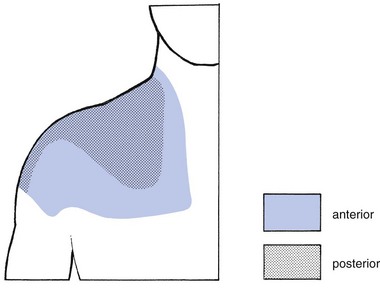
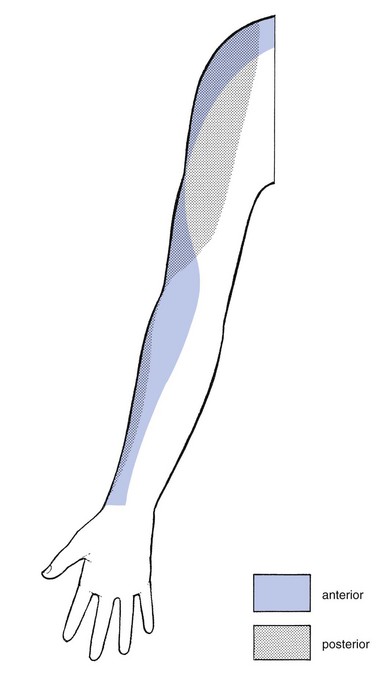
12 Pain in the shoulder is, after low back pain, the most frequent complaint of orthopaedic patients. Despite the frequency of shoulder lesions – and the consequent pain and disability – much confusion still exists as to aetiology, terminology and treatment,1 in contrast to the statement made by Cyriax:2,3 On other occasions, patients present with a painful limitation of passive movement together with pain on resisted movements, and the question arises as to whether the problem is in an inert or a contractile structure. If there is capsular limitation on examination, the joint should be treated first. If resisted movements remain painful after the joint has been managed appropriately, then the tendons should be treated. This approach is the best one, because resisted movements very often become negative after arthritis has disappeared. The only explanation for the phenomenon is the close relationship between the capsule of the shoulder and the surrounding tendons.4 It can easily be understood how tension on the contractile structures may influence the pain originating in arthritis. Therefore pain on resisted movement(s) in association with an articular pattern should not be interpreted as being caused by a simple tendinosis. Of course, a severe tendinosis can limit active movement, because of the pain. But passive movements are of full range with a normal end-feel, even though there might be severe pain at the end of movement. An arthritis is an arthritis, a tendinosis is a tendinosis and both have to be treated as such. It is a common misbelief that, as long as steroid is injected somewhere in the shoulder area, it will spread and cure the lesion, no matter where the lesion lies or where it was injected.5 In fact, if there is one region in the body which ought to be diagnosed and treated very specifically it is the shoulder. It is necessary to replace a vague diagnosis such as ‘rotator cuff disease’ or frozen shoulder by a precise one indicating exactly what is wrong.6–8 Other possible causes of referred pain at the shoulder are visceral disorders. The diaphragm is largely developed from the third and fourth cervical segment, the heart from the eighth cervical to the fourth thoracic. Therefore both can give rise to pain in the shoulder and arm. Irritation of the diaphragm and of the phrenic nerve, for example by blood or air under the diaphragm, is another well-known source of acute shoulder pain.9,10 A pulmonary neoplasm at the base of the lung with involvement of the diaphragm can provoke pain in the shoulder area. The same may also happen with a tumour of the superior sulcus (Pancoast’s tumour). The majority of these patients complain of shoulder pain and are often mistakenly thought to be suffering from a musculoskeletal lesion.11,12 Most structures around the shoulder are derived from the C5 segment. There is one important exception: the acromioclavicular joint, which is of C4 origin (Fig. 12.1). In acromioclavicular joint problems the pain is felt at the tip of the shoulder, with little spread. Exceptionally, when the lesion lies at the inferior acromioclavicular ligament, the pain can spread into the upper arm. In a lesion of one of the other shoulder structures, such as in all types of tendinosis, arthritis and subdeltoid bursitis, the pain is not so much felt at the tip of the shoulder but rather starts in the deltoid region and may spread further down the radial aspect of the arm to the base of the thumb (C5 dermatome; Fig. 12.2). How far down the arm the pain is referred depends on the severity of the lesion: the more severe the inflammation, the further the pain will spread. In glenohumeral arthritis, the degree of pain reference is of particular interest in following the healing process: as the patient improves, the inflammation decreases and the pain spreads less far. In arthritis of the shoulder, the history will be important to establish the stage (see Ch. 13). In other disorders it is of less significance. The answers to a number of questions (summarized in Box 12.1) will be needed. • What is your age? Age can be relevant in several disorders. It can be helpful in defining the exact type of arthritis. Traumatic arthritis will only be met after 40 years of age, arthritis from immobilization after the age of 60. Subdeltoid bursitis might be present between 15 and 65 years of age. Tendinosis can occur at any adult age. • What is the pain and does it radiate? Pain starting in the deltoid area and spreading towards the wrist, along the radial aspect of the arm, is caused by a lesion that originates in C5. Such pain may be felt in the whole dermatome or only in part of it. The majority of the shoulder structures belong to the C5 segment. The acromioclavicular joint, a C4 structure, is the main exception. A patient who indicates the tip of the shoulder only as the site of pain suggests strongly that there is a lesion of the acromioclavicular joint. Whether the pain is caused by arthritis, bursitis or simple tendinosis will make no difference to where or how far distally the pain is felt. The distal spread of referred pain depends only on the degree of inflammation. It is routine to ask if the pain remains above the elbow or radiates below it – a matter of particular importance in arthritis. • Is there any pain in the arm at rest? This gives information about the severity of the lesion: if spontaneous pain is present, there is a greater degree of inflammation than if pain is felt only on movement. Again, the answer to this question is one of the criteria for judging the stage of arthritis. • Can you lie on the affected side at night? Pain when lying on the shoulder indicates more severe inflammation than just pain on exercise. Bursitis, tendinosis or arthritis may make it impossible for the patient to lie on the affected side at night. Consequently, this question is not of much help in defining the exact nature of the structure at fault. However, it is rather important in following the resolution of the disorder: as the condition improves, the pain at night diminishes and finally disappears. • Did the pain come on spontaneously or was there any particular reason for it, such as overactivity or an injury? It is clear that overactivity may provoke tendinosis. In a ruptured tendon, however, one should not necessarily expect recent overuse. Overactivity can also cause arthritis in a joint that is already osteoarthrotic; this is just as true for the acromioclavicular joint as it is for the glenohumeral joint. In haemophilia, haemarthrosis usually comes on spontaneously; it is more common at the knee but may occur at the shoulder as well. • For how long have you had the pain? If the pain has already been present for some months, an acute subdeltoid bursitis can be excluded because the full course of this condition is 6 weeks. In addition, onset is abrupt over a few days, sometimes only hours, as in an attack of gouty arthritis. Arm pain because of root compression by a cervical disc protrusion wears off in about 4 months. Long-standing pain can be the outcome of a chronic subdeltoid bursitis or a simple tendinosis. Both can last for years. Monoarticular steroid-sensitive arthritis can take up to 2 years to disappear spontaneously. • Are any other joints affected? A more generalized inflammatory disorder is expected if other joints have been previously involved or are attacked at the same time. Indeed, the shoulder joint can be the seat of rheumatoid arthritis, lupus erythematosus and ankylosing spondylitis. • How is your general condition? Have you had any operations? Recent unexplained loss of weight can be the first sign of a carcinoma. A primary tumour at the shoulder or metastases can be a local source of shoulder pain. A Pancoast’s tumour of the lung often provokes pain in the shoulder area. The inspection starts with checking what position the head is held in and whether both shoulders are level. It is important to check for redness, swelling, muscular wasting or any deformity such as scapular winging. A step deformity at the upper lateral aspect of the shoulder is caused by an acromioclavicular dislocation, with the distal end of the clavicle lying superior to the acromion. Atrophy of the upper trapezius may indicate spinal accessory nerve palsy.13 Atrophy of supraspinatus and/or infraspinatus is caused by either a supraspinous nerve palsy or long-standing rotator cuff lesions.14 Effusion of more than 10–15 mL arising from the glenohumeral joint is normally visible on inspection at the anterior centre of the humeral head. Local swelling may also be found in acute, haemorrhagic or chronic subdeltoid bursitis and in acromioclavicular joint cysts,15 as well as in tumours. The shoulder is an easy joint to examine. The intention is to obtain the maximum information from a minimum number of tests. Recent studies have shown high inter-rater and intra-rater reliability of the examination scheme presented.16–18 • There is or was trapezius pain • The pain is only at the top of the shoulder and/or at the clavipectoral area • The pain is in the arm but remains quite localized • The pain in the arm is influenced by movements of the neck • Coughing, sneezing or taking a deep breath increases the pain The preliminary examination of the upper quadrant is comprised of the following tests (Box 12.2): 1. Six active movements of the cervical spine – range of movement and/or painfulness; quick survey of the cervical spine 2. Active elevation of the shoulder girdle – range of movement and/or painfulness; quick survey of all the structures of the shoulder girdle 3. Resisted rotations of the cervical spine and resisted elevation of the scapulae; quick survey of nerve roots C1–C2–C3–C4 4. Active elevation of both arms – range and pain; quick survey of shoulder and shoulder girdle 5. Resisted movements of the upper limb – strength and pain; this is both a quick test for peripheral lesions at the elbow–arm–wrist and a neurological examination of roots C5–C6–C7–C8–T1 and of the peripheral nerves of the upper limb 6. Passive examination of the elbow; quick test of the elbow joint.
Clinical examination of the shoulder
Referred pain
Pain referred to the shoulder
Pain referred from the shoulder
History
Inspection
Functional examination
Preliminary examination
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Clinical examination of the shoulder