Chapter 48 Complications of Anterior Cruciate Ligament Reconstruction
Rupture of the anterior cruciate ligament (ACL) is one of the most common ligament injuries to the knee. More than 100,000 ACL reconstructions are performed each year in the United States. The goal of these procedures is to re-create a stable and functional knee joint that allows return to the level of activity prior to injury. Current arthroscopic techniques have success rates reported between 75% to 95%. However, as many as 5% to 10% of ACL reconstructions are revisions.20 As with all surgical procedures, there are inherent risks to the reconstruction of the ACL. Complications from ACL reconstruction can be viewed as intraoperative or postoperative. Intraoperative complications include malpositioned tunnels, improper tensioning, and failure of graft fixation. Postoperative failures include infection, arthrofibrosis, graft failure, and osteoarthritis. The choice of graft also precludes an inherent set of complications, whether it is autologous bone-patellar tendon-bone, autologous hamstring, or allograft.
Intraoperative Complications
Tunnel Placement
Intraoperative complications often result from technical errors. Wetzler and colleagues83 have found that 77% of ACL revision cases are the result of technical shortcomings, including nonanatomic tunnel placement, graft impingement, improper tensioning, and inadequate graft fixation. Proper positioning of the femoral and tibial tunnels is essential to successful reconstruction of the ACL. Among these intraoperative complications, improper tunnel placement is the most common, specifically an anteriorly located femoral tunnel,38 which leads to excessive strain during flexion and restricted range of motion. A femoral tunnel that is too vertically oriented (the 12-o’clock position) may control anterior-posterior forces on the knee joint but will lack the rotational control of the native ACL.61 A femoral tunnel located too posteriorly in the notch risks blowing out the posterior wall of the tunnel, which may compromise fixation of the graft. If this occurs, one may move from interference to suspensory fixation, or another option is to redrill the femoral tunnel using an outside-in technique. Jepsen and coworkers36 randomized 60 patients undergoing ACL reconstruction to low or high femoral tunnel positions and found no difference in laxity at 25 and 70 degrees, but a significant increase was found in subjective knee stability in the group with low (2-o’clock) femoral tunnels. While drilling the femoral tunnel, one should attempt to recreate the anatomic attachment of the native ACL, whether it is through a transtibial, anteromedial, or retrodrill technique.1
The tibial tunnel is more forgiving than the femoral tunnel but malpositioning can also lead to complications. The tunnel should be located posterior to Blumensaat’s line when viewed on a lateral x-ray. When the tibial tunnel is drilled too anterior of the native footprint, the graft will impinge and likely fail. When too posterior, the graft becomes too vertical and loses rotational stability in the same fashion as the anteriorly drilled femoral tunnel.49 Medial or lateral malpositioning of the tibial tunnel can lead to impingement, increased laxity, or chronic synovitis.49,55
Some complications regarding tunnel placement are inherent to the technique used for reconstruction. During ACL reconstructions using a double-bundle technique, one must avoid convergence of the two tunnels in the femur and tibia. This can be accomplished by measuring the footprint to ensure appropriate size, careful pin placement, avoiding tunnels over 9 mm in diameter, and potentially drilling tunnels using an outside-in technique. Recently, several systems have been developed to help prevent tunnel convergence. An anteromedial portal may be used to drill the femoral tunnels. Anteromedial drilling allows anatomic placement of the femoral tunnels that is independent of the tibial tunnels. If an anteromedial portal is used, care must be taken to avoid damage to the medial femoral condyle as the guide pin or reamer pass closely by the articular surface. We recommend careful visualization during creation of the anteromedial portal and the use of half-fluted reamers to help avoid cartilage damage (Fig. 48-1). Additionally, an anteromedial drilling technique may lead to shorter femoral tunnels than typically encountered with a transtibial technique. Fixation strategies should be adjusted to ensure an adequate amount of graft within the femoral tunnel to allow graft integration.
Impingement of the graft is often caused by nonanatomic tunnel placement but can also result from oversized grafts and inadequate notchplasty. Impinging ACL grafts will deform with strain and will likely become lax or fail.24 Abrasion of the graft on the lateral femoral condyle or intercondylar roof can cause chronic synovitis, ligament attenuation, and failure.74 However, aggressive notchplasty may damage articular cartilage. A dog model demonstrated histopathologic changes at 6 months similar to those of early degenerative arthritis in groups undergoing aggressive notchplasty.45 Others have noted that although notchplasty may assist in visualization during arthroscopy, there does not appear to be a clinical difference in patients who did or did not receive a notchplasty during their ACL reconstruction.58 Minimizing the notchplasty may reduce postoperative pain, bleeding, swelling, and potential notch regrowth.21,60
Graft Tension
Another complication of ACL reconstructions arises from improper tensioning of the graft. Inadequate tensioning creates a loose graft that will not re-create joint stability and kinematics. Overtensioning of the graft can lead to loss of motion, graft stretching, excessive stress on the articular cartilage, poor vascularity, and subsequent graft degeneration.33,85 Failure to precondition a graft cyclically can decrease forces within the graft by 30% soon after fixation.29 A review of the randomized controlled trials evaluating graft tension in ACL reconstructions using bone-patellar tendon-bone (BPTB) autograft and hamstring autografts found no statistically or clinically relevant differences in various graft tensions.5 The amount of tension that should be applied to optimize outcome is unknown at this time.
Graft Contamination
Graft contamination caused by the graft being dropped onto the floor of the operating room is a rare but dangerous intraoperative complication which can lead to early septic arthritis. Cooper and associates15 investigated the incidence of positive cultures in dropped grafts in an operating room environment. Six of 10 grafts (60%) that were dropped on the floor for 3 minutes had a positive culture at 10 days. Three of 10 grafts (30%) that were dropped on the floor for 3 minutes and then soaked in sterile saline containing bacitracin and polymyxin B for 15 minutes also had positive cultures at 10 days. Similarly, Molina and coworkers54 harvested native ACLs during total knee arthroplasties, dropped them onto the operating room floor for 15 seconds, and then cultured them. In this study, 29 of 50 specimens (58%) were found to have positive cultures. Grafts soaked in solutions exhibited drops in the positive culture rate—12 of 50 (24%) in the povidone-iodine solution group, 3 of 50 (6%) in the antibiotic solution group, and 1 of 50 (2%, in broth only) in the chlorhexidine gluconate group. Although data regarding dropped grafts are limited, a survey of surgeons found that many recommend cleansing the graft and proceeding with the ACL reconstruction rather than harvesting a different autograft or switching to allograft.33 A combination of chlorhexidine gluconate and triple antibiotic solution in sterile saline appears to be the most effective for preventing positive cultures.28 The most effective way to prevent graft contamination caused by a dropped graft is clearly prevention. We recommend minimizing hand-offs during the reconstruction, clear communication between staff when the graft is being moved, and clamping the graft on the field.
Graft Fixation and Maturation
Until a graft has incorporated into the host bone tunnels, it is dependent on adequate fixation strength for stability. Current rehabilitation protocols emphasize early range of motion and strengthening, underscoring the need for stable fixation. One study has found no difference in clinical outcome among interference screws, whether they were metallic, titanium, or bioabsorbable.21 Furthermore, good results have been found with soft tissue grafts when using EndoButton, femoral transfix, soft tissue screws, or a tibial-sided screw and washer. BPTB grafts begin to incorporate between 6 and 12 weeks. At 16 to 24 weeks, a normal bone-ligament junction forms. However, caution must be exercised in patients with low bone mineral density, because interference screw fixation has low stiffness in osteopenic cancellous bone. This may necessitate switching to fixation based on cortical rather than cancellous bone. Cortical bone may also be used as backup fixation (e.g., tie sutures around a screw and washer or a staple).
A graft goes through morphologic changes over time and becomes similar to a native ACL, a process termed ligamentization. This process consists of several steps, including necrosis (0 to 4 weeks), revascularization and cellular proliferation (4 to 12 weeks), and remodeling (3 to 6 months).67 Arthroscopically collected samples of patellar tendon and hamstring ACL grafts taken at 6 and 12 months after ACL reconstruction have demonstrated the amount of collagen cross-linking in the ACL graft returns to the level of native ACLs within 1 year of reconstruction.51 Ligamentization takes a longer period of time in allografts and hamstring autografts. Animal studies have shown a delay of revascularization and proliferation in allograft compared with autograft at 6 and 12 weeks of healing whereas at 52 weeks the differences are less distinct.33,66 Although labeled as ligamentization, the incorporated graft does not have the same physical properties of the native ACL. The collagen fibers of the graft are uniform in length and diameter, unlike the various fibers of the native ACL, which are able to distribute loads throughout the range of motion. Furthermore, there are different proportions of glycosaminoglycans and collagen-reducible cross-links. These can contribute to biologic failure of the graft.24 The processes of graft incorporation and ligamentization should be taken into account when determining advances in rehabilitation, as well as return to sporting activities, to prevent an early failure of the graft.
Postoperative Complications
Infection
Infection is a rare but devastating complication following ACL reconstruction. It can lead to the loss of articular cartilage and increase the risk of arthrofibrosis. Once identified, infection should be treated with prompt arthroscopic irrigation and débridement. Broad-spectrum antibiotics should be initiated until a more culture-specific regimen can be identified. If still functional, the graft can often be maintained. Risk factors for infection include previous arthroscopic or open knee surgery and tibial ACL graft fixation with a post and washer.39 In a retrospective review of 3126 ACL reconstructions, Barker and colleagues9 have identified 18 infections (0.58%). Infections occurred in 6 of 1349 allografts (0.44%), 7 of 1430 BPTB autografts (0.49%), and 5 of 347 hamstring autografts (1.44%). The most common organism was Staphylococcus aureus. The increased rate of infection in hamstring grafts was statistically significant. A higher risk of infection or need for graft removal was not seen with allografts. Another review in China demonstrated a similar rate of infection (0.52%) among 4068 patients over a 10-year period. Of these 21 infections, 20 were autologous hamstring grafts and 1 was a patellar tendon allograft.82 Katz and associates41 have reviewed 801 reconstructions and found an infection rate of 0.75% (6 patients). Their analysis showed that autograft (2 of 170) had twice the risk of infection compared with allograft (4 of 628) but this difference was not statistically significant (p = 0.77).
Stiffness
Loss of motion is the most common complication after ACL reconstruction, occurring in 4% to 35% of cases.23 The causes are often multifactorial and the aforementioned complications can all contribute to joint stiffness. Other factors include prolonged immobilization, poor patient compliance, intercondylar notch scarring, capsulitis, cyclops lesion, and reflex sympathetic dystrophy.12 Harner and coworkers31 have retrospectively reviewed 244 ACL reconstructions for postoperative stiffness and found an incidence of 11.1%. Factors associated with loss of motion included acute reconstruction less than 1 month from injury, male gender, and concomitant medial collateral ligament (MCL) repair. Shelbourne and coworkers’ retrospective review70 of 169 ACL reconstructions found that acute reconstructions are not associated with increased risk of arthrofibrosis (4%) when an accelerated postoperative rehabilitation program is followed. Loss of both extension and flexion is more common, with loss of extension thought to be more detrimental to function. A knee flexion contracture greater than 10 degrees prevents a normal gait and increases loads across the patellar femoral joint. Loss of flexion past 125 degrees interferes with activities of daily living, including sitting, stair climbing, and running. Historically, ACL reconstructions were initially immobilized and motion was slowly advanced. This led to increased rates of arthrofibrosis. Current physical therapy protocols have emphasized early range of motion, which has decreased rates of stiffness without adversely affecting clinical outcomes.
Treatment of arthrofibrosis includes physical therapy and dynamic braces. A manipulation under anesthesia may aid in the recovery of motion, especially when performed within the first 6 weeks of the postoperative course. Arthroscopic lysis of adhesions or resection of a cyclops lesion may be necessary. Loss of motion resulting from technical errors (e.g., misplaced tunnels) during the initial surgery may require revision ACL reconstruction. Administration of a tapered course of oral steroids in the early postoperative period for patients with decreased range of motion has also been described as a method to improve flexion by reducing inflammation and intra-articular scar formation.62
Extensor mechanism dysfunction is uncommon after ACL reconstruction but can play a role in the development of arthrofibrosis. Early postoperative rehabilitative protocols emphasize quadriceps strengthening. Deficits in quadriceps strength can often be found in up to 20% of patients at 6 months post–ACL reconstruction.59 Although the magnitude and incidence of quadriceps weakness decrease with time, its role in maintaining knee joint stability underscores the importance of early aggressive strengthening of this muscle group.
Graft Failure
Biologic graft failure may occur in the early postoperative course (first 6 months) before full incorporation and ligamentization. As noted, this is usually a result of an intraoperative technical error. Other causes of early graft failure include premature return to sports, infection, and graft insufficiency. Late graft failures occur in 5% to 10% of individuals who have returned to their preinjury level of activity.30,37 Spindler and colleagues73 have reviewed nine randomized controlled trials comparing patellar tendon and hamstring autografts. There was no significant difference in failure between the two choices of graft with an overall incidence of 3.6% and a minimum of 2 years of follow-up. Salmon and associates64 followed 760 ACL reconstructions over a 5-year period. They reported a 6% risk of ACL graft rupture as well as a 6% risk of contralateral native ACL injury, which was not affected by choice of patellar tendon or hamstring autograft. In the first year, there was an increased risk of graft failure on the operative knee, but by 12 months there is an equal chance of rupturing the unaffected ACL or reconstructed ACL graft. This is significantly higher than the 1.5% to 1.7% risk of primary ACL injury in a young athletic population.43 Similarly, Wright and coworkers85 have reported on data collected in the MOON (Multicenter Orthopaedic Outcomes Network) cohort study. In their report, 235 patients who underwent ACL reconstructions were followed for 2 years. There were 14 ACL injuries, 7 in the contralateral knee (3%) and 7 in the reconstructed knee (3%). Although females are 2 to 8 times more likely to tear their native ACL than their male counterparts, there does not appear to be any differences in failure rates of ACL reconstructions between males and females.64 Recent data have suggested that allograft reconstructions may suffer from a higher failure rate compared to autograft.32
Arthritis
Osteoarthritis (OA) is a common postoperative disease complicating ACL reconstructions. The risk of OA has been reported to be 50% after an ACL injury and as high as 70% when associated with a meniscal injury.26 Keays and colleagues42 followed 56 ACL reconstructions for 6 years after surgery and noted that meniscectomy and chondral damage are associated with a higher risk of tibiofemoral and patellofemoral arthritis. Øiestad and associates57 have reviewed 7 prospective and 24 retrospective studies on the development of knee OA following ACL reconstruction. At 10 years follow-up, the prevalence of radiographic OA in isolated ACL injuries was 0% to 13% and higher with combined injuries (21% to 48%). They concluded that previous data overestimated the prevalence of osteoarthritis after ACL reconstruction. No differences were seen in patients who were treated nonoperatively versus those who underwent ACL reconstruction, regardless of graft selection.
Graft-Specific Complications
Bone-Patellar Tendon-Bone Autograft
The BPTB autograft is considered the gold standard and is often the graft of choice in high-demand athletes. It is thought that the bone plug to bone tunnel healing occurs more quickly than soft tissue grafts.33 Anterior knee pain is the most frequently noted complication associated with patellar tendon autograft. Sachs and coworkers63 have studied 126 patients who had undergone BPTB autograft ACL reconstructions and found patellofemoral pain in 19% of patients, which correlated positively with a flexion contracture. Aglietti and colleagues3 reviewed their series of 226 patellar tendon ACL reconstructions and reported a 5% incidence of painful patellofemoral crepitus with pain and 20% with crepitus and no pain. In a review of nine randomized trials, Spindler found a range of anterior knee pain between 13% and 43%, with no significant differences between hamstring (HS) and BPTB autografts.73 However, all four studies that evaluated kneeling pain found significantly more pain in the patellar tendon groups (36% to 67% of patients).
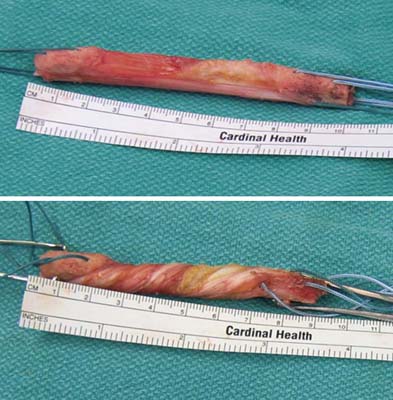
Graft tunnel mismatch is an intraoperative complication that may occur when the BPTB graft is too long and less than 20 mm of the bone plug remains within the tibial tunnel, preventing effective use of interference screw fixation. This is more likely to occur when the patellar tendon is more than 50 mm.69 Strategies to remedy this problem include recession of the graft further into the femoral tunnel, insertion of a bone plug into the tibial tunnel, and fixation at the tibia with a post and screw. Furthermore, the graft may be rotated to decrease the amount of mismatch. Rotation of 540 degrees will decrease length by 10%81 and 630 degrees by 25%,6 without any statistical difference in ultimate failure strength (Fig. 48-2). Furthermore, Barber8 reported on 50 patients who underwent flipping of the bone plug 180 degrees onto the tendon to shorten the length of tendon between bone plugs. No significant complications were found at a mean follow-up of 28 months.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree