Chapter 9 Complications of Supracondylar Fractures and Their Management
Background/aetiology
The incidence of vascular injuries following supracondylar fractures varies between 5% and 35%.1,2 In addition, patients may also suffer from vascular compromise, which can range from an absent or weak pulse to a frankly ischaemic limb.
Peripheral nerve injuries occur in 5–15% of supracondylar fractures.3,4 All nerves crossing the elbow may be injured, with the commonest being the median and its anterior interosseous branch. The median nerve is most at risk with posterolaterally displaced fractures, while the radial nerve is more likely to be damaged if displacement is posteromedial. The greater the bony displacement, the greater is the risk of nerve injury. Although most nerves are damaged at the time of the fracture, it is important to appreciate that they are also at risk during surgical treatment. In particular, the ulnar nerve may inadvertently be injured during pin insertion for fracture fixation.
Presentation, investigation and treatment options
Vascular injuries
If the hand is obviously ischaemic, the arm should be immediately manipulated and splinted in an extended position. This will often restore the circulation to the hand but if this fails the child should be taken immediately to the operating room for closed reduction and pinning. The role of arteriography is controversial.5,6 While plainly any information about the vascular status is helpful, undertaking the technique should not lead to undue delay with treatment. The rationale is that this is an emergency situation and, if the circulation does not return following reduction and pinning of the fracture, exposure of the brachial vessels should be performed. If the artery is trapped between bony fragments then the fixation should be taken down and the artery liberated. If the artery is crushed, transacted or has an intimal tear, reconstruction will be required, usually with help from a vascular or micro trained surgeon. In this situation it is also important to perform a fasciotomy of the deep fascia of the forearm, particularly if there has been significant ischaemia time.
Malunion
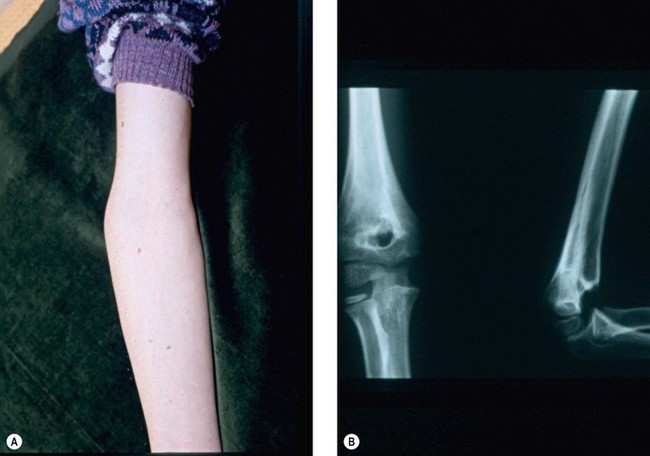
Cubitus varus or valgus is assessed by measuring the carrying angle of the arm. This is the angle created by the medial border of the fully supinated forearm and the medial border of the humerus when the elbow is extended (Fig. 9.1). The angle typically varies between the sexes, with the normal range lying between 6° and 12°. It is generally greater in female than male patients and is best assessed by comparison with the contralateral side. In addition, as the normal elbow extends, the carrying angle increases, i.e. becomes more valgus. With malunions, however, hyperextension tends to accentuate a cubitus varus deformity, while a flexion contracture can create the appearance of cubitus valgus. Measurement of rotational deformity is more difficult but can be assessed by asking the child to bend forward such that the thoracolumbar spine is parallel to the ground. Each arm is then placed in turn behind the patient’s back and rotation measured as the angle between the forearm and the patient’s thoracolumbar spine when the arm is maximally rotated.
Gurkan et al7 described posterior instability of the shoulder in three patients with cubitus varus deformity.
A less commonly reported complication of supracondylar fractures of the humerus in children is the dissolution of a portion of the trochlea at a variable time after fracture (Fig. 9.2). If this defect to the trochlea is severe it will allow migration of the ulnar proximally.8 A similar complication on the lateral side of the elbow was reported by Vocke-Hell et al.9 They noted that this could occur at any time between 1 and 4 years after the fracture and may result in secondary radial head dislocation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree