Fig. 51.1
A 52-year-old woman was treated with two-stage revision TKR for management of a chronically infected primary TKR. The patient developed severe end stem tibial pain. A prior tibial tubercle osteotomy had been performed, and the tibial hardware was removed (with the exception of a small posterior wire fragment) which did not improve the symptoms of end stem pain. (a) AP and (b) lateral radiographs show the long stem tibial component in which the distal stem is uncemented. (c) AP and (d) lateral radiographs show that the tibial component was revised to a short metaphyseal fully cemented stem with a proximal cementless trabecular metal cone, which resulted in complete resolution of end stem pain
51.2 Tibiofemoral Dissociation
The tibial insert of a modular tibial component is attached to the tibial baseplate with a mechanical locking mechanism. A number of different locking mechanisms have been used successfully in TKR including those with peripheral and/or centrally located mechanisms which capture the tibial insert.
Early postoperative tibial insert dissociation usually results from incomplete seating of the insert into the tibial baseplate. Cement or debris may prevent incomplete insert seating.
Dissociation of the tibial insert from the tibial baseplate usually results after TKR if the insert is incompletely seated at the initial surgery [11, 13]. Cement or soft tissue which becomes interposed between the insert and baseplate can prevent full seating of the insert and result in dissociation. This may be more of a risk with minimally invasive surgery in which visualization of the baseplate locking mechanism is more limited [11]. Displacement forces on the tibial insert are generally directed anteriorly, but can occur posteriorly [4, 17]. Dissociation of the insert is apparent on a lateral radiograph. Treatment should consist of revision to carefully inspect the integrity of the baseplate locking mechanism and revision of the insert provided the locking mechanism is intact.
Late dissociation can result from ultra-high-molecular-weight-polyethylene (UHMWPE) locking mechanism mechanical failure particularly with more constrained implants, or hinge devices with severe soft tissue laxity.
Insert dissociation can also result from mechanical failure of the UHMWPE insert at the insert locking mechanism [17]. This mode of failure has occurred more frequently in modular acetabular total hip components, including those made of highly cross-linked UHMWPE [7]. Constrained components which are used to treat ligament insufficiency have higher stresses on the locking mechanism than unconstrained components with intact ligaments. Constrained inserts which rely on a central screw to secure the insert to baseplate may dissociate if failure of the screw fixation occurs [4, 16]. Fully constrained rotating hinge mechanisms can also dissociate if sufficient soft tissue laxity is present to allow the rotating hinge stem to be completely distracted from the tibial component (Fig. 51.2).


Fig. 51.2
A 58-year-old woman with 2 failed two-stage treatments for MRSA-infected TKR with extensor mechanism disruption who adamantly refused amputation was treated with a third two-stage revision surgery using a rotating hinge segmental distal femoral replacement and medial gastrocnemius muscle flap transposition to the extensor mechanism. (a) AP and (b) lateral radiographs illustrate the segmental distal and proximal tibial replacement which had been used with uncemented press fit femoral and tibial stems. The treatment was successful in controlling infection, but proximal subsidence of the uncemented femoral component occurred resulting in soft tissue laxity and dissociation of the tibial component shown on (c) AP and (d) lateral radiographs. This was successfully treated with femoral component revision to a cemented stemmed distal femoral replacement shown in (e) AP and (f) lateral radiographs which restored leg length and soft tissue stability
51.3 Periprosthetic Fracture Around a Well-Fixed Long Stem TKR
Femoral fracture at the tip of a revision TKR femoral or tibial component diaphyseal stem can be a difficult problem to manage. Treatment options include revision to a longer stemmed component and/or cable plating or strut allografting (Fig. 51.3).


Fig. 51.3
(a) An AP radiograph illustrates a well-fixed hinge distal femoral replacement which had been used to treat a distal femoral tumor. (b) 10 years after surgery the patient fell and sustained a periprosthetic fracture around the proximal femoral stem tip. (c) Treatment consisted of femoral revision to a longer uncemented stem and cable plating
Periprosthetic fracture patterns after revision TKR can differ from periprosthetic fractures after primary TKR since the fractures typically occur around a stemmed component. Treatment may require long stem revision, plating, or both.
Periprosthetic fracture may occur from minor trauma if a stress riser is present at or near the stem tip. This may result from perforations in the cortex from prior hardware or reaming the intramedullary (IM) canal (Fig. 51.4). A stress riser also occurs if the proximal femoral stem tip is in proximity to the distal stem tip of a THR. Depending on the stem lengths, there may be a short distance between the two stems which results in an area between the stems at risk of fracture. Fracture between the distal tip of a THR stem and proximal tip of a TKR stem can be associated with considerable morbidity [10]. Treatment with plating allows retention of both the THR and TKR. However, if nonunion develops, then revision to a total femur is likely to be required. Patients with osteopenic bone, poor balance or cognitive dysfunction, and IM femoral THR and TKR stems in proximity to one another would be expected to have a risk of falling and developing a periprosthetic fracture between the two stems. Patients at risk of interprosthetic femoral fracture between THR and TKR stems may benefit from prophylactic femoral plating at the time of revision TKR (Fig. 51.5).


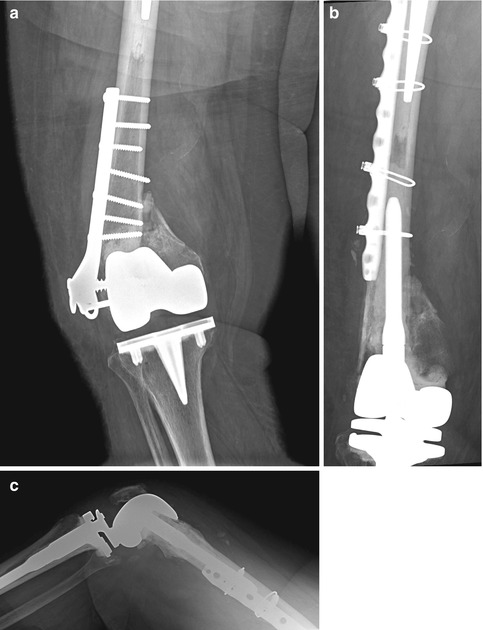


Fig. 51.4
(a) A lateral radiograph shows retained screw fragments from prior open reduction and internal fixation (ORIF) adjacent to the proximal end of a well-fixed femoral TKR stem in a 72-year-old woman. (b) The patient fell and sustained a periprosthetic fracture through the stress risers from prior screw hardware. (c) The fracture was stabilized with a lateral cable plate. (d) Nonunion and failure of fixation then developed. (e) Revision to a segmental distal femoral replacement with porous coated proximal stem was performed which resulted in effective restoration of knee function
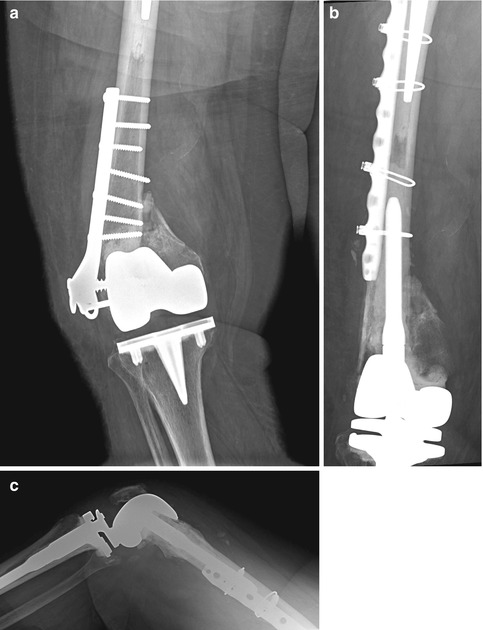
Fig. 51.5
A 79-year-old woman who had undergone prior right TKR as well as cemented bipolar hemiarthroplasty for right hip fracture sustained a supracondylar periprosthetic fracture. The fracture was treated with plating which failed. The patient presented with a supracondylar nonunion (a) and had been unable to ambulate for the past 18 months. The plate and TKR were revised to a cemented distal femoral replacement (b, c). Since the area between the hip and knee stems was considered to be a potential stress riser which could risk later periprosthetic fracture between the two stems, a prophylactic lateral cable plate was placed at the time of revision TKR
51.4 Arthrofibrosis with Patella Baja
Patella infera can occur from contracture of the patellar ligament following trauma or surgery and may develop in association with arthrofibrosis [14]. Arthrofibrosis can develop from a number of causes and results in formation of dense intra-articular scar formation [19, 21]. The combination of patella baja and arthrofibrosis is difficult to treat since patellar ligament contracture shortens the extensor mechanism contributing to limited knee flexion.
Revision TKR for arthrofibrosis can often result in the development of recurrent stiffness and patella baja. Femoral revision with distal augments to lower the joint line can improve the position of the patella relative to the femoral component, but this may also create flexion-extension imbalance requiring a constrained implant.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








