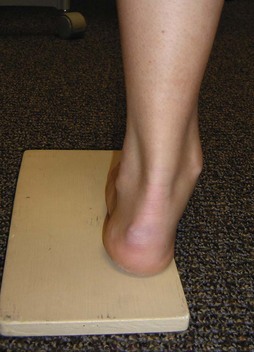
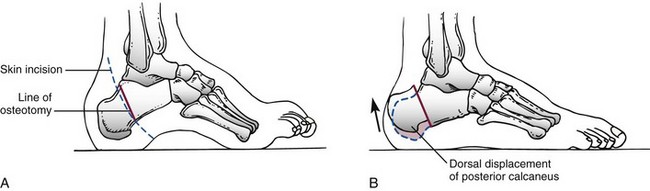
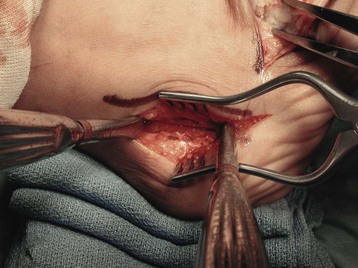
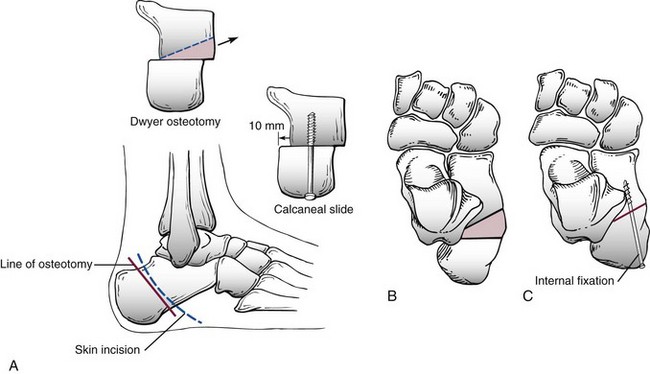
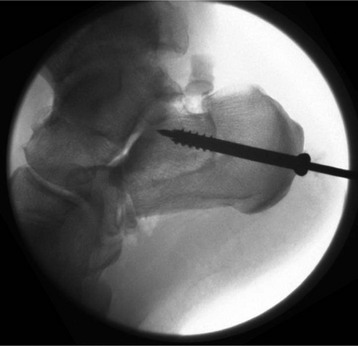
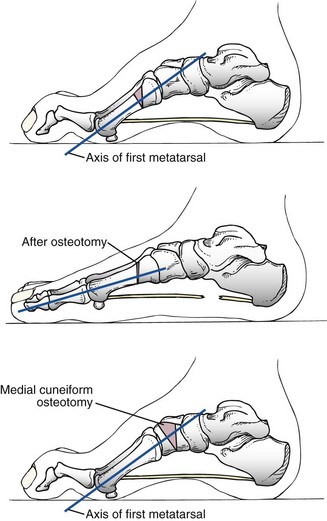
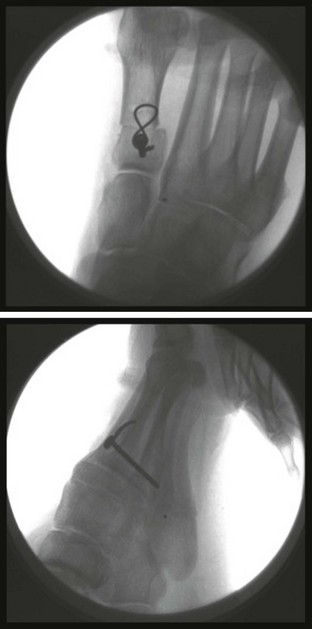
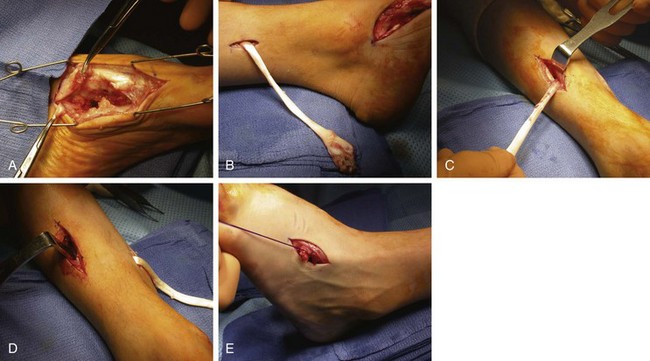
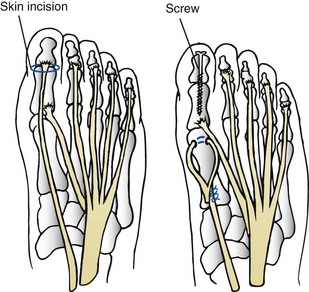
Chapter 34 Charcot-Marie-Tooth disease is a complex group of more than 50 diseases that are inherited, progressive peripheral neuropathies thought to result from an abnormality of myelination. Clinical presentations represent a spectrum of neurologic dysfunction, which reflects what is really a large group of genetically distinct conditions with similar phenotypic presentations. CMT disease as a group is part of a collection of conditions that are referred to as hereditary motor-sensory neuropathies (HMSNs).44 The basic distinction in hereditary polyneuropathies, including CMT, is between motor and sensory components. The hereditary sensory neuropathies (HSNs) have no motor component. Type I HMSN is the classic and most common presentation of CMT disease; up to two thirds of these patients have a cavus foot by adulthood. The most common pattern of inheritance is autosomal dominant, although autosomal recessive forms have also been reported.45 The disease is characterized by slow nerve conduction velocities, and it usually presents during the second decade of life. Genetic research has shown that the disease group demonstrates wide genetic heterogeneity, with 29 genes and more than 30 loci involved. Specific genetic sequences have been associated with a subset of type I patients, further defining this spectrum of disorders with future implications, not only diagnostic and prognostic but also potentially therapeutic.23 The majority of type I presentations have been linked to chromosome 17 and are designated CMT-1A.85 The most common abnormality identified on chromosome 17 is a duplication of a part of the PMP22 gene, but other variants have been identified. Type II HMSN has a similar presentation but is less pronounced and usually appears later in life. In type II, the rate of impulse transfer is normal, but the magnitude of the impulse is decreased, as manifested by the loss of sensory- and motor nerve–evoked response amplitudes. Nerve conduction velocities are seldom slowed and, if so, only mildly.6 The most common lower extremity presentation is bilateral pes cavovarus deformities with leg weakness (Fig. 34-1). Because a majority of these are autosomal dominant diseases, they occur as a familial disorder. Despite this, the variability within families can be so great that individual family members can become symptomatic earlier or later and show significant disparity in the amount of disability secondary to the disorder. In addition to the common presentation of the bilateral pes cavus, the orthopaedist must be aware of progressive weakness in the upper extremities, which usually occurs later than the foot findings. In general, CMT disease affects the longest nerves to the smallest muscles first, hence the symptomatic presentation of feet before hands. Hip dysplasia and scoliosis also are significant presentations in this diagnosis.33 Patients have a variety of complaints, including metatarsalgia, claw toes, tarsal prominence, and recurrent ankle sprains.2,60 The cavovarus presentation is the result of motor imbalance between pairs of muscles around the foot and ankle121 (Fig. 34-2). A common early finding is significant weakness of the tibialis anterior and peroneus brevis muscles.90,151 As a result of tibialis anterior weakness, the first ray is plantar flexed by the stronger peroneus longus, creating a relative forefoot valgus. Compensation for this on weight bearing, considering the foot as a tripod, is a compensatory hindfoot varus. This hindfoot varus is further exaggerated by the unopposed pull of the posterior tibialis muscle against the weakened peroneus brevis. Factoring in intrinsic wasting that causes an intrinsic minus deformity at the metatarsophalangeal (MTP) and interphalangeal (IP) joints, the clinician sees the clinical presentation of hindfoot varus, to midfoot cavus and forefoot valgus, to clawing of the toes. Attempts by the extensor hallucis longus and digitorum longus muscles to dorsiflex the foot further exacerbate toe clawing.60,90 As with all other neuromuscular conditions leading to some level of diminished sensation of the foot and ankle, education is a primary concern. Patients must be taught to examine their feet carefully once they have significantly diminished sensation and must consistently protect their feet with appropriate footwear (Fig. 34-3). Severe deformities and fusions are potentially problematic in the sensory-impaired foot and ankle.94 A thorough neurologic evaluation of these patients is essential, starting with a careful motor examination. Weakness of the anterior tibialis and peroneus brevis muscles is commonly observed, but each muscle of the leg must be assessed as the relative strengths determine the options for management. The original descriptions of CMT emphasized the asymmetry that is commonly observed clinically. The sensory impairment appears later and is usually not as severe. Up to 25% of patients do have significant sensory impairment.140 Vibration, two-point discrimination, and proprioception are the first factors to be affected. In the patient with a cavovarus foot, standing examination clearly shows the relative hindfoot varus, atrophy of the medial longitudinal arch, tarsal bossing, and some degree of toe clawing. In addition, the patient’s legs show significant atrophy below the knee (Fig. 34-4). On the seated biomechanical examination, reduction of the foot into a neutral subtalar position allows the examiner to observe a relatively flexible hindfoot, indicating that the hindfoot varus is compensatory for a fixed forefoot valgus. The primary deformity of the forefoot is a plantar-flexed first ray, but over time, the second and third rays may be similarly depressed in relation to the foot’s lateral border. In the long-standing deformity, because of the relative parallelism between the long axis of the talus and the calcaneus (the varus position of the hindfoot is a result of the medial rotation of the calcaneus beneath the talus), limited dorsiflexion is present because of an abutment of the talar neck against the anterior tibia (Fig. 34-5). The examiner must be sure to evaluate the motion of the talonavicular joint to determine if there is a mechanical block to abduction or a palpable prominence on the lateral aspect of the talar neck that precludes reduction of the midfoot to the hindfoot. When the patient is asked to ambulate, a combination of dorsiflexion weakness, fixed equinus, and difficulties with proprioception give a characteristic steppage gait. The Coleman block test remains the fundamental tool of clinical assessment of the patient with a cavus foot deformity. This classic test described by Coleman and Chestnut28 is useful in examining these patients clinically (Fig. 34-6). The block test is performed by supporting the heel and the foot’s lateral border with a block but allowing the first ray to drop over the edge of the block, and the relative flexibility of the hindfoot is then evaluated. If the hindfoot corrects to neutral or slight valgus, the implication is a compensatory (i.e., “forefoot driven”) hindfoot varus, and that dorsiflexion of the plantar-flexed first ray will correct the hindfoot deformity. If the heel moves only slightly or fails to move at all, the hindfoot deformity is fixed and must be addressed directly, which usually demands a calcaneal osteotomy or hindfoot fusion procedure. This relative hindfoot rigidity, however, is not necessarily the end stage of an algorithm requiring triple arthrodesis. Treatment begins with an accurate diagnosis, and in early stages, this might only require observation. Physical therapy has a limited role, but occasionally, in a young child with early loss of motion, range can be improved with aggressive therapy. Objective support for physical therapy has been reported in patients with CMT.122 Orthotic management and shoe modification do have a role in the treatment of CMT disease and the cavovarus foot. In the foot with significant early involvement, an orthotic device may be used to hold the foot in a more normal position by allowing for plantar flexion of the first ray, with relative posting of the lateral forefoot. An additional lateral heel wedge can also be effective. Ankle–foot orthoses can be used to support the more involved leg and foot deformity, and many adult patients tolerate this for years. However, it is important to note that this may be only a temporary measure because the neuropathy and corresponding deformity will likely continue to progress. Radiographic assessment is important in preoperative planning (Fig. 34-7). A series of weight-bearing radiographs should be taken of both feet and ankles. Because of the severity of many of these deformities, particularly midfoot adductus, obtaining a good lateral view of the foot can be difficult. To obtain a true talar lateral view and a good assessment of the hindfoot, the axis of the medial and lateral malleoli should be parallel to the x-ray beam. This, however, makes the midfoot and forefoot difficult to assess, so a second lateral view may be necessary to for a true lateral view of the forefoot. Studies of the ankle are important, particularly in long-standing severe varus hindfoot, in which case, the lateral ligamentous structures may be compromised. Finally, because this is a sensory neuropathy, radiographic images are useful in the evaluation of possible Charcot neuroarthropathy changes in the foot and ankle. Considerations for surgical treatment in these patients can be complex.5,24,27,58,66,83,143 The patient’s goals, expectations, and demands are the primary concern. Young persons who wear high-top athletic shoes that provide some ankle support and have a large toe box that accommodates clawing of the toes might not require much more than this. In the patient who is considered a surgical candidate, the following three questions are important: n. What is the motor status of each muscle around the foot and ankle? n. Are the deformities fixed or flexible in terms of joint motion? Complete plantar fascia release of the cavus foot is seldom performed in isolation but is commonly performed as an initial step during soft tissue and bone reconstruction in patients with CMT.51,70,119,142 In the earliest presentation of mild flexible cavus, the plantar fascia should not be released. The question arises: Can early soft tissue procedures (complete plantar fascia release) combined with tendon transfers (transfer of the peroneus longus to the lateral portion of the foot) alter the pathologic modeling of the immature foot? Are bony abnormalities observed in patients with CMT genetically driven or only the result of neuromotor imbalance? 1. The plantar fascia is approached through a medial skin incision approximately 3 cm long at the junction between the plantar and medial skin, beginning at approximately the level of the medial tuberosity and extending distally. 2. Sharp dissection is done down to the abductor hallucis muscle. The plantar fascia is easily palpable by using a blunt Mayo scissor, and the tissue above and below the fascia is dissected off the fascia. In long-standing disease, the abductor muscle may show signs of significant atrophy and fibrosis. 3. Once the muscle is retracted, the thickened lateral fascia of the abductor halluces is encountered, which blends plantarly into the plantar fascia and intrinsic musculature. The leading edge of this fascia is found cephalad and carefully transected. A Freer elevator is placed behind this to protect the lateral plantar nerve, which is often visible during this approach. Care must be taken throughout this procedure to avoid manipulation of the nerve. 4. When the abductor fascia is out of the way, the lateral plantar nerve can be seen crossing over to the lateral portion of the foot with a somewhat distal trajectory. The intrinsic musculature and plantar fascia should be clearly visualized and then can be sharply divided. 5. Because this is seldom done as an isolated procedure and is often combined with a calcaneal osteotomy, it is important to ensure that the plantar fascia is completely released so that the tuberosity can easily be mobilized during deformity correction. This procedure is performed to correct hindfoot varus alignment. If the Coleman block test shows some degree of correction but does not allow the hindfoot to correct to slight valgus, or if physical examination reveals well-preserved subtalar motion, a lateralizing calcaneal osteotomy is indicated51,123,124 (Fig. 34-8). Ankle instability may also be present in patients with long-standing deformities and can be confused with subtalar motion. Preoperative standing radiographs of the ankle are important in addition to a careful examination. 1. A curvilinear incision is made beginning 1 cm above the palpable calcaneal tuberosity between the Achilles tendon and the peroneal tendons. This curves down and ends at the junction between the lateral skin and plantar skin at the level of the peroneal sulcus. 2. Sharp dissection is performed straight down to bone because the skin incision is away from the major trunk of the sural nerve and the peroneal tendons. 3. A curved retractor is placed over the top of the tuberosity and another under the calcaneus. An oblique osteotomy is performed perpendicular to the lateral face of the calcaneus from the midportion of the tuberosity to approximately 1 cm past the weight-bearing portion of the calcaneus plantarly (Fig. 34-9). 4. The primary displacement of the tuberosity fragment is laterally into a valgus position. The midaxis of the tibia should fall just to the medial side of the midpoint of the calcaneal tuberosity. 5. The calcaneus may be shifted slightly cephalad (i.e., more vertical) to diminish the calcaneal pitch. Care must be taken not to shift this too far, or impingement of the neck of the talus into the anterior lip of the tibia will result. 6. By changing the obliquity of the osteotomy from more vertical to horizontal, more or less length can be obtained from the calcaneus as necessary, as opposed to more correction of the calcaneal pitch with the more vertical cut. 7. At times, the varus deformity is severe enough that it is necessary to remove a secondary wedge (Dwyer osteotomy)43 (Fig. 34-10). This wedge is generally 1 cm wide laterally, tapering to emerge at the medial cortex, coincident with the first cut. The wedge is usually taken off the distal fragment of the calcaneus. 8. Fixation is accomplished with one or two screws inserted just off the heel pad posteriorly. Attempts should be made to keep the shaft–screw interface as far from the osteotomy as possible because this is the most common site of hardware failure. Both lateral and axial fluoroscopic image can be useful to confirm screw position. 9. In cases where a more significant deformity is addressed, a multiplanar osteotomy (“Malerba” type) may be used. This Z-shaped osteotomy has the potential advantage of allowing for translation, angulation, and rotation (Fig. 34-11). When the hindfoot corrects completely to slight valgus with the Coleman block test and the medial ray is fixed in plantar flexion, a medial column dorsiflexion osteotomy is indicated24,27,155 (Fig. 34-12). Careful examination of the forefoot will reveal whether this deformity is limited to a plantar-flexed first ray, or if the second and sometimes the third rays are also involved. When only the first metatarsal is plantar flexed, a dorsal closing-wedge osteotomy of the medial cuneiform can be performed. In general, the osteotomy should be located at the apex of the midfoot as seen on the standing lateral radiograph. In some presentations, a dorsal closing-wedge osteotomy across the midfoot (navicular/cuneiforms/cuboid) is necessary. If there is an adductus component, this can require a biplanar osteotomy (dorsal–lateral). It should be noted that the reliability of achieving bony compression is greatest for the first metatarsal osteotomy, so one must consider whether the quality of the bone to be compressed will allow adequate fixation if a cuneiform or other osteotomy is contemplated. 1. The proximal first metatarsal is isolated through a medial incision. In the skeletally immature foot, the proximal location of the first metatarsal growth plate must be identified and protected. The anterior tibial tendon must also be protected. 2. A dorsal closing-wedge osteotomy is most useful. Care is taken to maintain the plantar cortex. The first ray is dorsiflexed, and the overall alignment is assessed. 3. Fixation is generally with a smooth pin in the skeletally immature patient and with a distal-to-proximal screw or dorsal-medial plate in the skeletally mature patient. 4. An alternative method for stabilization is to approach the base of the first metatarsal dorsally and perform a closing-wedge osteotomy from the top. This can be stabilized with a tension band wire placed around a post created with a 2.4-mm screw adjacent to the metatarsocuneiform articulation. A 22-gauge wire is sufficient (Fig. 34-13). 5. Careful assessment is then made of the second and third metatarsals. If further deformity correction is required, an incision is made between the proximal half of the second and third metatarsals. The proximal portion of the second metatarsal is exposed subperiosteally, and a long oblique osteotomy is performed. Then the distal portion of the second metatarsal is allowed to float into its corrected position. A small amount of cancellous bone graft obtained from the calcaneus can be used to enhance bone healing around the first and second metatarsal osteotomies. 6. The dorsal closing-wedge osteotomy of the medial cuneiform is performed through a slightly more proximal incision. The tibialis anterior will be crossing over a portion of the cuneiform and must be protected. The first osteotomy is parallel to the distal articular surface of the cuneiform at about the distal two thirds. Make the second cut, creating and removing the appropriate-size wedge. Dorsiflex the first ray and use internal fixation. Remember that the medial cuneiform is wedge shaped and narrower at the base. In general, the peroneus longus tendon maintains its strength well into the disease process. It is a primary deforming force and therefore an excellent choice for tendon transfer, which removes a deforming force while providing a useful and functional motor for transfer.2,60,7 Specifically, the goal is to oppose adduction by the posterior tibialis tendon and/or to aid in dorsiflexion of the foot.139 The latter is accomplished by tendon transfer around the fibula into the cuboid and the former by tenodesis to the peroneus brevis tendon. 1. The incision for the calcaneal slide osteotomy is extended to the base of the fifth metatarsal, staying dorsal to the plantar skin. 2. The abductor digiti quinti muscle is encountered first and retracted. The peroneus brevis tendon is identified and retracted, and the peroneus longus tendon is found deep to it against the groove in the cuboid. 3. The peroneus longus tendon is brought into the wound’s more superficial aspect with a right-angled instrument, the transection site is selected, and a suture is placed just distal to this and tied into the insertion of the peroneus brevis. 4. An incision is made approximately 10 cm proximal to the tip of the lateral malleolus just behind the fibula, with sharp dissection down through the skin and subcutaneous tissues. The peroneal sheath is opened. A slight tug on the peroneus longus distally identifies the tendon proximally. The tendon is then brought into the proximal wound. 5. An incision is made over the cuboid in line with the fourth metatarsal, and the peroneus longus tendon is transferred subcutaneously to this level. 6. The transferred tendon is secured using soft tissue anchors and heavy absorbable suture. 7. An alternative peroneus longus transfer is to the peroneus brevis tendon. Tenodesis can be accomplished over the last 3 to 4 cm of the peroneus brevis before its insertion into the fifth metatarsal. If a fixed adductus deformity exists, however, a medial release or midfoot osteotomies must be considered. After the triceps surae musculature, which almost always maintains some strength, the posterior tibial tendon is the second strongest motor around the foot and ankle. Therefore it is usually a late deforming force and a motor with enough residual power to be considered for transfer. The posterior tibial tendon is transferred through the interosseous membrane (Fig. 34-14) in patients with a foot that is essentially paralyzed except for the posterior tibial tendon tendon and the triceps surae. A lengthening of the triceps surae may be necessary if an equinus contracture is present, but in the absence of equinus or if a calcaneocavus deformity is present, lengthening is typically not necessary. When dealing with the posterior tibial tendon as a deforming force in the presence of significant midfoot adductus, the flexible deformity may be corrected with a medial release and transfer of the peroneus longus to the peroneus brevis tendon. In the fixed deformity, correction of the metatarsus adductus may require midfoot osteotomies (Fig. 34-15). 1. A short medial incision is made over the talonavicular joint. The posterior tibial tendon is identified and sharply excised from the navicular and cuneiform, obtaining as much length as possible. 2. Another short incision is made approximately 10 cm above the medial malleolus just behind the tibia. The posterior tibial tendon is readily identified proximally and then brought into this wound. The flexor digitalis longus (FDL) tendon is typically the first tendon visualized through this incision. 3. At the same level, approximately 10 to 12 cm above the ankle, a straight anterior incision is made just lateral to the crest of the tibia. The anterior compartment along with the neurovascular bundle is then retracted laterally. The interosseous membrane is then identified between the fibula and tibia. 4. A window approximately 3 cm wide is made in the interosseous membrane. An instrument is then passed through the interosseous membrane, remaining on the tibial cortex, transferring the posterior tibial tendon deep to all other structures and through the window. 5. The tendon is then passed subcutaneously or subretinacularly down to the level of the cuboid and anchored using a soft tissue anchor and absorbable suture. Alternatively, the tendon can be fixed with a tenodesis screw if there is sufficient length. The tendon may be also sutured to the peroneus tertius. Correction of clawing of the great toe with transfer of the extensor hallucis longus (EHL) tendon is often indicated for the symptomatic deformity. This also improves the role of the EHL as an ankle dorsiflexor.151,70 1. A midline incision is made over the dorsum, exposing the MTP and IP joints of the hallux. With the EHL tendon protected, cartilage is removed at the IP joint and fixed with a single screw from distal to proximal (Fig 34-16). 2. The EHL tendon is then transected, leaving enough tendon to allow tenodesis of the MTP joint in a neutral position. 3. The EHL tendon is then tenodesed into the distal portion of the first metatarsal through a drill hole, with the foot held in a neutral position at the ankle to apply appropriate tension (see the technique for the Jones procedure in Chapter 26). If the extensor digitorum communis tendon is a deforming force acting to dorsiflex the foot, it could be tenodesed to the dorsum of the foot, again making sure that appropriate tension is achieved.24,103 If the toe deformities are flexible, a Girdlestone-Taylor148 transfer may be performed. If significant clawing is present, an MTP capsulotomy transecting the collateral ligaments will be necessary to achieve realignment. If the deformities are fixed, a Girdlestone-Taylor procedure may still be done, but resection of the proximal interphalangeal joint (PIP) may be indicated (see the technique for the Girdlestone-Taylor tendon transfer in Chapter 7). For any procedure used to correct a progressive neuromuscular condition, the outcome is difficult to evaluate. Evaluation of triple arthrodesis, which for years has been a hallmark procedure in the treatment of the severe cavovarus foot deformity in this diagnosis, would indicate mixed results at best.94,88,159 Triple arthrodesis should be used only as a salvage procedure for a rigid deformity that shows signs of degenerative joint disease of the hindfoot. It is particularly important to ensure that concomitant ankle instability is addressed with ligamentous reconstruction, with or without anterior ankle debridement, and that the hindfoot is positioned in a neutral position if a triple arthrodesis is deemed necessary. The triple arthrodesis can be an excellent salvage procedure. The concept of removing wedges to perform this arthrodesis is rarely beneficial.136,137,154,165 The key to successful correction of the deformity is derotation of the calcaneus under the talus, allowing the talus to plantar flex and the hindfoot varus to move into slight valgus. A variety of midfoot osteotomies have been described, the rationale being that the midfoot is the apex of the deformity. The Japas procedure67 is essentially a vertical chevron osteotomy through the midtarsal region. The Jahss procedure65 is a truncated wedge osteotomy through the midtarsal region at the apex of the deformity; however, the foot must have appropriate muscular balance. Ankle instability must be documented and some form of treatment instituted. When the cavovarus foot is reconstructed, a lateral ligamentous reconstruction can be performed as well. This can be done with local tissues or autologous tendon (see the discussion of ankle reconstruction in Chapter 30). Treatment of this disorder involves a range of deformities, from congenital presentations to modeling changes in the growing foot and conditions in the skeletally mature patient. Up to one half of children with myelomeningocele have some type of significant foot deformity.40 The most common congenital foot deformity is talipes equinovarus (clubfoot) deformity.130 Vertical talus is also noted with this diagnosis. Other deformities include calcaneus and equinus of the hindfoot with components of valgus or varus. The primary goal in treatment of these foot deformities is a relatively supple plantigrade foot. Because of the highly variable paralytic and sensory deficit and variable functional capacity, treatment of these patients must be determined carefully. It is just as important for the nonambulatory patient to have a plantigrade, shoeable foot that fits on the footrest of a wheelchair as it is for a low lumbar patient with good quadriceps function to have a plantigrade and braceable foot and ankle. Although the early emphasis in these children is on functional motor level (i.e., whether they will ultimately ambulate), an important long-term prognostic factor is foot sensibility. The majority of these children have an insensate foot and loss of proprioception; only patients with the lowest lumbar and sacral levels have any preservation of plantar skin sensation. Early patient and parent education focuses on careful inspection of feet, socks, and footwear. All children with this diagnosis should wear some type of orthosis as a protective measure for the insensate foot and a preventive measure against the deforming forces that can lead to fixed contractures and deformities.163 These children must never be barefoot and, even when swimming, must wear some appropriate form of protective footwear. Discussions of foot sensory deficits with patients and their parents must also include the need for preservation of a plantigrade foot. Deformity that limits the weight-bearing contact surface of the foot’s plantar aspect increases focal pressures and can result in ulcerations.55 The correction of deformity alone is not enough; deforming forces around the foot and ankle must be balanced as well. Arthrodesis to correct deformities of the foot and ankle in these patients should be avoided.18 Rigidity of the foot and ankle reduces the foot’s ability to accommodate to irregularities of the ground. This can result in increased pressure on the foot’s plantar surface and on the joints adjacent to the sites of fusion.91 This increased pressure through the remaining articulations of the foot and ankle can result in the Charcot neuropathic arthropathy.56 Although triple arthrodesis is an excellent procedure for the correction of severe deformities of the foot, it is not appropriate in patients with sensory compromise. In these patients, tendon transfers and extraarticular osteotomies can be used to reduce pressure on the calcaneus.107 However, in the older or nonambulatory patient who has trouble fitting shoes or braces, triple arthrodesis is a good compromise to obtain a plantigrade foot. Even then, a limited fusion is preferable.17 Use of casting in these patients should be reserved for healing of ulcerations and for the protection of soft tissues after surgical reconstructive procedures. Serial casting of deformities can be problematic because of the insensate nature of the foot. The casting of the congenital deformities in these patients must be carefully considered.153 The majority of these feet will eventually need surgical correction. If no correction is found after short-term casting, the clinician should consider the use of holding splints until the child’s foot is mature enough to undergo surgery. Postoperative casting must be lightweight, be carefully padded, and have room for swelling. The cast should be used only to support the soft tissues and not to achieve foot correction. The clubfoot deformity (Fig. 34-17) is generally seen in myelomeningocele of the third lumbar level or above.130,34 At this level, the foot is essentially completely paralyzed and insensate, with occasionally some anterior tibial function. In the infant, it is very difficult to assess any voluntary or involuntary motor function around the foot and ankle. Repeat examinations are helpful, as is family input, but often family members mistake hip flexion for foot motion. The difficulty with motor function assessment is evident in the patient whose unrecognized posterior tibial function results in progressive clubfoot deformity. Because of the insensate nature of these feet and their relative stiffness on presentation, cast treatment should be used carefully.153,96 The majority of these feet do ultimately require surgery; however, casting should attempted initially. The foot should first be manipulated and then a holding cast applied. The cast itself should not be used to get further correction after it has been applied (Fig. 34-18). If casting is successful, splints must be worn full time until the child is standing. The authors’ preference is to stop casting at 3 months if the foot is not corrected, and perform surgery at approximately 9 months. Surgery at this age usually allows the patient to be up and standing or walking at approximately 1 year of age. This helps maintain the patient’s development and the plantigrade nature of the correction. The clubfoot deformity in myelomeningocele cannot be corrected by limited surgery (Fig. 34-19). The use of the complete subtalar release is necessary.93 Only in sacral-level deformities should tendon lengthening be performed. At all other levels, the tendons should be resected; if not, scarring of the lengthened tendons will result in recurrence of the deformities. It is easier in the long term to brace a flaccid foot. The main concern at surgery and in the immediate postoperative period is the soft tissue envelope and the potential for significant loss of skin (see the discussion of surgery for clubfoot in Chapter 33). In late childhood and adolescence, with a fixed bony deformity, osteotomies should be considered before a triple arthrodesis or a talectomy.161 Although a talectomy will correct the deformity, the position is difficult to maintain with orthotics, and plantar pressure will not be evenly distributed.38,97,128,133,134 Careful evaluation of bony deformity and any residual motors that may be causing recurrent deformation must be factored into the surgical plan. This, combined with the patient’s functional needs, provides some rationale as to how aggressive the surgeon must be to obtain a completely plantigrade or a near-plantigrade foot.96 1. The most common surgical incision is the Cincinnati incision.31 This approach provides excellent visualization from the medial midfoot around the posterior aspect of the hindfoot to the lateral midfoot. The primary difficulty with this incision in the foot with a severe equinus deformity is sloughing of the posterior skin. After correction of the foot deformity and closure of the skin, careful assessment of skin tension should be evaluated. By leaving the foot in a plantigrade position and performing slow, gentle serial casting after postoperative swelling has subsided, this risk of skin slough may be avoided. 2. When too much tension still exists, to obtain posterior skin closure, a vertical posterolateral incision can be made. After mobilizing the posteromedial skin and rotating it to achieve coverage, the posterolateral skin is mobilized and rotated, leaving a skin defect over the extensor brevis muscle dorsolaterally, which can be covered with a split-thickness skin graft. 3. The two-incision surgical approach of Carroll,21 which combines a vertical posterolateral incision and an S-shaped medial incision, is an excellent alternative. This provides good exposure and has been effective with even the most severe deformities. 4. Beginning posteriorly after sectioning of the Achilles tendon, the posterior tibiotalar and subtalar capsules are opened. The posterior tibialis, flexor digitorum longus, and flexor hallucis longus tendons can all be sectioned proximally, as can the peroneus longus and brevis tendons on the lateral side. Care should be taken laterally that a complete sectioning of the subtalar capsule, as well as of the posterior talofibular ligament and calcaneal fibular ligament, is performed. When the foot is in severe equinus, it is often necessary to open the syndesmosis from a posterior approach for the talus to dorsiflex into the ankle mortise. 5. A complete medial release should be performed, including resectioning the medial tendons, particularly the posterior tibial tendon, and opening the master knot of Henry. 6. The plantar fascia and the short intrinsic musculature are transected. 7. Complete capsulotomy of the midfoot articulations and the anterior portion of the subtalar joint must be performed. 8. The surgical procedure is accomplished when the hindfoot can be derotated into a more anatomic position. This usually requires complete release of the subtalar joint and the interosseus ligament. In this case, after the talus has been medially rotated and pinned to the navicular, a vertical pin stabilizing the subtalar joint may be necessary to avoid subluxation of the calcaneus into valgus. If the calcaneocuboid joint has been completely opened, a pin inserted laterally to stabilize this articulation may be necessary. 9. Pins are brought out the dorsum of the foot and are carefully bent, clipped, and padded. 10. Skin is closed carefully but not too tightly. 11. The foot is then assessed for position and placed in a short-leg cast in the position where the foot lies passively.
Congenital and Acquired Neurologic Disorders
General Considerations
Congenital Neurologic Disorders
Charcot-Marie-Tooth Disease
Treatment Approach
Surgical Treatment
Plantar Fascia Release
Surgical Technique (Video Clip 47
![]() )
)
Lateralizing Calcaneal Tuberosity Osteotomy
Surgical Technique
Metatarsal Osteotomy (Video Clip 118
![]() )
)
Surgical Technique
Peroneus Longus Tendon Transfer
Surgical Technique (Video Clip 49
![]() )
)
Posterior Tibial Tendon Transfer
Surgical Technique
Modified Jones Procedure
Surgical Technique (Video Clip 57
![]() )
)
Correction of Lesser Toes
Salvage Procedures
Myelomeningocele
Sensory Deficits
Treatment Approach
Cast Treatment
Talipes Equinovarus
Conservative Treatment
Surgical Treatment (Video Clip 91
![]() )
)
Correction of Clubfoot
Surgical Technique
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree