Complications in Hallux Abducto Valgus Surgery (Excluding Hallux Varus)
Molly A. Judge
Recurrence of deformity can occur in the face of any procedure performed for the correction of the hallux abducto valgus (HAV) deformity (1,2,3,4,5 and 6). In general, these procedures are selected based upon their ability to address either structural or dynamic components of the deformity depending upon the presumptive etiology. It is common to perform both an osseous correction (structural rearrangement) and a soft tissue balancing procedure (dynamic rebalancing) in an attempt to address combination deformities. The recurrence rate after the most common of HAV procedures, the distal metaphyseal osteotomy (DMO), has been reported between 1.85% and 10% (2,3,6). Revision surgery pursued after a combination of procedures has been performed can be challenging since the normal anatomy of both soft tissue and bone has been altered. A second dissection in the same location may well increase the risk of nerve entrapment, the development of a painful or unsightly scar, vascular compromise, and wound and bone healing complications as well as the risk of chronic edema, nerve irritation or entrapment, and the development of chronic pain. In addition, as in any surgical procedure, revision surgery necessarily includes the risk of infection, overcorrection and undercorrection of the deformity.
EVALUATION
THE SUBJECTIVE COMPLAINT
While conservative measures should always be exhausted, many patients suffering from complications of HAV surgery fail at this effort when major structural complications such as hallux varus or painful sagittal plane deformities of the first ray exist. To ensure that the patient’s goals and expectations are understood, it is prudent to begin with a cursory exercise in which patients are asked to point to the target of their most important discomfort and to describe their pain in that area thoroughly. Is the target of tenderness at the first metatarsophalangeal joint (MTPJ), at the hallux interphalangeal joint (HIPJ), beneath the metatarsal head, or in a combination of areas? Often, the target of tenderness is actually beneath the second MTPJ due to the inability of the first MTPJ to bare weight. Once the location of the chief complaint is determined, the type or quality of the pain is elucidated. Certain descriptions of pain are suggestive of the etiology. Descriptors such as tingling, numbness, burning, and pins and needles sensations are often associated with entrapment neuritis or sensory neuropathy indicating that a nerve decompression may be required as a sole procedure or as an adjunctive portion of the surgical plan. When the complaint includes pain about the inferior aspect of the first MTPJ, this may indicate an abnormal articulation with a sesamoid bone or fibrous adhesions between the plantar plate and the sesamoids and therefore may require a release of the capsular and sesamoidal structures about the periphery of the MTPJ. This can result from an overaggressive medial eminence resection leaving a painful articulation between the tibial sesamoid and the inferior medial aspect of the metatarsal head (Fig. 36.1). When the patient describes a painful grinding with motion of the joint, loose bodies or intra-articular damage is likely and suggests degenerative changes of one or both chondral surfaces of the MTPJ. Such crepitation and dysfunction may indicate the need for an arthroplasty if not a joint destructive procedure depending upon the nature and extent of the chondral defects present. Tightness, cramping, and spasm of the extensor hallucis longus (EHL) tendon are often associated with lateral bow stringing of the structure and a hallux over- or underriding the second digit. These structural aberrations suggest persistent transverse plane (abduction) deformity with or without frontal plane (valgus) rotation of the hallux.
CLINICAL EVALUATION
Evaluation of recurrent or residual HAV should be performed in a stepwise fashion to most consistently identify the full extent of deformity and dysfunction. Clinical evaluation includes both weight-bearing and non-weight-bearing examinations of the foot and ankle, identical to that performed prior to firsttime elective bunion surgery. The stance evaluation is the key to determining the first ray position and alignment under normal weight-bearing conditions. Weight-bearing assessment will reveal the true nature of the deformity be it structural, dynamic, or a combination of both. Hallux varus and other planar deformities of the first ray may be unmasked in the weightbearing condition (Fig. 36.2).
So too the presence of compensatory digital deformities, such as flexor or extensor substitution and flexor stabilization, can shed light onto additional components of the functional problem. When thoroughly conducted, this portion of the clinical evaluation will demonstrate the true nature of the deformity and muscle-tendon imbalances, which will have a weighty impact on procedure selection. When the weight-bearing condition reveals shifting of load to the lesser MTPJs, it becomes obvious that the first MTPJ is dysfunctional (Fig. 36.3). The gait examination can be done strictly by visual observation or with the assistance of force plates or other computer-assisted modalities. From a practical perspective, the emphasis here will be on clinical evaluation without the benefit of additional technical support. When watching patients, it is best to be methodical and review the patients from head to toe as they walk away and walk toward their starting point. Noting posture, position, and alignment of the axial and appendicular skeleton will provide
the most comprehensive assessment. This exam should reveal a predictable heel to toe gait pattern with stride length and cadence that falls into normal parameters given the patients habitus. Taking note of shoulder, hip, and knee alignment should prompt adjunctive orthopaedic consultations as necessary. Propulsion off the first MTPJ should be easily discernable if the first ray is functioning properly. Dysfunction is obviated when propulsion is interrupted, as is the case when an abductory twist is present or if antalgia, vaulting, or splinting away from the first MTPJ is seen during the gait examination. A completely apropulsive gait will be evident when the first MTPJ is significantly subluxed, dislocated, or impinged. In addition, the weight-bearing exam reveals the extent of first metatarsal head prominence whether it is dorsal, medial, plantar, or a combination, and this helps to clarify the structural deformity present such as first metatarsal elevatus and hallux limitus, sesamoid apparatus dysfunction, or end-stage first MTPJ subluxation.
the most comprehensive assessment. This exam should reveal a predictable heel to toe gait pattern with stride length and cadence that falls into normal parameters given the patients habitus. Taking note of shoulder, hip, and knee alignment should prompt adjunctive orthopaedic consultations as necessary. Propulsion off the first MTPJ should be easily discernable if the first ray is functioning properly. Dysfunction is obviated when propulsion is interrupted, as is the case when an abductory twist is present or if antalgia, vaulting, or splinting away from the first MTPJ is seen during the gait examination. A completely apropulsive gait will be evident when the first MTPJ is significantly subluxed, dislocated, or impinged. In addition, the weight-bearing exam reveals the extent of first metatarsal head prominence whether it is dorsal, medial, plantar, or a combination, and this helps to clarify the structural deformity present such as first metatarsal elevatus and hallux limitus, sesamoid apparatus dysfunction, or end-stage first MTPJ subluxation.
The non-weight-bearing evaluation is an equally important component of the physical examination. When assessing the motion of the first MTPJ transverse, frontal and sagittal planes are considered since the deformity is typically multiplanar. Whether or not the deformity is reducible is an important clue to whether the condition is flexible enough to be corrected with revision of the original procedure (assuming a DMO and soft tissue balancing) or if an alternate procedure is warranted. The examination of the first MTPJ begins with stabilizing the first ray at the metatarsal neck and manipulating the hallux at the MTPJ level. With the foot at 90 degrees to the ankle and the subtalar joint in neutral position, the hallux is manipulated into a rectus position on the metatarsal head and sagittal plane motion is assessed in both dorsiflexion and plantarflexion. It is important to load the foot prior to evaluation to eliminate the effects of hypermobility and masking of structural deformities such as metatarsus primus elevatus. When motion is absent, limited in dorsiflexion, or restricted to solely plantarflexion, it is suspected that there is a metatarsus primus elevatus present and further study is required. If the first MTPJ motion is limited with a bone-on-bone end range of motion or when crepitation is present, a degenerative condition is suspected and significant articular defects are likely. If there is limitation with the joint held in a congruous position and a spongy end range of motion is evident, then the soft tissue structures remain suspect and revision of the lateral release and/or adductor tendon transfer may be required. If the medial column exhibits hypermobility and the first metatarsocuneiform joint (MCJ) is excessively mobile, then the peroneus longus muscle becomes ineffective at both plantarflexing the first ray and abducting the forefoot, allowing the first ray to deviate medially and rotate into varus (4,5).
To determine the transverse plane deformity, again, the first metatarsal is stabilized at the metatarsal neck. With the hallux placed into neutral position on the metatarsal head, the range of motion of the first MTPJ is then assessed. If the motion at the first MTPJ remains unrestricted with the joint in a congruous position, then the deformity is considered fully reducible and soft tissue rebalancing may be considered alone or in combination with an osseous procedure. If the joint is irreducible, then structural deformity or malposition of the first metatarsal is likely (e.g., meaningful metatarsus primus varus, adductus or a fixed sagittal plane deviation of the metatarsal bone) and an osseous procedure is probably required. If the motion at the first MTPJ is restricted due to a plantarflexed or dorsiflexed first ray segment, then structural realignment including a sagittal plane osseous procedure will be required. This can be achieved via osteotomy or a joint destructive procedure depending on the severity of the metatarsal angulation and the integrity of the articular surfaces. The decision to perform a proximal or distal procedure in this instance is determined by the degree of sagittal plane correction needed to achieve adequate first ray mobility, and radiographic evaluations will assist in making that determination.
When sagittal plane motion is restricted in the direction of dorsiflexion and point tenderness exists beneath the inferior aspect of the hallux base and/or the first metatarsal head, the sesamoid apparatus may be adhered warranting an aggressive release of both the capsular and ligamentous structures about the first MTPJ. Dorsal impingement occurs when the metatarsal head has been shifted into an elevated position and restricts sagittal plane motion. With impingement, osteophytic degeneration may prompt crepitation due to the formation of loose bodies.
Close inspection of the local anatomy will reveal whether or not an exaggerated length or angulation of the proximal phalanx
is contributing to the residual hallux abduction significantly. The influence of the HIPJ deformity may have been underestimated previously and may contribute to residual or recurrent deformity. If excessive length and abduction of the proximal phalanx are a deforming factor, a basilar phalangeal osteotomy such as an Akin procedure should be considered as this angular deviation creates a retrograde force that exacerbates the HAV deformity (6).
is contributing to the residual hallux abduction significantly. The influence of the HIPJ deformity may have been underestimated previously and may contribute to residual or recurrent deformity. If excessive length and abduction of the proximal phalanx are a deforming factor, a basilar phalangeal osteotomy such as an Akin procedure should be considered as this angular deviation creates a retrograde force that exacerbates the HAV deformity (6).
Mobility or laxity at the level of the first metatarsal cuneiform joint (MCJ) and the medial aspect of the naviculocuneiform joint should be assessed to determine if in fact there is a more proximal joint contributing to the recurrence of the hallux abductus deformity (7,8 and 9). If the MCJ is semirigid or immobile, then it may be impossible to reduce the transverse plane deformity of the metatarsal, leaving the sesamoid apparatus rotated in a lateral position as compared with the metatarsal head. Should excessive laxity exist at this joint level, the incidence of recurrent HAV deformity is predictable (10). Plain radiographs may reveal an abnormal angulation of the articular facets at the first MCJ, which is felt to be contributory to hypermobility in the proximal first ray (11,12). While it is generally understood that the primary source of motion within the first ray during propulsion occurs at the medial naviculocuneiform joint, the precise clinical measurement of this joint motion remains difficult to perform and even more difficult to reproduce in everyday practice (13,14). Normal parameters of motion within the medial column have been defined as 12.3 degrees at the medial naviculocuneiform joint and 5 degrees at the first metatarsocuneiform joint (13). Should the clinical exam reveal increased mobility at these joint levels in the face of a recurrent HAV deformity, strong consideration for selecting a proximal medial column arthrodesis is suggested. This may include arthrodesis of one or both of the most proximal medial column joints: the metatarsocuneiform joint and/or the naviculocuneiform joint.
RADIOGRAPHIC EVALUATION
Weight-bearing radiographs obtained in multiple orthogonal planes, in addition to oblique and axial views of the forefoot, will elucidate the degree of intra-articular derangement. The intermetatarsal angle (IMA) and associated length patterns of the first metatarsal and proximal phalanx are important radiographic parameters in determining the need for structural correction. Should the length of the first metatarsal bone be insufficient to maintain adequate weight-bearing function, sub two transfer lesions may be present.
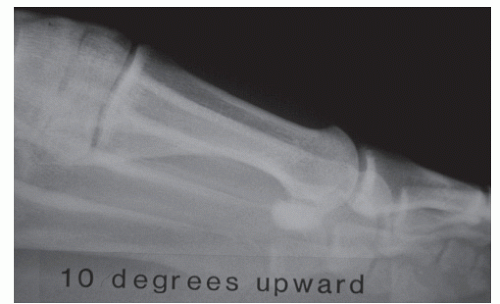
A lateral view of the first MTPJ often reveals derangement such as joint space narrowing, periarticular osteophytes, or an elevated metatarsal (or elevated metatarsal head after a DMO procedure) position that may not be appreciated in the clinical exam. It should be noted that poor technique when positioning the x-ray tube head for the lateral radiograph can create a virtual metatarsal elevatus; for example, when the tube head is positioned 10 degrees caudal to the lateral foot, the first ray will appear to be elevated (Fig. 36.4). The tube head must be positioned parallel to the weight-bearing surface and perpendicular to the lateral foot to reveal the true angular relationship between the first and second rays. When there is a divergence between the first and second dorsal cortices of the metatarsal bones, the question becomes whether the deformity is positional, as in a forefoot varus, or if it is structural and due to deformity of the bone itself (15). Both intrinsic and extrinsic deformities have the potential to be nonreducible and so either may require an osseous procedure for correction. Often as a complication of HAV surgery, the first metatarsal may be elevated due to an intrinsic change in bone structure. This iatrogenic deformity will mandate an osseous procedure when the degree of elevatus disrupts joint function (15,16) (Fig. 36.5). Once the presence of a first metatarsal elevatus has been identified, a stress lateral radiograph can be used to evaluate whether
the deformity is reducible allowing adequate joint function. This weight-bearing view will help to determine the extent to which the first MTPJ can be reduced and the degree of plantarflexion, if any, that will be required to restore joint function (Fig. 36.6).
the deformity is reducible allowing adequate joint function. This weight-bearing view will help to determine the extent to which the first MTPJ can be reduced and the degree of plantarflexion, if any, that will be required to restore joint function (Fig. 36.6).
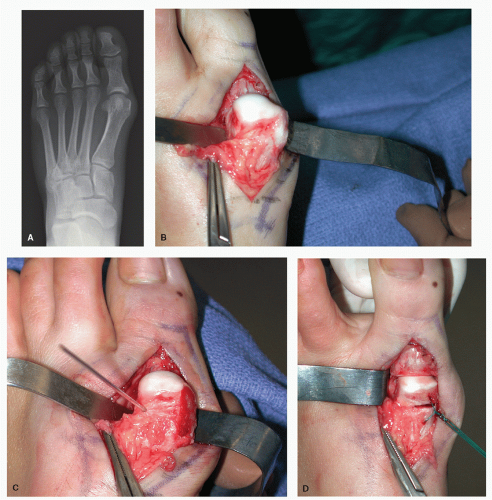
Determining whether the first MTPJ is deviated, subluxed, or congruent or if an abnormality of the proximal articular set angle (PASA) is present is an integral exercise in determining the contributory features of joint malalignment (17). With close inspection of the dorsoplantar (DP) film, the morphology of the articular surface and condition of the subchondral plate can be estimated considering the presence of sclerotic changes and irregularities about the metatarsal head and phalangeal base. When the distal-most aspect of the metatarsal head appears skewed, the cartilage is suspected to be deviated. While cartilage itself is not visible on plain radiographs, the position and alignment of the subchondral bone lend insight as to whether there is an angular deformity of this surface. Often, the appearance of an abnormal PASA is overestimated by plain radiographs, but when intraoperative findings conclude that cartilage malalignment exists, a cartilage realignment procedure will be necessary to achieve a congruous joint (Fig. 36.7). Should there be significant evidence of subchondral cystic degeneration, sclerosis, unusual derangement in morphology, or literal collapse of the metatarsal head, a dysvascular condition is suspected and further study may be required.
If there is serious concern regarding perfusion to the forefoot, then noninvasive vascular studies such as pulse volume recordings, photoplethysmography, ankle-brachial index, arterial Doppler and transcutaneous oxygen pressure (TCPO2) measurements, and vascular consultation are warranted. Ancillary imaging via magnetic resonance imaging (MRI) or nuclear medicine imaging (NMI) will demonstrate whether healthy perfusion is evident or if a dysvascular condition exists. Of added benefit is the fact that both modalities can be used to rule out the coincidence of an infectious process. Should an infection be identified, a staged procedure is required to eradicate infection before definitive structural correction is pursued. In this instance, the emphasis is on expertly obtained bone and soft tissue cultures to confirm the presence of infection and antibiotic sensitivity when it exists. Ascertaining this information is critical prior to procedure selection. When chronic edema, discoloration, unusual coolness, or cyanosis exist, it is prudent to pursue vascular consultation with the benefit of noninvasive vascular testing including TCPO2 measurements to assess healing potential for the forefoot and digits. Vasospastic conditions can impair the ability of bone to heal, and prophylactic vasodilatory medications can be used during the perioperative period to override this condition. Cold water immersion stress studies can be completed to determine the significance of this condition when it exists (18,19 and 20). Identification of decreased perfusion and reduced healing potential will increase the risk of developing a chronic nonhealing wound and may prompt serious postoperative complications threatening more proximal amputation.
Cortical hypertrophy of adjacent metatarsal shafts 2 and 3 may also reflect the lateral transfer of weight-bearing away from the first MTPJ indicating stress fractures or at least stress deformation of the metatarsal(s). This finding suggests that a reconstructive procedure to restore weight-bearing function of the first ray is in order. This is often the case when the first ray is shortened and/or elevated resulting in first MTPJ dysfunction and compensatory weight transfer to the lesser metatarsal phalangeal joints. Understanding the extent to which the length pattern of the first ray contributes to dysfunction is critical to procedure selection. The metatarsal parabola can be readily evaluated on the dorsal plantar radiograph, and the presence of a shortened first ray segment is often a harbinger for the need of a modified distal osteotomy technique or in more severe cases of shortening other lengthening procedures, which may require bone graft material (autogenous or allergenic) or the callus distraction (bone transport) technique for restoring weight-bearing potential to the great toe joint. Each of these special techniques will shift the risk:benefit ratio into a negative direction since these procedures are more complex and their outcomes are less predictable than other more traditional HAV correction techniques.
The radiographic position of the sesamoid apparatus as we have come to learn is most reflective of a malposition or residual deviation of the metatarsal head medially (21) and is often accompanied by significant lateral contractures due to
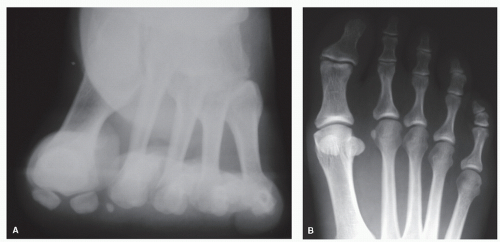
insufficient capsular and ligamentous release or from adhesion and fibrosis due to previous surgery. Performing a sesamoid axial radiograph will reveal whether or not the sesamoid position is actually associated with incongruence at the level of the cristae within the sesamoid apparatus (22). This view is particularly helpful when considering the need for revisional lateral release and mobilization of the intrinsic musculature (Fig. 36.8). When there is congruency of the sesamoids and the cristae as seen on the forefoot axial (aka sesamoid axial), a revisional lateral dissection may be avoided.
insufficient capsular and ligamentous release or from adhesion and fibrosis due to previous surgery. Performing a sesamoid axial radiograph will reveal whether or not the sesamoid position is actually associated with incongruence at the level of the cristae within the sesamoid apparatus (22). This view is particularly helpful when considering the need for revisional lateral release and mobilization of the intrinsic musculature (Fig. 36.8). When there is congruency of the sesamoids and the cristae as seen on the forefoot axial (aka sesamoid axial), a revisional lateral dissection may be avoided.
PROCEDURE SELECTION
Complications occurring during the index procedure in correcting the HAV deformity are addressed immediately during surgery. While there are a host of potential complications that can occur, misadventures in distal metaphyseal osteotomies are often due to poor planning and placement of the osteotomy itself. The nuances of creating the V osteotomy have been detailed to include proper positioning of the osteotomy within the metatarsal head to avoid placing in the cuts too far proximal or distal within the metatarsal head as each extreme in positioning carries with it different potential complications (23). When placed too far proximally, a large amount of the osteotomy rests in diaphyseal bone and so has a higher potential for nonunion or malunion of bone. Should the osteotomy be made too far distal, the potential for splitting the metatarsal head and creating an intra-articular fracture is a reality (Fig. 36.9).
Procedure selection is based upon the nature of the residual deformity and dysfunction. If an appropriate procedure was selected initially, then revision surgery may be a matter of simply performing the same in a more aggressive manner. Revision surgery for overcorrection may be a matter of reversing the
original procedure to affect a more appropriate structural or dynamic correction of deformity whichever the case may be. The original procedure may have compromised the condition of bone, intrinsic musculature, ligaments, neurovascular elements, or a combination of these, and for that reason, revision surgery always carries a worse risk:benefit ratio than the initial procedure. Should there be evidence of significant neurovascular compromise, alternate medical consultations should be pursued in advance of conducting revision surgery. Any history or overt evidence of complex conditions such as reflex sympathetic dystrophy or chronic regional pain syndrome should be considered a contraindication to further surgery and merits referral to a neurovascular specialist or pain management expert. When these conditions exist, it is wise to refer the patient for a second opinion as a precursor to any further consultations for revisional surgery.
original procedure to affect a more appropriate structural or dynamic correction of deformity whichever the case may be. The original procedure may have compromised the condition of bone, intrinsic musculature, ligaments, neurovascular elements, or a combination of these, and for that reason, revision surgery always carries a worse risk:benefit ratio than the initial procedure. Should there be evidence of significant neurovascular compromise, alternate medical consultations should be pursued in advance of conducting revision surgery. Any history or overt evidence of complex conditions such as reflex sympathetic dystrophy or chronic regional pain syndrome should be considered a contraindication to further surgery and merits referral to a neurovascular specialist or pain management expert. When these conditions exist, it is wise to refer the patient for a second opinion as a precursor to any further consultations for revisional surgery.
The types of surgical procedures available in addressing complications of HAV surgery are no different than those available for the initial surgery, and they fall into a number of categories including reconstructive and joint destructive procedures. Procedures designed to salvage function of the first ray segment include the following. Joint destructive procedures such as implant arthroplasty of the first MTPJ are reserved for discussion in an alternate section of this text.
Reconstructive procedures for residual HAV deformity
Soft tissue and tendon balancing procedures
Phalangeal osteotomy of the hallux
Distal first metatarsal osteotomies
Proximal first metatarsal osteotomies
Joint destructive procedures for residual HAV deformity*
Metatarsal phalangeal joint arthroplasty
Metatarsal phalangeal joint arthrodesis
MCJ arthrodesis
EARLY COMPLICATIONS
In the early postoperative period, within the first 21 days, soft tissue adhesion and fibrosis do not significantly interfere with reduction of the deformity. In this early period, bone healing consists of blood clot formation that is gradually replaced by highly vascular connective tissue. This connective tissue becomes infiltrated by fibrocartilage over time and develops into a provisional bone callus. At this early stage, the callus serves as a flexible bone bridge not yet ossified and is relatively malleable. Complications that occur during the first few weeks after surgery are often due to overt trauma or patient noncompliance. This situation is met when the patient experiences either unexpected trauma or is grossly negligence in self-care (e.g., another person accidently stepping on the patients’ foot after recent HAV surgery) or when unusual weight-bearing activities (e.g., aggressive walking, running, deep squatting, ladder climbing, or prolonged kneeling) cause disruption of the osteotomy or disturb soft tissue balance. In these circumstances, there are three principal goals to be achieved to salvage the function of the first ray: (a) evacuation of hematoma, eradication of infection, and resolving incision dehiscence; (b) open reduction and internal fixation (ORIF) of the disrupted bone with or without bone graft; and (c) revision of soft tissue rebalancing such as revising the medial capsulorrhaphy or adductor tendon transfer depending on the original procedure performed. Each may be a necessary adjunctive procedure in circumstances that arise unexpectedly resulting in early recurrence of deformity (Fig. 36.10).
CORRECTION OF DELAYED RECURRENCE
SOFT TISSUE IMBALANCE AND RESIDUAL SESAMOID DISPLACEMENT
Whenever possible, an extension of the original incision line is used to access the first MTPJ and the intermetatarsal space. The revisional incision should begin approximately 1 cm more proximal than the original incision and extends a similar distance beyond the most distal extent. This will allow the surgeon to identify, both proximally and distally, the zones of transition between normal anatomy and that violated by previous dissection. Starting the dissection proximally in healthy tissue will make it easier to become oriented in the soft tissue planes before pursuing the remainder of the exploration. In particular, identifying predictable dorsal cutaneous nerves at this level will help to identify evidence of nerve entrapment due to adhesions and fibrotic changes resulting from prior manipulation or violation. Dissection is likely to be difficult due to the presence of this aberrant soft tissue layer. Care should be taken to explore for the presence of entrapped cutaneous nerves and when present nerve decompression should be completed with exploration along the full length of the affected nerve until reconstitution of normal nerve tissue is identified. Often, a two-layer dissection is prepared with the dermis and superficial subcutaneous structures being prepared as a single layer. The deep fascia is dissected as the second layer and is meticulously prepared to preserve a solid plane of tissue for closure over the affected bone and joint. In cases in which adhesions and fibrotic changes are profound, it may be necessary to create one sharp incision to the deep fascia.
When residual sesamoid displacement exists after a modified McBride-type bunionectomy, the culprit for recurrence is likely an insufficient lateral release. The enthesis of the common adductor tendon is through attachments at the phalangeal base, the plantar plate, and sesamoid apparatus. Depending on the severity of the underlying deformity, the sesamoid apparatus may have retained fibrosis or adhesions to the plantar and lateral intrinsics preventing long-term realignment of the plantar plate. To ensure adequate lateral release, dissection of the first intermetatarsal space and exploration of the lateral MTPJ are required. The fibular sesamoid is a complex region of intrinsic
attachments and includes the lateral head of flexor hallucis brevis (FHB) tendon, the deep transverse intermetatarsal ligament (DTIL), the common tendon (oblique and transverse) of the adductor hallucis and fibrous bands that extend from the sesamoid apparatus into the flexor digitorum longus tendon, and the superficial plantar aponeurosis (24). Since the sesamoids and plantar plate are intra-articular structures with many intrinsic attachments, identification and isolation of the lateral joint capsule in the region of the enthesis is a critical first step in this process. The region of the first MTPJ is exposed, and the lateral aspect of the joint space is identified by placing distal traction on the hallux to cause a puckering of the joint capsule. This maneuver facilitates identification of the lateral joint space where the intrinsic structures can be found as they attach to the base of the proximal phalanx, sesamoid apparatus, and plantar plate. Delineating this joint level allows for proper placement of a capsulotomy via a stab incision. Once performed, any residual intrinsic attachments can be undermined and transected from their entheses liberating the hallux and sesamoid apparatus. Manual manipulation of the hallux into extreme varus will break through any remaining fibrous banding that may exist deep within the lateral joint. Modifications of the capsulotomy include making a larger more vertically oriented capsular incision or simply fenestrating the lateral joint capsule and then allowing manual manipulation of the hallux to break through residual lateral ligamentous structures (25). If there is evidence that the adductor tendon remains attached at the proximal phalanx base, this structure should be grasped, undermined, and transected or dissected out proximally and prepared for later transfer. The use of an adductor transfer to the medial capsule for supplementation of the medial capsule repair may be an important adjunctive procedure in the face of recurrent HAV. Whether this structure is transferred dorsally to the medial capsule or run through the neck of the first metatarsal, the end result is supplementation of the medial capsulorrhaphy while creating a change in muscle balance countering adductus or varus shift of the first metatarsal. This technique has been called into question by some as the benefits of the adductor have never been scientifically born out in the literature, and in fact, one series concluded that this maneuver provided no added benefit when performed with a DMO (26).
attachments and includes the lateral head of flexor hallucis brevis (FHB) tendon, the deep transverse intermetatarsal ligament (DTIL), the common tendon (oblique and transverse) of the adductor hallucis and fibrous bands that extend from the sesamoid apparatus into the flexor digitorum longus tendon, and the superficial plantar aponeurosis (24). Since the sesamoids and plantar plate are intra-articular structures with many intrinsic attachments, identification and isolation of the lateral joint capsule in the region of the enthesis is a critical first step in this process. The region of the first MTPJ is exposed, and the lateral aspect of the joint space is identified by placing distal traction on the hallux to cause a puckering of the joint capsule. This maneuver facilitates identification of the lateral joint space where the intrinsic structures can be found as they attach to the base of the proximal phalanx, sesamoid apparatus, and plantar plate. Delineating this joint level allows for proper placement of a capsulotomy via a stab incision. Once performed, any residual intrinsic attachments can be undermined and transected from their entheses liberating the hallux and sesamoid apparatus. Manual manipulation of the hallux into extreme varus will break through any remaining fibrous banding that may exist deep within the lateral joint. Modifications of the capsulotomy include making a larger more vertically oriented capsular incision or simply fenestrating the lateral joint capsule and then allowing manual manipulation of the hallux to break through residual lateral ligamentous structures (25). If there is evidence that the adductor tendon remains attached at the proximal phalanx base, this structure should be grasped, undermined, and transected or dissected out proximally and prepared for later transfer. The use of an adductor transfer to the medial capsule for supplementation of the medial capsule repair may be an important adjunctive procedure in the face of recurrent HAV. Whether this structure is transferred dorsally to the medial capsule or run through the neck of the first metatarsal, the end result is supplementation of the medial capsulorrhaphy while creating a change in muscle balance countering adductus or varus shift of the first metatarsal. This technique has been called into question by some as the benefits of the adductor have never been scientifically born out in the literature, and in fact, one series concluded that this maneuver provided no added benefit when performed with a DMO (26).
The condition of the sesamoid apparatus should be inspected to ensure that there is adequate mobility of the sesamoids. It is understood that relocation of the first metatarsal is impeded by fibrosis and adhesion of the sesamoid apparatus, and so this is an important portion of the procedure. If the fibular sesamoid appears to be grossly hypertrophic and abnormally fixed in position, then the need for a fibular sesamoidectomy should be entertained. Once the fibular sesamoid is mobilized or excised, the first MTPJ may be manipulated to check for reducibility in the transverse plane. If it is impossible to reduce the hallux valgus deformity due to a residual or nonreducible metatarsus adductus or metatarsus varus, the MCJ should be reassessed to rule out residual contractures or degenerative joint changes interfering with joint mobility. Weight-bearing may be simulated on the operating table to evaluate the degree of reduction achieved from the soft tissue release alone. Any residual contractures of the EHL tendon or first MTPJ capsule will be evident and should be addressed via lengthening techniques in lieu of capsulotomy or tenotomy. By performing a controlled tissue lengthening, physiologic tension can be achieved and is preferred to simple release. To address residual EHL contracture, a Z lengthening will allow sufficient relaxation for neutral position and alignment of the great toe. It is important to perform the MTPJ capsulotomy in the plane of the contracture to correct the deformity at its apex. Although numerous techniques have been suggested, a simple V to Y capsulotomy will release contracture, and the capsule closure can be performed under physiologic tension with the hallux in neutral alignment on the metatarsal head.
At this point, the residual deformity is assessed and whether or not to perform a metatarsal osteotomy or a more proximal procedure is considered. It is generally understood that performing a metatarsal osteotomy in the face of a fibular sesamoidectomy increases the risk of developing a hallux varus deformity (see Chap. 37), and so caution is advised and judicious use of this combination of procedures is recommended. The detailed execution of specific osteotomies and their modifications in performing the distal or proximal metaphyseal osteotomy, midshaft metatarsal osteotomy, first MCJ arthrodesis, and their modifications can be found in alternate chapters of this text.
PHALANGEAL OSTEOTOMY OF THE HALLUX
When the apex of deformity is within the hallux itself, an Akin osteotomy may be effective in correcting the condition. An unusually long hallux or high angulation hallux interphalangeus are typical criteria for use of this adjunctive technique. The original procedure described by Akin included resection of the medial eminence of the first metatarsal head, resection of the medial phalangeal base, and wedge osteotomy of the proximal hallux (27). While the original procedure was extensive, current modifications include simply creating an oblique base wedge osteotomy (short or long) or a transverse osteotomy within the proximal phalanx of the hallux. This technique should not be used as a primary procedure to correct an increased IMA or deformity due to an abnormal PASA deformity. When used inappropriately, the Akin procedure may create enough retrograde pressure on the metatarsal head to exaggerate the lateral deviation of the first metatarsal perpetuating deformity (28,29,30,31 and 32).
The use of this osteotomy is usually an intraoperative consideration when there is residual lateral deviation of the hallux noted after a primary bunion procedure has been performed, that is, first metatarsal osteotomy with muscle tendon balancing.
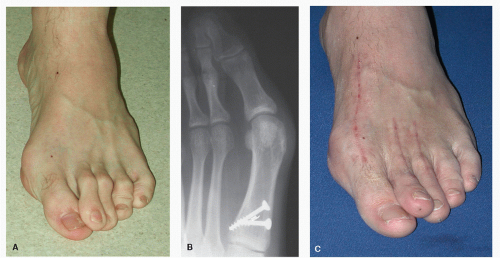
A high angulation hallux abductus interphalangeus, a long medial border of the proximal phalanx of the hallux, or an increased distal articular set angle may be responsible for this residual deformity (Fig. 36.11). By derotating the hallux medialward using the Akin osteotomy, the long tendons of the flexor and extensor tendons will be relocated more centrally about the HIPJ and the metatarsal phalangeal joint reducing the retrograde force that aggravates recurrence of HAV deformity.
Technique
The skin incision should provide ample exposure for preparation of the osteotomy and allow for ease of application of fixation. A linear incision along the dorsomedial aspect of the hallux or one that divides the dorsal and plantar skin is often sufficient for execution of the procedure. An optimal incision plan incorporates the original incision allowing for exposure of the first MTPJ and the distal 1/3 of the proximal
phalanx. Sharp and blunt dissection is used to get through the subcutaneous tissue envelope, which is naturally asthenic in this region. Due to the thin dermal and subcutaneous layers, meticulous handling is important to avoid necrosis of the wound margins from overaggressive retraction. Using the blunt end of Regnauld retractors is effective for this dissection. All four of the very delicate digital neurovascular elements within this region are invariably manipulated since the most medial and lateral borders of the phalanx must be exposed throughout the procedure. Once the first MTPJ and body of the proximal phalanx have been exposed, a linear incision is made extending from the dorsum of the first MTPJ onto the distal 1/3 of the phalangeal body. It is best to begin this incision proximally along the medial border of the EHL tendon. The periosteum is reflected sharply about the proximal phalanx base, while blunt reflection over the central and distal aspects of the phalanx can be managed with a freer elevator. Preparation of this soft tissue layer is an important portion of the procedure as it will allow for thorough coverage of the osteotomy site and fixation devices during closure. This coverage will prevent adhesion formation between the osteotomy site and the long extensor tendon. The metaphyseal-diaphyseal junction of the phalangeal base is identified, isolated, and scored with marking pen to provide two important landmarks. The first landmark is a horizontal line that parallels the base of the proximal phalanx approximately 0.5 to 1.0 cm from the first MTPJ. This is the most proximal area for screw or pin placement without risking violation of the articular surface. The second landmark is drawn to create a transverse or oblique arm for a closing base wedge osteotomy (CBWO). The length and angulation of this osteotomy will depend upon the degree of reduction needed to realign the hallux. One method to determine the size of the wedge resection is to measure the difference between the medial and lateral cortical margins. This difference should provide adequate reduction of hallux deviation while creating a more parallel relationship between the distal and proximal articular surfaces of the hallux (Fig. 36.12A). This medially based wedge can be expected to heal promptly when placed within the metaphyseal region of bone. The longer and more oblique the cut, the more diaphyseal bone involved, and rigid internal fixation is integral to facilitate primary bone healing in this region. An axis guide is placed in the proximal lateral corner of the metaphyseal diaphyseal junction and is drilled from dorsal to plantar using a 0.045-inch Kirschner wire (K-wire) (Fig. 36.12B) Just
as in a CBWO for the first metatarsal, the guide wire can be angulated to provide sagittal plane correction; however, since this is a medially based wedge, the orientations to achieve plantarflexion or dorsiflexion of the part are opposite. Tilting the axis guide lateralward will effect elevation of the distal segment and may be efficacious when hallux limitus is coincident. An axis guide tilted medially will affect plantarflexion while tilting the axis distally will reduce valgus deviation of the hallux. Once proper placement of the axis guide is determined, the osteotomy is scored using a no. 10 osteotome and a mallet. Once satisfied with the orientation of the proposed osteotomy, power instrumentation is used to cut the osteotomy. An oscillating saw
held parallel to the axis guide will allow for a well-controlled cut. The maximum depth of the proximal phalanx is approximately 1.0 cm, and so a fine-tooth blade that is 1.0 cm wide and at least 1.0 cm long will facilitate this maneuver. Constant irrigation during the osteotomy will minimize thermal necrosis and improve the setting for bone healing. The lateral hinge of the osteotomy provides a second point of fixation, and so care is taken to preserve this structure during provisional fixation. Final assessment of correction should be completed prior to applying definitive fixation devices. While the fixation of an Akin osteotomy is a matter of surgeon’s preference, the long oblique modification allows for rigid internal fixation with the benefit of a 2.7-mm cortical screw. Numerous alternate types of fixation have been used for this procedure such as staples, K-wires, cannulated screws, and absorbable screws and pins. Since full visualization of the entrance and exit of the screw is easily achieved, standard screws are the mainstay for this procedure. In the face of a transverse osteotomy, bone coaptation and rigid fixation can be achieved with the benefit of the twopoint cerclage technique, parallel staples, or K-wires. Once satisfied with correction of the deformity and stabilization of the osteotomy, a layered closure can be completed after copious irrigation. A meticulous layered closure will reduce the risk of wound dehiscence. Immediate weight-bearing in a rigid-soled or orthowedge surgical shoe for 6 weeks or until adequate bone consolidation is appreciated both clinically and radiographically (Fig. 36.12C and D). Potential complications of the procedure include fracturing of the lateral hinge or failure of fixation devices in either transverse or oblique osteotomies. If failure of fixation occurs, then the addition of supplemental fixation devices can be done percutaneously. Some would argue that simply splinting the hallux or providing a more aggressive off loading of the hallux will allow bone union to complete in a primary or secondary fashion.
phalanx. Sharp and blunt dissection is used to get through the subcutaneous tissue envelope, which is naturally asthenic in this region. Due to the thin dermal and subcutaneous layers, meticulous handling is important to avoid necrosis of the wound margins from overaggressive retraction. Using the blunt end of Regnauld retractors is effective for this dissection. All four of the very delicate digital neurovascular elements within this region are invariably manipulated since the most medial and lateral borders of the phalanx must be exposed throughout the procedure. Once the first MTPJ and body of the proximal phalanx have been exposed, a linear incision is made extending from the dorsum of the first MTPJ onto the distal 1/3 of the phalangeal body. It is best to begin this incision proximally along the medial border of the EHL tendon. The periosteum is reflected sharply about the proximal phalanx base, while blunt reflection over the central and distal aspects of the phalanx can be managed with a freer elevator. Preparation of this soft tissue layer is an important portion of the procedure as it will allow for thorough coverage of the osteotomy site and fixation devices during closure. This coverage will prevent adhesion formation between the osteotomy site and the long extensor tendon. The metaphyseal-diaphyseal junction of the phalangeal base is identified, isolated, and scored with marking pen to provide two important landmarks. The first landmark is a horizontal line that parallels the base of the proximal phalanx approximately 0.5 to 1.0 cm from the first MTPJ. This is the most proximal area for screw or pin placement without risking violation of the articular surface. The second landmark is drawn to create a transverse or oblique arm for a closing base wedge osteotomy (CBWO). The length and angulation of this osteotomy will depend upon the degree of reduction needed to realign the hallux. One method to determine the size of the wedge resection is to measure the difference between the medial and lateral cortical margins. This difference should provide adequate reduction of hallux deviation while creating a more parallel relationship between the distal and proximal articular surfaces of the hallux (Fig. 36.12A). This medially based wedge can be expected to heal promptly when placed within the metaphyseal region of bone. The longer and more oblique the cut, the more diaphyseal bone involved, and rigid internal fixation is integral to facilitate primary bone healing in this region. An axis guide is placed in the proximal lateral corner of the metaphyseal diaphyseal junction and is drilled from dorsal to plantar using a 0.045-inch Kirschner wire (K-wire) (Fig. 36.12B) Just
as in a CBWO for the first metatarsal, the guide wire can be angulated to provide sagittal plane correction; however, since this is a medially based wedge, the orientations to achieve plantarflexion or dorsiflexion of the part are opposite. Tilting the axis guide lateralward will effect elevation of the distal segment and may be efficacious when hallux limitus is coincident. An axis guide tilted medially will affect plantarflexion while tilting the axis distally will reduce valgus deviation of the hallux. Once proper placement of the axis guide is determined, the osteotomy is scored using a no. 10 osteotome and a mallet. Once satisfied with the orientation of the proposed osteotomy, power instrumentation is used to cut the osteotomy. An oscillating saw
held parallel to the axis guide will allow for a well-controlled cut. The maximum depth of the proximal phalanx is approximately 1.0 cm, and so a fine-tooth blade that is 1.0 cm wide and at least 1.0 cm long will facilitate this maneuver. Constant irrigation during the osteotomy will minimize thermal necrosis and improve the setting for bone healing. The lateral hinge of the osteotomy provides a second point of fixation, and so care is taken to preserve this structure during provisional fixation. Final assessment of correction should be completed prior to applying definitive fixation devices. While the fixation of an Akin osteotomy is a matter of surgeon’s preference, the long oblique modification allows for rigid internal fixation with the benefit of a 2.7-mm cortical screw. Numerous alternate types of fixation have been used for this procedure such as staples, K-wires, cannulated screws, and absorbable screws and pins. Since full visualization of the entrance and exit of the screw is easily achieved, standard screws are the mainstay for this procedure. In the face of a transverse osteotomy, bone coaptation and rigid fixation can be achieved with the benefit of the twopoint cerclage technique, parallel staples, or K-wires. Once satisfied with correction of the deformity and stabilization of the osteotomy, a layered closure can be completed after copious irrigation. A meticulous layered closure will reduce the risk of wound dehiscence. Immediate weight-bearing in a rigid-soled or orthowedge surgical shoe for 6 weeks or until adequate bone consolidation is appreciated both clinically and radiographically (Fig. 36.12C and D). Potential complications of the procedure include fracturing of the lateral hinge or failure of fixation devices in either transverse or oblique osteotomies. If failure of fixation occurs, then the addition of supplemental fixation devices can be done percutaneously. Some would argue that simply splinting the hallux or providing a more aggressive off loading of the hallux will allow bone union to complete in a primary or secondary fashion.
Pearls/Pitfalls
The oblique osteotomy is less stable than its transverse counterpart. Therefore, when the lateral hinge is lost, the entire construct becomes markedly less stable. This would change the degree of protected weight-bearing or digital splinting required to achieve bone union.
CONSIDERATIONS IN SALVAGE AFTER AN OVERLY AGGRESSIVE OSTECTOMY
When HAV surgery is complicated by an overly aggressive medial exostectomy, one of two conditions may develop: undercorrection or overcorrection of the transverse plane deformity or residual hallux valgus or hallux varus. Hallux varus as a complication of HAV surgery is discussed specifically in Chapter 36. When undercorrection is the result, it is likely that the original deformity was underestimated and an insufficient procedure was selected. Stretching the indications for the use of conservative bunion surgery is doomed to failure in the face of a high IMA or excessive hallux abductus angle or when significant metatarsus primus adductus, metatarsus adductus, increased proximal articulation set angle, or a combination of these exists. An overly aggressive exostectomy is often an attempt to further reduce medial metatarsal prominence when the index osteotomy/ostectomy failed to provide this correction. This medial scalloping of the metatarsal rarely achieves the desired effect of eliminating the structural deformity and so results in persistent or recurrent hallux valgus with a significant loss of bone volume from the metatarsal head.
The conservative bunion surgery aka exostectomy is intended to remove the excess medial eminence without violating the articulation of the tibial sesamoid. Salvage of this condition requires a combination of procedures: one to restore the articular surface of the metatarsal head and the other to achieve definitive correction of the first ray alignment. Determining the procedure for correcting first ray alignment is dependent upon function of the first MTPJ, degree of residual MTPJ incongruity, degree of first metatarsal malalignment, and medial column stability not unlike selecting a primary bunion procedure.
Technique
Metatarsal head grafting
One viable technique for salvage of the first MTPJ function after an overaggressive exostectomy is to graft the metatarsal head and restore a more normal cubic content for articulation with the phalanx. When reinforcing the region with bone graft, the convex surface of the metatarsal head is supplemented and a foundation for the phalangeal base articulation is restored (33). The purpose of this technique is to create a more normal morphology to the first metatarsal head allowing for congruous articulation with the hallux base and was originally described to reverse the ill effects of hallux varus resulting from HAV surgery. Once the surface area of the metatarsal head has been restored, the metatarsal segment can be realigned with a combination of osseous and soft tissue procedures as necessary. This may require the benefit of a proximal metatarsal osteotomy and release of contractures within the first intermetatarsal space depending on the severity of the residual deformity.
Resectional arthroplasty of phalanx
After an overaggressive exostectomy, a joint salvage procedure may not be possible. In bedridden, wheelchair-bound, or low-demand, sedentary patients, an arthroplasty to remove the phalangeal base, the Keller procedure, may be enough to reduce the deformity, eliminate painful bone prominence, and reduce risk of ulceration (34). In select patients, the Keller procedure can provide an apropulsive gait that allows for effective weight transfers and pivoting necessary for basic low-weight-bearing daily activities. Care should be taken to perform a meticulous capsulorrhaphy and include reattachment of the long flexor tendon for optimal stabilization of the hallux. This tendon transfer will provide enhanced stability reducing the risk of hallux contracture after surgery. Performing a combination of purse stringing the joint capsule and reattaching either the short or long flexor tendon to the residual phalanx will prevent hallux extensus deformity (35,36).
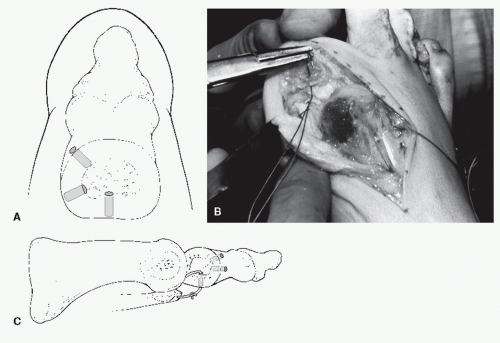
With reattachment of the short flexor tendon, the sesamoid apparatus is firmly supported, and it is felt that this serves to prevent joint subluxations that contribute to lesser metatarsalgia (Fig. 36.13). Although there are no strict contraindications for the Keller procedure, the relative contraindication is the presence of chronic lesser metatarsalgia in the absence of hammertoe contractures and instability of the first ray segment. When excessive bone loss results in instability of the MTPJ, it may not be possible to re-create a supporting surface for the hallux base. In higher-demand patients, the Keller arthroplasty is not a functional option.
REVISIONAL DISTAL METAPHYSEAL OSTEOTOMY
Clinical Considerations
When revision of a distal osteotomy is necessary and the quality of the residual bone is in question, ancillary imaging is warranted. The benefit of three-dimensional imaging, MRI, or computed axial tomography (CAT) will identify voids and other structural defects that may not be evident on plain x-ray aiding in procedure selection. If the metatarsal head is in relatively good condition and there is little shortening of the metatarsal segment, then a revisional osteotomy may be curative. The primary risks of the procedure are increased when performing revisional surgery; infection, nerve entrapment, painful or unsightly cicatrix, chronic edema, over- or undercorrection, and delayed nonunion or malunion of bone are all possible if not even more likely in this surgery. Due to the repeated neurovascular insult, the hallux is at particular risk for compromise. Hence, meticulous dissection and bone handling are critical to success in these cases. In revisional surgery, it is prudent to discuss and reserve the right to perform a joint destructive procedure should intraoperative findings warrant it. This would dramatically change the postoperative care plan likely including a considerable period of non-weight-bearing when performed. If that nonweight-bearing plan evolves in a patient with risk factors for the development of deep vein thrombosis (DVT), then a plan for DVT prophylaxis should be pursued and communications with the primary care physician should be completed well in advance of the surgery. On a similar note, if the patient is on anticoagulant therapy, then reversal of the agent and perioperative prophylaxis becomes a major component of the surgical plan.
Technique
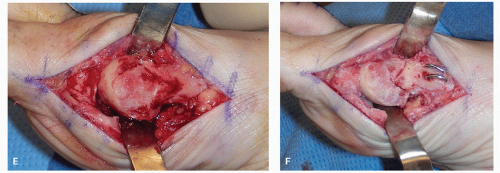
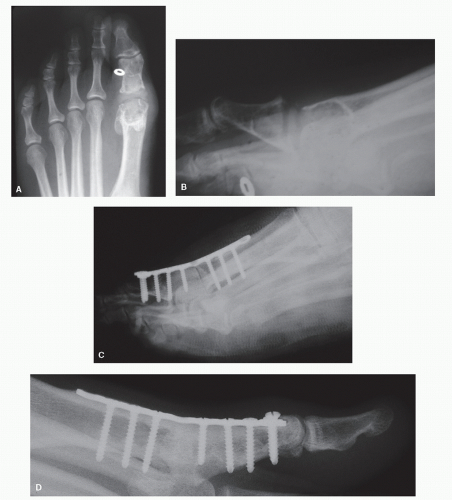
The incision takes into consideration the clinical appearance of the deformity and the most recent radiographs to ensure that exposure is optimal to execute débridement, osteotomy, and fixation (Fig. 36.14A and B). For this reason, the incision plan often includes the original cicatrix line plus extensions both proximally and distally to enhance exposure and allow for the identification of tissue planes that have not been disrupted by previous surgery. Gentle manipulation of the skin is required to prepare the skin in a single layer for retraction and exposure of the subcutaneous layers; however, when dermal atrophy is profound and the basement layer of skin is adhered to the subcutaneous layer, this may not be possible. The dorsal cutaneous nerves and vessels should be identified, isolated, and retracted whenever possible. The integrity of the EHL tendon should be assessed and may be found fibrosed to the underlying joint capsule when tendinopathy is a contributing factor (Fig. 36.14C). A layered dissection is always preferred however is not always possible in revision surgery. Often, when the surgical site is matted down due to dermal atrophy and deep adhesions or when extensive fibrosis exists, the dissection is performed using sharp incision through a single layer down to the periosteum. A dorsolinear periosteal incision is made to expose the joint, and the capsulotomy may be linear or modified into an inverted L or T configuration for best joint exposure. When the joint capsule contributes to contracture of the joint, the capsular incision should be placed strategically to facilitate relaxation of that tissue. The original osteotomy site is often easy to identify intraoperatively. It is common to find a well-defined line of sclerosis defining the margins of the capital fragment with or without exuberant osteophytic degeneration (Fig. 36.14D). Before incising the osteotomy site, it is important to inspect the articular surfaces of the metatarsal head and phalanx base to identify unusual articular defects or obvious joint incongruity. If the degenerative changes about the articular surfaces are more significant than predicted or if the bone quality is not sufficient to maintain an osteotomy (overly sclerotic or grossly osteoporotic), then consideration for an alternate procedure such as a
more proximal osteotomy should be entertained. Modification of the osteotomy, when necessary, is much easier to prepare before the original osteotomy is recut. Critical evaluation of the articular surfaces to assess the condition of the cartilage and reducibility of the MTPJ is performed prior to recutting the osteotomy. When angular deformity of metatarsal bone exists, such as sagittal plane malalignment, modifications of the osteotomy can be employed avoiding the need for a combination of osteotomies to reduce deformity (37,38).
more proximal osteotomy should be entertained. Modification of the osteotomy, when necessary, is much easier to prepare before the original osteotomy is recut. Critical evaluation of the articular surfaces to assess the condition of the cartilage and reducibility of the MTPJ is performed prior to recutting the osteotomy. When angular deformity of metatarsal bone exists, such as sagittal plane malalignment, modifications of the osteotomy can be employed avoiding the need for a combination of osteotomies to reduce deformity (37,38).
When significant angular deformity of the articular surface of the metatarsal head is evident, modification of the original osteotomy cut is warranted and a cartilage realignment procedure is necessary. When there is significant sclerosis or avascular changes present, a DMO procedure is not prudent and so close scrutiny of the bone quality is required to avoid further devitalization of the metatarsal head. There are some that would suggest performing a hallucal osteotomy in this case to realign the pull of the long flexor and extensor tendons to create a more effective tendon function across the MTPJ and reduce the angular retrograde pull that aggravates the recurrence of the HAV deformity. This avoids further violation of the metatarsal head while correcting abnormal biomechanics that perpetuate the deformity.
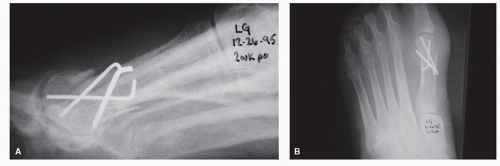
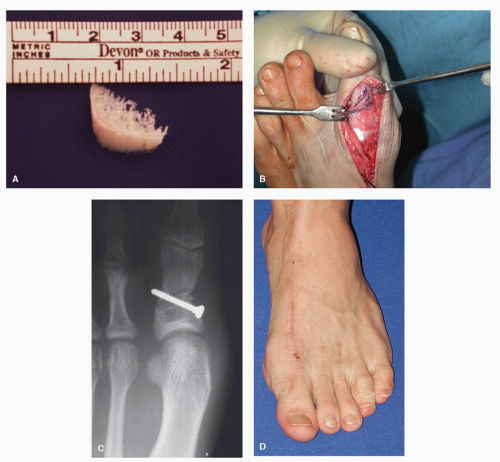
When a DMO is appropriate, an axis guide is prepared for the revision and sharp resection of the osteotomy will require power instrumentation to minimize shortening. Copious irrigation should be performed throughout the resection to prevent thermal necrosis and reduce the risk of devascularizing the metatarsal head. Depending on the quality of bone, the intramedullary segment of the metatarsal head may be manipulated into an improved position with the benefit of a freer elevator. It is important to gently manipulate this segment of bone to avoid devitalization or fragmentation of the part. When the bone quality is compromised, débridement and supplemental bone should be pursued to improve bone quality and enhance bone healing. Using graft material to pack voids within the metatarsal head, shaft, or both will often require two points of fixation to afford optimal stability of the parts and provide ample immobilization of bone to ensure bone healing. When grafting is required simply to pack voids, the fixation technique can be completed simply by using two points of fixation, for example, two parallel or crossing K-wires where the goal is to achieve a stable construct for propulsion by way of primary bone healing (Fig. 36.15A and B). This supplemental bone grafting is a very different procedure than when an interpositional bone graft technique is used for the benefit of restoring length to the first ray, and so the rationale in fixation is dramatically different between the two. See the Pearls/Pitfalls section for further discussion on this subject.
When using power instrumentation to re-create an osteotomy, especially in unusually dense and sclerotic bone, continuous irrigation is important to prevent thermal necrosis. Fenestration of the parts will facilitate vascular ingrowth and encourage enhanced perfusion to the metatarsal segments (Fig. 36.15C and D). Once the fragment has been well coapted, the articulation of the joint should be assessed. Ultimately, positioning of the revisional osteotomy should produce a congruous articulation with the hallux. If this new position is not optimal, modification of the osteotomy may be required. If excessive elevation of the metatarsal head is evident while manipulating the V-type osteotomy, enhanced plantarflexion can be achieved simply by planning the dorsal arm of the osteotomy and allowing the entire metatarsal head to drop down. The reverse maneuver will be effective when faced with extreme plantarflexion of the part. The sagittal saw blade is 1 mm thick and so removes approximately 1 mm of bone when planing the site. It is important to reevaluate the position of the osteotomy closely after each pass of the blade to prevent excessive bone
loss. Once optimal position has been achieved, the capital fragment should be manually impacted onto the shaft compressing the parts prior to preparing the fixation device(s). Fixation of the osteotomy can be completed with the benefit of a single 0.062-inch K-wire in many cases. Which fixation device and how many points of fixation are used are dependent on the overall stability of the osteotomy in the corrected position. It is prudent to challenge the osteotomy by grasping the hallux and distracting at the MTPJ while observing for evidence of insufficiency about the osteotomy site. If there is evidence of motion across the osteotomy or frontal plane instability about the capital fragment, then a second point of fixation should be employed. A final assessment of the alignment of the articular surfaces, joint motion, and hallux position should be completed after rigid fixation has been achieved to confirm optimal position and function prior to closure.
loss. Once optimal position has been achieved, the capital fragment should be manually impacted onto the shaft compressing the parts prior to preparing the fixation device(s). Fixation of the osteotomy can be completed with the benefit of a single 0.062-inch K-wire in many cases. Which fixation device and how many points of fixation are used are dependent on the overall stability of the osteotomy in the corrected position. It is prudent to challenge the osteotomy by grasping the hallux and distracting at the MTPJ while observing for evidence of insufficiency about the osteotomy site. If there is evidence of motion across the osteotomy or frontal plane instability about the capital fragment, then a second point of fixation should be employed. A final assessment of the alignment of the articular surfaces, joint motion, and hallux position should be completed after rigid fixation has been achieved to confirm optimal position and function prior to closure.
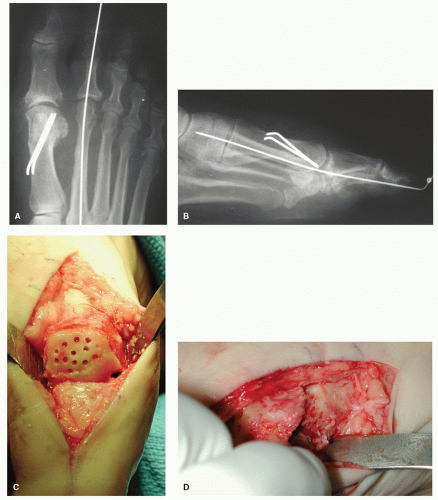 Figure 36.15 Postoperative DP (A) and lateral (B) radiographs reveal the revision of a DMO stabilized using two-point 0.062-inch K-wire fixation in osteopenic bone. Notice the improved alignment and congruity of the first MTPJ as compared with Figure 36.14B. C: Intraoperative photo showing the dorsolateral aspect of the metatarsal head is reflective of the joint impingement resulting from an iatrogenic metatarsal elevatus and subsequent hallux limitus as a complication of a proximal metatarsal osteotomy malunion. The bald chondral zone of the metatarsal head is fenestrated using a 2.0-mm wire pass drill bit (in lieu of a K-wire) to excavate bone and decompress the region to encourage vascular ingrowths. D: Distraction of the osteotomy in revision HAV surgery reveals densely sclerotic bone that has been fenestrated to encourage vascular ingrowths. |
Pearls/Pitfalls
When considerable angular deformity of the metatarsal articular surface is evident, modification of the original osteotomy cut is warranted. While it may seem intuitive to perform a Reverdin-type wedge within the distal metatarsal head to realign the cartilage, this may not be prudent when there is significant sclerosis or avascular changes. There are some that would suggest attempting a hallucal osteotomy, such as a proximal Akin, in this case to attempt to realign the pull of the long flexor and extensor tendons to create a more effective muscle tendon function across the MTPJ. This realignment of the hallux will reduce the angular retrograde pull of these extrinsic tendons that aggravates recurrence of the HAV deformity. The Akin osteotomy cannot be expected to reduce an elevated PASA or reduce an increased first-second IMA.
If the recurrent HAV deformity is the result of subsidence of bone, then grafting may be required to repair the osteotomy defect. When this is the case, supplemental bone graft materials can be interposed in small amounts preventing excessive impaction of the part. Removing excess bone from the medial metatarsal head, milling it, and replacing it within regions of bone subsidence may prove sufficient. In other cases in which larger defects are evident, bone graft morsels of autogenous or allogenic material may be used to fill defects of the metatarsal shaft when revision of an osteotomy is an appropriate procedure. It is understood that autogenous graft materials provide a more physiologic environment since it is enhanced with osteoinductive and osteoconductive agents such as bone morphogenic protein and growth factors from host thrombocytes. Others have demonstrated that allogenic bone graft material can be used in these small areas of bone deficit with good outcome. Regardless of the source of the graft material, ultimately, it is the position and stability of the fixation that will bring the construct to final union.
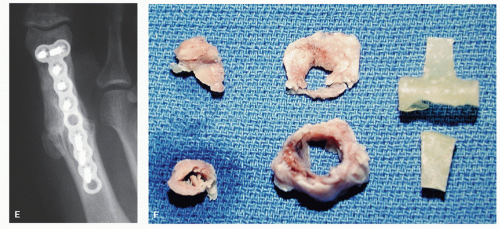
When grafting is required simply to pack voids, the fixation technique can be as simple as a crossing K-wire technique in which the goal is to achieve a stable construct for propulsion whether that is from primary bone healing or the development of a fibrous union (Fig. 36.16). This supplemental bone grafting is a distinctly different procedure than the interpositional bone graft technique used to restore length to the first ray. Generally, bone grafting to simply fill voids after failed DMO or silicone implant will require two points of fixation and protected weight-bearing to achieve union. The interpositional bone graft procedure requires more technical considerations regarding the type of grafts used and the methods of fixation for them. This grafting procedure requires the use of low-profile plates and screws and the need for absolute non-weight-bearing to achieve union. When using this technique, there is an increased risk of complication since two discrete areas will have the potential for developing a nonunion (Fig. 36.17).
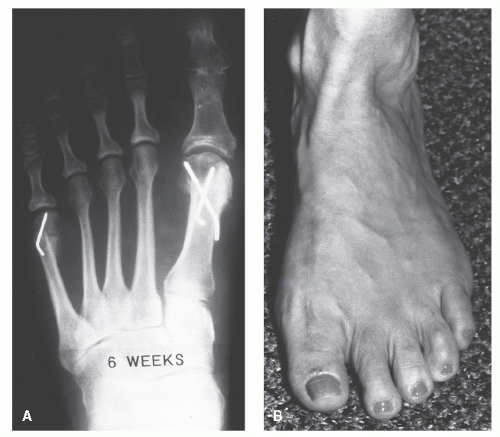 Figure 36.16 A: Radiograph 6 weeks postoperatively. B: Clinical appearance 4 months postoperatively. |
PROXIMAL METATARSAL OSTEOTOMY
When the quality of bone residual from DMO is suspect, a more proximal procedure may be required for revision. In such instances, a CBWO can be performed to achieve multiplanar correction while sparing the length pattern of the first ray. This technique mandates strict attention in preparing the osteotomy axis guide to ensure optimal correction of the deformity while preventing the ill effects of a misaligned osteotomy. While this procedure is straightforward in its essence, the literature reflects that complications often arise when the standard technique is poorly understood and executed. The oblique base wedge osteotomy is an inherently unstable configuration and so requires rigid internal fixation in concert with a course of non-weight-bearing to achieve primary bone healing in the intended position. Should the fixation of a base wedge procedure fail, untoward outcomes such as first ray elevation and shortening of the metatarsal are predictable (37).
Other proximal metatarsal shaft procedures are further options; however, from the standpoint of bone healing, procedures performed on diaphyseal bone require heartier internal fixation and are naturally more challenging in regard to achieving bone healing as compared with procedures performed within metaphysis. In the right hands, a CBWO can provide significant derotation of the first metatarsal and requires the benefit of relatively simplistic internal fixation techniques. Close scrutiny of articular cartilage alignment is needed to determine if an adjunctive procedure is needed to achieve total joint congruity. Cartilage realignment procedures such as the Reverdin, a closing wedge performed in the distal aspect of the metatarsal head, can accomplish this task adding a modicum of time and additional fixation to the procedure (see Fig. 36.8).
Technique
The skin incision is place about the dorsomedial aspect of the first MCJ. If there is a need for concomitant first intermetatarsal space dissection, as is often the case, this incision will extend distally across the first MTPJ. Proximally, the subcutaneous dissection will reveal the dorsomedial cutaneous nerve as it crosses the base of the first metatarsal. The subcutaneous layer and superficial neurovascular structures should be gently retracted to reveal the deep fascial layer including the EHL tendon and the proximal aspect of the first MCJ. The soft tissue balancing procedure of the first intermetatarsal space is performed as described earlier in this text.
The deep fascia is incised in a single layer beginning 1 cm proximal to the first MCJ and extending distally along the medial aspect of the EHL tendon just past the first MTPJ. This will provide exposure for the lateral interspace release as well as the proximal osteotomy. With the periosteum exposed, the incision plan for the osteotomy can be prepared. The configuration of the periosteal incision will vary depending on the shape of the intended osteotomy; usually a short or long oblique orientation is used. The long oblique osteotomy has the benefit of facilitating two points of fixation, and its longer radius arm allows greater lateral rotation as the wedge is closed. Before preparing the osteotomy, it is prudent to place an 18-gauge needle in the first MCJ to serve as a landmark for the articular surface of the first metatarsal base. This will help prevent inadvertent violation of the joint. Here the periosteal incision begins approximately 1 cm distal to the proximal medial corner of the first metatarsal base. This placement preserves the periosteum about the proximal medial border of the metatarsal base and will serve to support the lateral hinge of the osteotomy. The periosteal incision is made at a 40-degree angle to the shaft of the metatarsal, and when the lateral border of the metatarsal is
encountered, the incision is directed along this border to facilitate wide exposure of the metatarsal. A freer elevator is used to reflect the periosteum, and the metatarsal is prepared for osteotomy. A 0.062-inch K-wire is run oriented from dorsal to plantar through the medial base of the metatarsal, 1 cm distal to the MCJ. This K-wire is oriented perpendicular to the weightbearing surface to serve as an axis guide for the osteotomy. This orientation will allow transverse plane translocation of the segment without untoward deviation in the frontal or sagittal plane (see the Chapter on Closing Base Wedge Osteotomy). A skin marker can be used to design and preview the length and width of the intended osteotomy. An osteotome or saw blade can be used to score the dorsal cortex of the metatarsal and create a 40- to 45-degree angle for the proximal cut of the osteotomy. The angulation of the distal cut will depend on the degree of correction required (see the Chapter on Closing Base Wedge Osteotomy). An oscillating saw can be used to begin the osteotomy at the lateral most cortex and should propagate toward the K-wire maintaining the blade parallel to the pin throughout the procedure. It is best to create a smaller wedge and later gently plane the osteotomy than to cut an excessively large wedge and be unable to close the osteotomy without fracturing the hinge. Constant irrigation while performing the osteotomy will reduce the risk of thermal necrosis of bone and will provide optimal physiology for bone healing. Once satisfied with the wedge resection, the bone wedge is inspected along with the deepest region of the osteotomy cut to ensure that the wedge was removed in its entirety. Any inadvertent bone remnant will impede closure of the wedge and create a stress riser about the hinge when attempting to close the wedge. The bone clamp is used to maintain closure of the wedge while intraoperative radiographs are taken to ensure adequate reduction of the deformity. Two points of fixation are employed: an anchor screw and a compression screw. Precise placement of the screws is important to prevent collision of the devices. When viewing the lateral base of the metatarsal in the sagittal plane, the area can be divided into four quadrants. By placing the anchor screw in the dorsal and proximal quadrant and placing the compression screw in the plantar and distal quadrant, collision of the screws is unlikely. The most proximal screw is run transversely through the base of the first metatarsal bone and serves as the anchor screw, protecting against telescoping and shortening of bone and fracture of the medial hinge. This anchor screw is tightened to two-finger tightness as overtightening prior to application of the second screw will prompt a distal shift of the medial fragment and fracture the hinge. Prior to inserting the second screw, the bone clamp is released. The second (distal) screw is oriented as close to perpendicular to the osteotomy as possible.
encountered, the incision is directed along this border to facilitate wide exposure of the metatarsal. A freer elevator is used to reflect the periosteum, and the metatarsal is prepared for osteotomy. A 0.062-inch K-wire is run oriented from dorsal to plantar through the medial base of the metatarsal, 1 cm distal to the MCJ. This K-wire is oriented perpendicular to the weightbearing surface to serve as an axis guide for the osteotomy. This orientation will allow transverse plane translocation of the segment without untoward deviation in the frontal or sagittal plane (see the Chapter on Closing Base Wedge Osteotomy). A skin marker can be used to design and preview the length and width of the intended osteotomy. An osteotome or saw blade can be used to score the dorsal cortex of the metatarsal and create a 40- to 45-degree angle for the proximal cut of the osteotomy. The angulation of the distal cut will depend on the degree of correction required (see the Chapter on Closing Base Wedge Osteotomy). An oscillating saw can be used to begin the osteotomy at the lateral most cortex and should propagate toward the K-wire maintaining the blade parallel to the pin throughout the procedure. It is best to create a smaller wedge and later gently plane the osteotomy than to cut an excessively large wedge and be unable to close the osteotomy without fracturing the hinge. Constant irrigation while performing the osteotomy will reduce the risk of thermal necrosis of bone and will provide optimal physiology for bone healing. Once satisfied with the wedge resection, the bone wedge is inspected along with the deepest region of the osteotomy cut to ensure that the wedge was removed in its entirety. Any inadvertent bone remnant will impede closure of the wedge and create a stress riser about the hinge when attempting to close the wedge. The bone clamp is used to maintain closure of the wedge while intraoperative radiographs are taken to ensure adequate reduction of the deformity. Two points of fixation are employed: an anchor screw and a compression screw. Precise placement of the screws is important to prevent collision of the devices. When viewing the lateral base of the metatarsal in the sagittal plane, the area can be divided into four quadrants. By placing the anchor screw in the dorsal and proximal quadrant and placing the compression screw in the plantar and distal quadrant, collision of the screws is unlikely. The most proximal screw is run transversely through the base of the first metatarsal bone and serves as the anchor screw, protecting against telescoping and shortening of bone and fracture of the medial hinge. This anchor screw is tightened to two-finger tightness as overtightening prior to application of the second screw will prompt a distal shift of the medial fragment and fracture the hinge. Prior to inserting the second screw, the bone clamp is released. The second (distal) screw is oriented as close to perpendicular to the osteotomy as possible.
Final radiographs or fluoroscopy is obtained to ensure adequate position and alignment of bone and fixation devices. The range of motion about the first MTPJ is reassessed, and joint congruence is confirmed. Copious irrigation is then completed, and a layered closure is performed with the benefit of 3-0 absorbable suture running from proximal to distal to reapproximate the periosteum and capsule in an interlocking running fashion to completely cover the fixation devices. The subcutaneous structures are closed with the benefit of 4-0 absorbable suture in a simple running fashion, and the dermal edges are reapproximated with the benefit of 5-0 absorbable suture in a subcuticular running fashion. A Jones compression dressing with a fiberglass egg shell or posterior splint is maintained for the first 5 to 7 days. Absolute non-weight-bearing is integral to success as early weight-bearing will deform if not fracture the proximal metatarsal segment. The duration of non-weight-bearing will vary based upon the quality of the bone stock and evidence of radiographic bone consolidation confirmed in multiple views. It is difficult to assess the degree of bone consolidation of the proximal metatarsal from a clinical perspective, and no physical exam for this has ever been described. After 6 weeks of non-weight-bearing with satisfactory radiographic evidence of bone consolidation, the patient is allowed to return to protected weight-bearing in a firmsoled shoe and is advanced as tolerated thereafter. Serial radiographs are taken in 2- to 3-week intervals for the first 2 months and monthly thereafter until full functional recovery has been achieved. More frequent radiographs are taken when symptoms or clinical change dictates further examination.
Pearls/Pitfalls
The technical consideration regarding proper placement of the hinge axis concept and placement of the axis guide for the CBWO is discussed in detail in an alternate section of this text.
It is prudent to place an 18-gauge needle in the first MCJ to serve as a landmark for the articular surface of the first metatarsal base in an attempt to prevent inadvertent violation of the joint. To further protect the articular surface, the periosteal incision begins approximately 1 cm distal to the proximal medial corner of the first metatarsal base. This placement preserves the periosteum about the proximal medial border of the metatarsal base and will serve to support the lateral hinge of the osteotomy.
Precise placement of the screws is important to prevent collision of fixation devices. When viewing the lateral base of the metatarsal in the sagittal plane, the area can be divided into four quadrants. By placing the anchor screw in the dorsal and proximal quadrant and placing the compression screw in the plantar and distal quadrant, collision of the screws is unlikely.
ARTHRODESIS IN FAILED HALLUX ABDUCTO VALGUS SURGERY
Clinical Considerations
When the first MTPJ is placed in the corrected position and there is a considerable loss of first MTJ motion, a joint preservation procedure may not be feasible. In the face of irreducible MTPJ incongruity or instability of the first MTPJ, an arthrodesis may provide the most predictable and arguably the most definitive correction of the deformity, especially in patients with higher functional demands. Over time, numerous modifications in performing arthrodesis of the first MTPJ have been described (39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54 and 55). The first MTPJ fusion, traditional or modified techniques, can correct transverse plane deformity while simultaneously achieving optimal sagittal plane joint position for propulsion when properly executed. This will stabilize the distal aspect of the first ray and with optimal positioning will improve weight-bearing function of the first MTPJ.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree