CHAPTER 61 Complications of Elbow Replacement Arthroplasty
INTRODUCTION
The majority of these complications neither require surgery nor adversely influence the ultimate result. Thus, these problems might best be discussed according to their management and significance: (1) those that increase the morbidity but do not influence the outcome by requiring additional surgery, removal, or replacement of the implant; and (2) those requiring additional surgery, including revision of the implant. Gschwend and colleagues,21 in their systematic review of the world’s literature from 1986 to 1992, discussed 828 procedures. Of these, 43% had complications (Table 61-1).
TABLE 61-1 Complications of Elbow Replacement, 1986-1992
| Complication | Incidence (%)* |
|---|---|
| Aseptic loosening | |
| Radiologic | 17.2 |
| Clinical | 6.4 |
| Infections | 8.1 |
| Ulnar nerve lesions | 10.4 |
| Instability | 7-19 |
| Disassembly | — |
| Dislocation | 4.3 |
| Subluxation | 2.2–6.5 |
| Intraoperative fractures | 3.2 |
| Fractures of prosthesis | 0.6 |
| Ectopic bone formation | — |
* Total number of cases = 828.
In the intervening years, there have been many advances in prosthetic design and surgical technique. For example, constrained devices have been eliminated owing to their high rate of loosening. Semiconstrained and unconstrained devices are being used now, and recently, hybrid designs that are unlinked but can be converted to a linked design have been developed. Variations in techniques such as triceps tendon dissection and repair, better cementation techniques, routine antibiotic prophylaxis, and others have emerged. Despite advances in prosthetic design and surgical technique over the past decade, there had been no systematic review of the literature on the complications of TEA since the 1996 report by Gschwend et al.21 We recently conducted a comprehensive review of the literature to determine the complications associated with modern-day TEA.56 The review comprised 38 studies that reported on 1981 total elbow replacements. The overall significant complication rate (requiring another surgical procedure or resulting in permanent clinical sequalae) after primary TEA was 27.9% ± 13.3%. The main complications included 4.8% clinical loosening (including symptomatic loosening or revision), 3.8% instability including dislocation and symptomatic subluxation, 2.5% deep infection, and 2.5% ulnar nerve complications56 (Table 61-2). In this edition, the treatment of infection is discussed in detail in Chapter 62, and loosening and periprosthetic fractures are dealt with in the chapters on revision (see Chapters 65 and 66). A detailed summary of the current literature regarding complications is given in Table 61-2.
TABLE 61-2 Complications of Elbow Replacement, 1993-200456
| Complication | Incidence (%) |
|---|---|
| Aseptic loosening (clinical) | 4.81 |
| Aseptic loosening (clinical and radiographic) | |
| Linked Designs | 15.92 |
| Unlinked Designs | 18.53 |
| Infections | 2.51 |
| Ulnar nerve lesions | 2.51 |
| Disassembly | 4.21 |
| Dislocation/Subluxation | 3.81 |
| Intraoperative fractures | 1.81 |
| Fractures of prosthesis | 1.11 |
| Ectopic bone formation | — |
1 Total number of cases = 1981.
2 Total number of cases = 282.
COMPLICATIONS NOT USUALLY REQUIRING SURGERY
MOTION RESTRICTION
The goal of elbow replacement surgery is to obtain the functional arc of 30 to 130 degrees of flexion.39 Those rheumatoid arthritic patients who have the ankylosing type of disease tend not to obtain the typical 30 to 130 degrees of flexion-extension after surgery.7 Therefore, we attempt to treat this motion restriction with an aggressive capsular resection at the time of the implantation. If the anterior capsule is contracted, sufficient depth of insertion is most important. A trial reduction is essential to identify this potential problem so that it can be avoided. Often, a static adjustable splint is used to gain or maintain motion. Furthermore, a slight but consistently greater flexion contracture is observed with resurfacing designs (see Chapter 52).
WOUNDS
Wounds are much less a problem today19 than the 5% incidence previously reported.9,13,23,34,46
Management
Wound healing problems are best avoided. At the Mayo Clinic, we avoid the use of the steri-drape after skin preparation with iodinated solutions, especially in patients with rheumatoid arthritis. I also use a straight incision just medial to the tip of the olecranon and carefully cauterize vessels during surgery. The elbow is placed in full extension with a compression/cryotherapy (Cryocuff Aircast, DJO, Vista, CA) device, which is now used routinely.1 If the wound remains tenuous at 1 week or 10 days, we do not hesitate to place the patient in a cast or anterior splint for 10 to 14 days and then reassess.33 If severe wound necrosis occurs, surgical treatment may involve special soft tissue coverage, which is discussed in Chapter 36.
NEURITIS
In patients with rheumatoid arthritis or in a joint that has been subjected to previous surgery, the ulnar nerve is particularly vulnerable. The incidence of ulnar nerve involvement has been reported in 2%3 to 26%13,54 of patients and varies in severity from profound neuropathy in less than 5%9,31,49,52 to transient paresthesias in as many as 25%.21 Implicated causes are excessive traction, perineural or epineural hematoma, direct mechanical pressure during the procedure, and irritation by the bandage or from swelling. The possibility of thermal damage from juxtaposed methylmethacrylate may be considered, as well as devitalization during the translocation procedure. Gschwend’s review of the experience in the literature from 1986 to 1992 reveals an incidence of approximately 10% after almost 900 procedures.21 We have found 3% subjective symptoms after 700 procedures at the Mayo Clinic. No patient had motor weakness.
In our review of literature in the last decade, the rate of ulnar neuropathy was found to be 2.5%.56 In light of the association between TEA and ulnar neuropathy, controversy persists regarding the need for routine ulnar nerve transposition during surgery. Some of the cited advantages of routine nerve transposition include protection of the nerve in a safe location during the exposure and elbow manipulation, decreasing the stretching forces on the nerve with elbow motion postoperatively, and reducing the compression on the nerve in the cubital tunnel. Some of the disadvantages include injury to the blood supply to the nerve and mechanical injury during the dissection. In our meta-analysis,56 the rates of significant ulnar neuropathy were compared between the studies that routinely transposed and the ones that selectively transposed the nerve. The results showed that routine ulnar nerve transposition resulted in lower rates of significant ulnar neuropathy (2.1% ± 3.5%) compared with the studies in which the nerve was not mobilized routinely (4.3% ± 5.2%) (P = 0.17). Even though this difference was not statistically significant, it is believed to be clinically significant. The overall rate of significant ulnar neuropathy was only 2.5%, making it very difficult to detect a statistically significant difference between routine and nonroutine ulnar nerve transposition.
TRICEPS INSUFFICIENCY
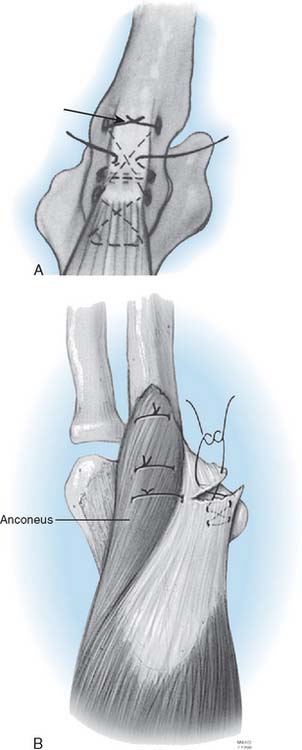
Triceps insufficiency is probably common, but it is not reported very often. The poor quality of the triceps tendon in patients with rheumatoid arthritis is well recognized, but only about 4% of patients with rheumatoid arthritis have been recognized as having significant triceps insufficiency.35,38 The Mayo approach and its modification57 was developed because of this problem.5 We have documented 13 of 700 (2%) since 1981. In our literature review of the last decade,56 triceps-related complications were analyzed after the three most common triceps dissection techniques. No triceps-related complications were found with the V-shaped tongue approach at the musculotendinous junction. Triceps reflection, with or without extra-articular wafers of olecranon, was associated with a complication rate of 2.3% ± 4.6%, whereas the triceps split, either with or without extra-articular wafers of olecranon, was associated with a 6.2% ± 14.8% complication rate. The difference in complication rates between the three approaches was not statistically significant.56
ECTOPIC BONE
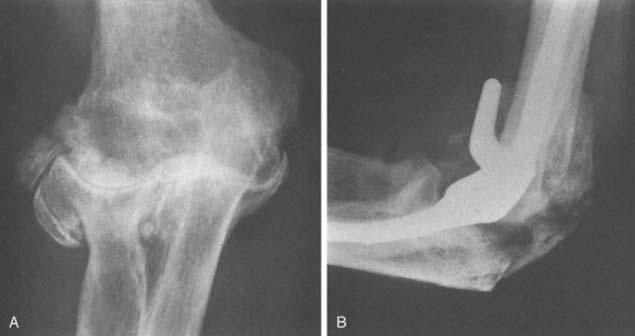
Ectopic bone has been reported after TEA.15 Although some heterotopic ossification may be seen following elbow replacement, in our experience and opinion, this is a very rare complication that occurs only under unusual circumstances, such as in patients with severe degenerative arthritis.26 We have observed only three cases of this problem after approximately 700 primary and revision total elbow replacements using several implant designs and exposures. In one patient, marked hypertrophic changes existed before surgery, extensive bleeding occurred after surgery, and moderate ectopic bone developed (Fig. 61-2).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree