ACL reconstruction, if necessary; see later), but should not be considered a replacement for it.
The posteromedial capsulorrhaphy is performed through a separate 3- to 4-cm incision behind the medial femoral condyle (Fig. 85-11). This incision can be located by placing a blunt instrument from inside the arthrotomy to the posteromedial corner and then cutting down on the instrument tenting the skin. The redundant capsule is dissected free of superficial tissues with the knee flexed, a segment excised, and the imbrication performed (see Fig. 85-11B-D). Following the medial-lateral capsulorrhaphies, the knee should lack 30 degrees or more from full extension; the patient will eventually stretch this iatrogenic flexion contracture in 4 to 6 months.
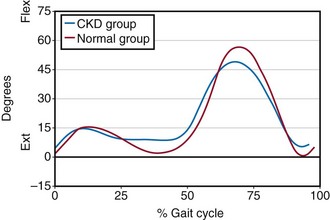
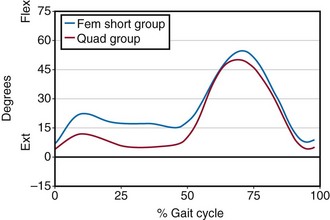
We have recently determined49 the long-term outcomes of seven patients (nine knees) who underwent surgical correction of CDK, with objective criteria that included functional outcome assessment (Lysholm knee questionnaire, Pediatric Outcomes Data Collection Instrument [PODCI]) and three-dimensional kinematic and kinetic gait evaluation. The patients were evaluated as a group and compared based on surgical approach (femoral shortening vs. V-Y quadricepsplasty) at an average of 12-year follow-up. A fairly normal total arc of knee motion (112 degrees) was found, with only one patient from each group demonstrating an extensor lag. Although not statistically significant, the femoral shortening group did demonstrate a better range of motion and Lysholm knee scores when compared with the V-Y quadricepsplasty group. Gait analysis of these patients demonstrated that they walked with more flexion during stance and achieved less peak knee flexion during swing as compared with normal controls (Fig. 85-12). Comparison of the gait between the patients with femoral shortening and V-Y quadricepsplasty showed minor differences in the sagittal plane of the knee, which were consistent with increased stiffness in the quadriceps muscle in the V-Y quadricepsplasty group, consistent with more extensive dissection and resultant fibrosis (Fig. 85-13). Because of the small number of patients, caution must be used in drawing definitive conclusions, but overall it does appear that patients treated surgically for CDK maintain functionality fairly well, with femoral shortening providing improved knee motion and self-reported knee function as compared with V-Y quadricepsplasty.
Anterior Cruciate Ligament Reconstruction
The issue of ACL reconstruction in a young child is controversial, to say the least, but in an unpublished review of 22 knees (14 patients) treated at our institution, with up to 15-year follow-up, the 9 knees that underwent reduction by V-Y quadricepsplasty and no ligament reconstruction were uniformly unstable, had poor quadriceps strength, and required full-time bracing or assistive devices (crutches, wheelchair) for community ambulation. Of these 9 unsatisfactory knees, 8 were in patients with laxity syndromes (predominantly Larsen). The instability was dramatic in that unbraced knees dislocated in the extended position (Fig. 85-14) and, even with bracing, were still unstable, although were usually capable of weight bearing. As a result of this review, an attempt to reconstruct the ACL-deficient knee in the laxity syndrome group seemed justified in an attempt to improve the uniformly unacceptable results of the earlier cases.
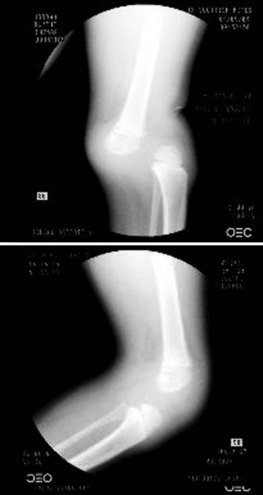
Figure 85-14 Right knee of patient in Figure 85-3 showing dislocation in extension and reduction in flexion.
Although historically there has been reluctance to attempt intra-articular ACL reconstruction in children, because of fear of physeal injury producing deformity and growth arrest from transphyseal procedures, these concerns are gradually relenting because both clinical and experimental studies have shown that this risk may be overplayed. Options include transphyseal and physeal-sparing techniques. Although drilling an anchoring hole across any physis potentially risks injury, the practice of placing smooth pins across physes for periarticular and physeal trauma is well accepted, especially if the fixation is temporary. Logically, a smooth, centrally placed hole across a physis that is filled with a nonosseous (e.g., tendon) material is no more likely to produce growth disturbance than temporary pin fixation because it is an interposition material. Both animal23,61 and clinical studies52 using hamstrings, IT band, or patellar tendon as transphyseal ligament reconstructions have demonstrated knee stability without limb length or angular deformity.
The pes anserine tendons are conveniently used for ACL reconstruction by physis-sparing or physis-crossing techniques.2,40,52,54 In the former, the tendon(s) are left attached at their insertion, detached proximally in the posteromedial thigh, pulled distally and rerouted superficially over the anterior tibial surface, passed under the transverse meniscal ligament to penetrate the knee joint, and passed through the intercondylar notch and over the top of the lateral femoral condyle to be anchored to bone and lateral intermuscular septum (Fig. 85-15A). To place such an ACL substitution closer to anatomic position, the tendon(s) may be passed through a transphyseal drill hole exiting the tibial articular surface at the normal ACL insertion point (see Fig. 85-15B). This method is currently our treatment of choice, regardless of patient age (see later). A 6-mm drill hole has proven technically adequate and noninjurious, with the tendons again anchored over the top of the lateral femoral condyle after traversing the notch. In either technique, care in drilling or passing tendons near the tibial tubercle is most important, because this part of the physis seems most vulnerable. For the same reason, use of the patellar tendon as a ligament substitution is not recommended because of the dissection near this portion of the physis. Several small series2,40,54 have reported restoration of stability, as documented by KT-1000 instrumentation, improvement in Lachman test, and return to previous levels of sport, without physeal injury in immature patients followed up to 5 years.
An alternative ACL reconstruction involves the use of the IT band in a combined intra-articular and extra-articular technique (see Figs. 85-9 and 85-15C). This method, a modification of the procedure described by McIntosh and Darby, has been popularized by Kocher and collagues.35 The technique involves rerouting a central slip of IT band, which is left attached distally to Gerdy’s tubercle, in an over the top position. The tendon is sutured to the lateral femoral condyle to secure its position and routed through the intracondylar notch. The tendon can then exit the knee in the over the front position under the transverse meniscal ligament or it can be routed through a more anatomically positioned drill hole through the tibial articular surface, as described earlier. Good results were reported with this technique in their series of 44 skeletally immature patients, with a 95% graft survival at an average follow-up of 5.3 years. If this technique is used in a child with CDK, it may be helpful to use the anterior third instead of the middle third of the IT band for the reconstruction. This minor modification would allow the most anterior aspect of the IT band to be detached, eliminating this deforming structure of the knee dislocation.
We have previously used the IT band transfer rerouted through the intercondylar notch, as described by Insall and associates.27,58,65 It is readily detached from Gerdy’s tubercle during the approach described for the open reduction of the knee (see Figs. 85-9 and 85-15D), and mobilized proximally to be passed antegrade over the top of the lateral femoral condyle and through the notch prior to completing the capsulorrhaphy. The tubed tendon is then anchored in the proximal tibia through a drill hole within the epiphysis (see Fig. 85-15E), and is tensioned prior to wound closure with the tibia in maximum posterior drawer and the suture tied over a button on the anterior tibial skin or over a suture staple in the tibial metaphysis. The drill hole should be placed with radiographic control to minimize the possibility of oblique transphyseal placement; the tunnel must include the ossification center to provide tendon to bone anchorage. Alternative transphyseal placement through a more vertical, centrally placed tunnel can be attempted if enough length of tendon is available. The postoperative care is the same as for the knee reduction procedure.
The advantage of the Insall technique, as opposed to other ACL substitution procedures, in which the IT band is left attached at its insertion and rerouted as a passive restraint,44,47 is that it is an active transfer in which only the insertion of the tendon is being rerouted. The structure being transferred is also probably one of the deforming forces maintaining the CDK in the first place, so its rerouting should be beneficial. In any case, it will be dissected and mobilized as part of the open reduction-shortening procedure. The disadvantage of the antegrade transfer is poor maintenance of adequate anchorage of the insertion in a diminutive, mostly cartilaginous tibial epiphysis. This has been noted visually in two cases of revision performed for recurrent anterior instability, in which the IT band insertion was severely attenuated 2 to 3 years after the initial transfer. Also, this transfer retains the possibility of physeal injury at the proximal tibia, a feared complication that has restrained the use of transphyseal ACL substitutions, except in adolescents nearing skeletal maturity. Three knees in two children younger than 5 years have undergone this reconstruction simultaneously with the index open reduction procedure, with one physeal arrest (Fig. 85-16). This complication occurred in the first of bilateral reconstructions in a boy with Larsen syndrome, operated at age 18 months. He underwent the identical procedure on the second knee at age 3, with no physeal injury apparent at 9-year followup. The first side eventually developed a varus-flexion deformity, corrected uneventfully by a simple open wedge proximal tibia osteotomy at age 12. Both knees are painless and stable, with 0- to 120-degree range of motion and normal quadriceps strength. The third knee in the series, in a second child with fibular hemimelia, is stable and painless, and the patient actively runs and plays using a Syme’s amputation prosthesis on the operated side. Although other investigators47 have reported satisfactory stability without physeal injury using this technique in older children (age 12 years), the combined problems of gradual stretching out of the insertion and possibility of physeal injury has led us to use transphyseal hamstring reconstruction more frequently.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree