Fig. 6.1.
(a) Long-standing radiograph of bilateral knee osteoarthritis. (b) Preoperative lateral radiograph of right knee with distal femoral malunion.
The patient was born with a large cavernous hemangioma of the right lower extremity involving the entirety of the thigh, lateral and anterior aspect of the knee and extending to the proximal tibia. She had previous treatment with radiation therapy and seven surgical procedures including a cross-leg flap from the posterior calf of the left leg to provide skin coverage over the anterior right knee. This resulted in a large, bulbous flap approximately 15 cm in diameter (Fig. 6.2). As a result of her radiation therapy, extensive dense scar extended from the lateral hip down to the lateral calf. At the level of the knee, this scar tissue was primarily posterolaterally located and was associated with a 20° hard flexion contracture of the knee (Fig. 6.2b). In the distribution of this scar tissue, the patient had developed severe hypersensitivity that had been diagnosed as complex regional pain syndrome (CRPS).


Fig. 6.2.
(a, b) Photographs of lateral and posterolateral external scarring and prior cross-leg flap to anterior right knee.
Other than her musculoskeletal issues, the patient was healthy and had a BMI of 28. She had neutral alignment of the right knee and a 20° flexion contracture (ROM from 20 to 50°). There was no opening laterally with varus stress as the knee had developed a severe posterolateral based external scar contracture. There was an intact extensor mechanism and she had intact sensation and palpable pulses in the right foot.
6.2 Diagnosis/Evaluation
Initially, we discussed with this patient the surgical options of above knee amputation, fusion, and arthroplasty. We had the patient meet with several local amputation patients, with prosthetists, and with our orthopedic oncology partners for a second opinion. We met with the patient several times over a 7-month period while she was investigating her surgical options. We counseled her that there was considerable risk of worsening her pre-existing complex regional pain syndrome and that flap and skin necrosis may occur. We discussed with her that if her soft tissue necrosis did occur, this may lead to the need for free flap coverage or even above knee amputation if she were to develop periprosthetic joint infection. After extensive informed consent, the patient elected to proceed with total knee arthroplasty with the soft tissue management plan of a midline incision through her existing cross-leg flap.
A preoperative consultation with a plastic surgeon was obtained to evaluate the tissues about the knee and vascular surgeons to evaluate the status of the large hemangiomas in the right lower extremity. An MRI was performed showing diffuse venous vascular malformation extending from the right hemipelvis to below the knee. There were extensive hemangiomas in the anterior and posterior right thigh compartments and very mild osseous involvement in the mid femoral shaft (Fig. 6.3). Intra-articularly, there was only suprapatellar pouch involvement with minimal involvement of the lateral knee or articular surfaces.
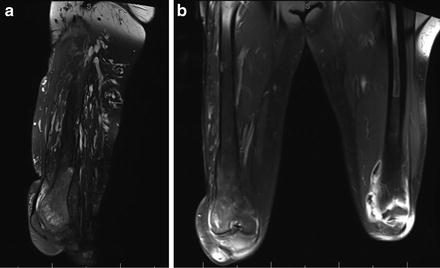
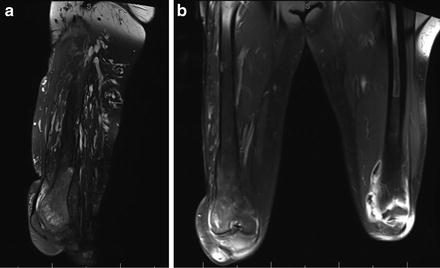
Fig. 6.3.
Sagittal (a) and coronal (b) MRI imaging of vascular malformations of right thigh and periarticular region.
The preoperative evaluation with the vascular surgeons revealed that since the majority of the vascular malformations were in the posterior thigh and did not involve the articular surfaces of the knee, that total knee arthroplasty would be reasonable. The plastic surgeons advised that with a cross-leg flap there was no specific pedicle to preserve and thus recommended a longitudinal full thickness incision through the midline of this flap with elevation of full thickness subfascial flaps medial and lateral. We discussed lifting the flap from the lateral most aspect to follow the general principle of using prior lateral based incisions. However, as this knee had undergone prior skin grafting and irradiation, there was abundant scar along the interface between the flap and lateral skin. Additionally we were concerned that if we had to elevate the entire flap from the lateral side that we may disturb the blood supply to the majority of the flap and lose our coverage over the entire anterior knee.
6.3 Management and Treatment Options of Complex Skin Issues
Preoperative evaluation of the TKA patient should always involve a close examination of the soft tissues. The presence of prior incisions or scarring should prompt a discussion of prior surgical interventions or trauma and when they occurred. It is often felt that old incisions can be ignored in the setting of TKA; however, if any prior longitudinal incision is ignored, the consequences can be devastating as seen in the clinical photos in Fig. 6.4 of a patient 6 weeks after a new medial incision was made in the setting of an ignored 20 years old lateral based incision. The majority of blood supply to the anterior skin around the knee comes from terminal branches of a peripatellar anastomotic ring of arteries in the subcutaneous fascia, most of which enters from the medial side. Therefore, flap formation over the anterior knee should be performed deep to the subcutaneous fascia to avoid disrupting this blood supply. If multiple prior longitudinal incisions exist, the lateral most incision should be utilized whenever possible so as to minimize the size of vulnerable lateral flap. If prior oblique, or transverse incisions exist, these can most safely be approached at 90° angles to limit the risk of necrosis in the corners where these incisions meet. In general, angles of less than 60° between a prior oblique incision and the new proposed incision should be avoided.
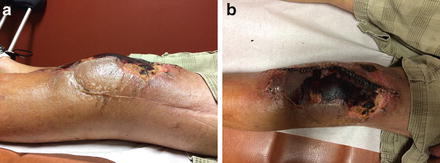
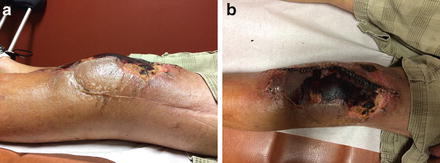
Fig. 6.4.
(a, b) Photographs of knee with skin necrosis after midline incision made adjacent to prior lateral incision.
When performing incisions on knees with prior flaps, the source of blood supply needs to be considered. Preoperatively, the type of prior flaps and their potential pedicles should be investigated through discussion with plastic surgeons, reading prior operative reports, and possible advanced imaging to assess blood supply to the flap.
Soft tissue expanders may be indicated if periarticular skin is compromised by multiple prior crossing incisions, flaps, or severe deformity preventing skin mobilization and coverage after the reconstruction is performed. Expanders are generally utilized for a period of 8–10 weeks with injection of saline into a subdermal port and have yielded favorable long-term results [1]. Typically, patients with prior skin graft, irradiated tissue, or densely adherent scar tissue are contraindicated for soft tissue expansion and may require flap coverage prior to their arthroplasty procedure. In our case, our patient did have a prior flap and we considered using a soft tissue expander preoperatively, but due to the fact that she also had some areas of skin grafting, irradiated tissues, and adherent scar tissue, we elected to avoid expansion.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








