Fig. 6.1
(a) Medial view of the knee: attachment sites (Redrawn from Bonasia et al. [17]). (b) Medial aspect of the knee showing the MCL (left loop) and the POL (right loop)
6.3 Diagnosis
In the diagnosis of MCL lesions, the authors prefer the Fetto and Marshall classification. This classification divides medial-sided knee injuries into grade 1 (no valgus laxity), grade 2 (valgus laxity at 30° of flexion), and grade 3 (valgus laxity at 0° and 30°) [8]. The stability of the knee is then tested in all planes in order to evaluate anteroposterior, lateral, and rotational instability.
By definition, patients with medial-sided injuries have increased laxity with valgus stress. The examiner applies a valgus stress to the knee at both 0° and 30° of flexion. For isolated sMCL injuries, the greatest joint space opening occurs with the knee in 30° of flexion [9]. Joint space opening with the knee fully extended indicates an injury to the capsule, the POL, or both. Grade III MCL injuries are frequently associated with injury to another ligament (mostly the ACL) [2].
Other physical examination maneuvers combine rotation with various amounts of knee flexion in an attempt to discriminate between MCL and MCL/PMC injuries. One of the most common involves a valgus stress to the knee in 30° of flexion with the foot externally rotated [2]. The presence of anteromedial rotary instability (AMRI) is indicative of PMC injury. AMRI is detected by performing the anterior drawer test with the tibia both in neutral and in external rotation. Increased translation with the tibia in external rotation is indicative of AMRI [10, 11]. Increased external rotation and AMRI indicate injury to the PMC and possibly to the ACL as well.
Weight-bearing radiographs of the knee are obtained in anteroposterior and lateral views. If valgus malalignment is present, a weight-bearing long-leg radiograph is obtained. MRI is helpful in diagnosing associated bone and soft tissue injuries (anterior and posterior cruciate ligaments, posterolateral corner, and menisci) as well as determining the location and extent of medial/posteromedial ligamentous injuries. However, it has been shown that MRI tends to overestimate injury to ligamentous structures [12].
6.4 Indications
In the acute setting (<3 weeks), the treatment of grade I–II injuries is mostly conservative [13, 14], but significant controversies exist regarding the treatment of grade III lesions, both isolated and combined with other ligamentous injuries [15, 16].
On the other hand, in the chronic (>6 weeks) medial/posteromedial instability setting, the conservative treatment option can be excluded. However, controversies exist regarding the most reliable surgical technique. In addition, the limb alignment is a crucial predicting factor and needs to be carefully evaluated. In case of varus or neutral alignment, only soft tissue procedures addressing the medial instability should be performed. In case of severe valgus, a distal femoral varus osteotomy with or without soft tissue procedures should to be considered.
In case of combined PMC and ACL instability, ACL reconstruction is performed and the knee is evaluated intraoperatively for medial laxity. If the knee shows at full extension a medial opening greater than 4 mm compared to the contralateral side, capsular procedures or MCL reconstruction can be considered [17]. This has to be carefully considered while planning the surgery in order to leave adequate graft options for PMC reconstruction after the ACL procedure. In these cases, the authors recommend patellar tendon or allograft ACL reconstruction, in order to preserve the hamstrings for the PMC procedures. Alternatively, allografts can be used for PMC reconstruction.
In case of multiligament knee injuries [18, 19], these are generally treated acutely, but in some cases (i.e., polytrauma), the procedure can be delayed, respecting the damage control principles. In case of chronic multiligament knee injuries in young patients, the authors’ approach is to treat all torn ligaments with allograft reconstruction procedures at the same time. Alternatively, only ACL reconstruction can be delayed.
Many techniques have been described for the treatment of medial and posteromedial ligamentous injuries of the knee, either with allograft or autograft. These can be divided in capsular procedures and reconstruction techniques.
6.5 Capsular Procedures
In these procedures the lax medial/posteromedial structures are re-tensioned but not reconstructed. The surgical approach is as previously described in specific chapters of this volume.
6.5.1 Re-tensioning of the Posteromedial Structures
The goal of this technique is to create increased distance between the origin and insertion of the lax medial/posteromedial structures. This is done by attaching the lax segments of the tendon/ligament to an adjacent intact structure. Therefore, this procedure is indicated when some medial or posteromedial structures are intact. There are no strict rules regarding the re-tension of lax structures, because this depends on the patient’s injury pattern. However, different structures need to be visualized and probed for tension, and these include the sMCL, the posteromedial capsule, the medial meniscus attachments, the POL, and the capsular arm of the semimembranosus tendon.
The sartorius fascia is incised longitudinally and care is taken to avoid injury to the saphenous nerve. The whole MCL is probed (proximal and distal attachments as well as mid-substance). Once the posteromedial capsule is visualized and palpated for laxity, a longitudinal arthrotomy is performed posterior to the MCL. The capsular arm of the semimembranosus is identified and probed for tension. The POL and the meniscotibial attachments are evaluated. Every lax structure is armed and sutured to an intact adjacent ligament/tendon or back to the bone with transosseous sutures. Multiple reinforcing sutures can be placed across the POL and MCL.
6.5.2 En Masse Elevation
This procedure is indicated when a generalized laxity of the medial/posteromedial structures is present. A medial hockey-stick incision is preferred, from the pes anserinus to the posterior portion of the medial femoral epicondyle. The weakest attachment (femoral or tibial) of the medial/posteromedial complex should be identified. The structures at the weakest attachment must be released as an entire tendon/ligament unit (en masse) and not as individual tendons or ligaments, in order to preserve their integrity and vascularity (Fig. 6.2). This unit must be strongly armed with sutures, re-tensioned, and fixed back to the bone. Reattachment to the bone is performed anteriorly and inferiorly if the tibial insertion is lax or posteriorly and superiorly in case of femoral insertion laxity. The bone around the isometric point is “roughed-up” until good bleeding is achieved. Fixation can be achieved with staples or suture anchors [20, 21]. As in the acute MCL repair, care must be taken to preserve the isometricity, mostly when a proximal en masse elevation is performed, in order to reduce the risk of postoperative stiffness.
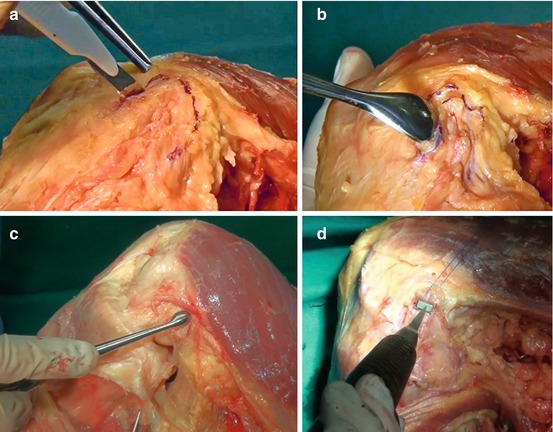
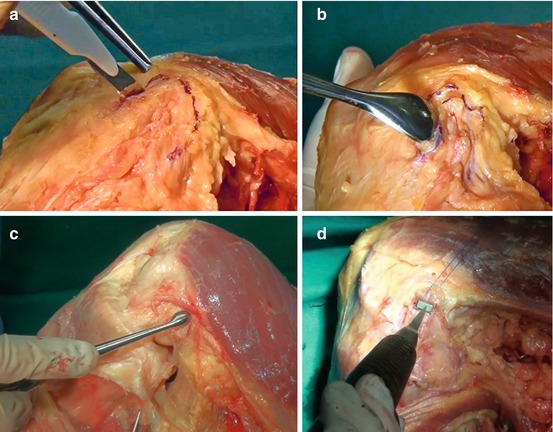
Fig. 6.2
En masse elevation. (a, b) The structures at the weakest attachment (in this specimen, the femoral attachment) are released as an entire tendon/ligament unit (en masse). (c) The bone around the isometric point is “roughed-up” until a good bleeding is achieved. (d) Fixation is achieved with staples or suture anchors
6.6 Reconstruction Techniques
6.6.1 Kim’s Technique
A curvilinear incision is placed from the medial femoral epicondyle to the pes anserinus. The sartorius and gracilis tendons are retracted medially. The semitendinosus is harvested, preserving the tibial attachment. The proximal end of the tendon is armed with a n°2 nonabsorbable suture. A 1.6 mm K wire is placed on the posterosuperior border of the medial femoral epicondyle. The semitendinosus tendon is looped around the wire, and isometricity (<2 mm migration) is tested through a full range of motion. A 6.5 mm cancellous screw and an 18 mm diameter soft tissue washer are placed through a hole. The screw hole is drilled 9 mm (the radius of the washer) proximal to the isometric point. Decortication is performed around the drill hole. After manual tensioning of the graft, the screw is tightened with the knee in 30° of flexion and varus stress (Fig. 6.3). Dissection of the direct head of the semimembranous tendon is performed. The free end of the graft is pulled under the direct head of the semimembranosus tendon and sutured to it at 30° of knee flexion [22].
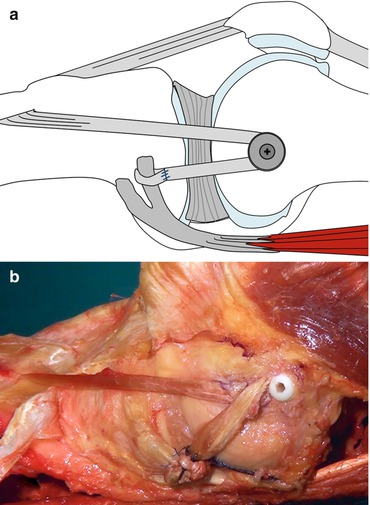
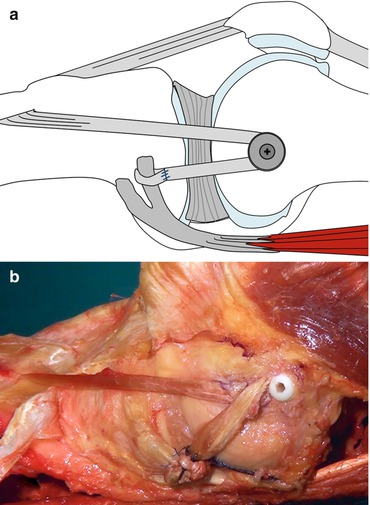
Fig. 6.3
(a) Kim’s technique (see text) (Redrawn from Bonasia et al. [17]). (b) Specimen showing the reconstruction (in this case with an interference screw, instead of screw and washer)
6.6.2 Stannard’s Technique
In Stannard’s modification of Kim’s technique, the free end of the semitendinosus is passed under the direct head of the semimembranosus tendon and sutured to the intact insertion of the semitendinosus itself on the tibia (Fig. 6.4). The graft is tensioned with the knee in approximately 40° of flexion and a slight varus stress [23].
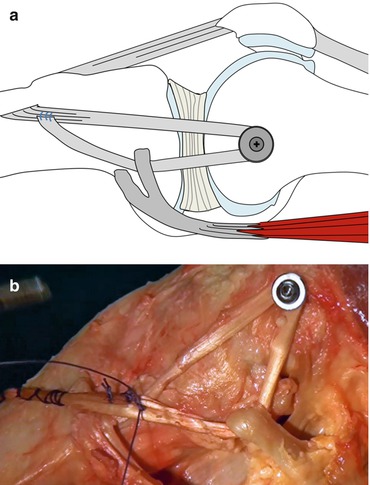
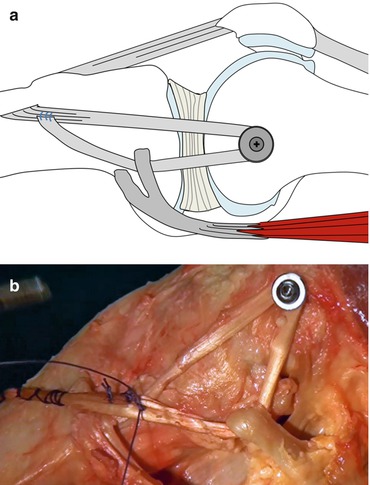
Fig. 6.4
(a) Stannard’s modification of Kim’s technique (see text) (Redrawn from Bonasia et al. [17]). (b) Specimen showing the reconstruction
6.6.3 Lind’s Technique
Incision, semitendinosus harvesting, and isometricity evaluation are as described by Kim. A tunnel of the same size of the double-looped tendon is drilled at the isometric point on the femur. The tendon loop is then armed with a baseball suture, passed into the tunnel, and fixed with an interference screw (same diameter as the tunnel or 1 mm bigger according to the bone quality). This is performed with the knee at 10° of flexion and neutral rotation. A tibial tunnel (same size of the graft) is then drilled to the posterior corner of the medial tibial condyle from anterior to posterior. The drill hole is aimed to exit 10 mm below the tibial plateau, posterior and lateral to the semimembranosus insertion. The free end of the graft is passed through the posterior tibial tunnel opening and fixed here with an interference screw (same diameter as the tunnel) to reconstruct the POL (Fig. 6.5). This is tightened at 60° of flexion and neutral rotation [24].
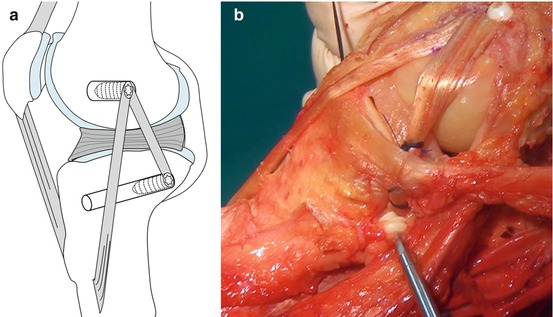
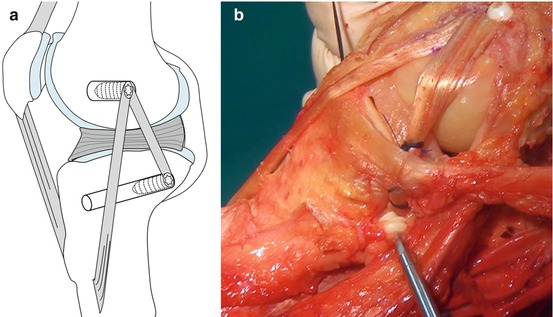
Fig. 6.5
(a) Lind’s technique (see text) (Redrawn from Bonasia et al. [17]). (b) Specimen showing the reconstruction
6.6.4 Coobs et al. Technique
This technique entails a reconstruction of both sMCL and POL, through a single medial incision, with two separate grafts and four different tunnels (Fig. 6.6). Allografts or gracilis and semitendinosus autografts can be used. The anatomy of proximal and distal insertions of both bundles needs to be known (Fig. 6.1). Isometricity is evaluated with K wires for both bundles. Correctly sized tunnels are drilled at the isometric points. The sMCL is tightened at 30° of knee flexion and the POL is tightened at 0°. Fixation is achieved with interference screws [25, 26].
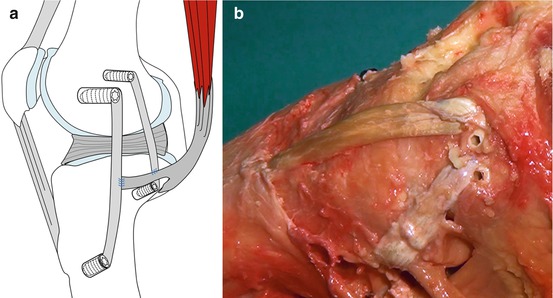
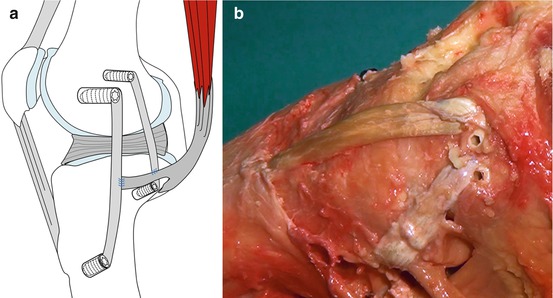
Fig. 6.6




(a) Coobs et al. technique (see text) (Redrawn from Bonasia et al. [17]). (b) Specimen showing the reconstruction
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








