Diagnostic arthroscopy and meniscal and cartilage treatment
Medial skin incision
Graft harvesting
ACL tibial tunnel
PCL femoral tunnel
PCL tibial tunnel
ACL femoral tunnel
Medial reconstruction
Lateral skin incision
Lateral reconstruction
PCL graft is tensioned in full extension and then fixed at 80° flexion
ACL graft is tensioned and fixed in near full extension
Medial and lateral fixation
Skin closure
15.4 Anesthesia
At our center, preoperative nerve (femoral and sciatic) block is the preferred method of pain relief for the first 1 or 2 days after ligament surgery. This procedure is not advocated in the presence of peroneal nerve palsy or disease.
15.5 Graft Selection
Considering the multiple grafts needed for this type of surgery, allografts are a logical and valid option. As allografts have limited availability in our country, we are forced to use autografts in chronic dislocation, even if we have some concern about donor site morbidity when harvesting two or more grafts from the same knee. We usually prefer to harvest the quadriceps tendon-patellar tendon or the bone-patellar tendon-bone from the ipsilateral limb for the PCL reconstruction, the hamstring tendon from the ipsilateral limb for the ACL reconstruction, and the hamstring tendon from the contralateral limb for the medial or lateral reconstruction. These options are interchangeable and largely depend on the anatomic lesions being addressed. When allografts are available, the choice depends largely on the surgeon’s preference; their main advantages are to minimize donor site morbidity in an already severely injured knee and to reduce the duration of the operation [1, 12–15].
15.6 Arthroscopy
For acute or chronic dislocation, the patient is positioned supine on the operating room table in the decubitus position with the knee flexed 70–90° and the foot on the table. A simple lateral post without a circumferential leg holder is preferred to control the surgical leg, as this allows more freedom for knee motion and can easily be removed if necessary. A tourniquet is used during all surgeries and standard arthroscopy is performed to verify all intra-articular lesions. Five portals are routinely used: (1) superolateral approach for the outflow, (2) anterolateral portal located just inferior to the distal pole of the patella, (3) parapatellar anteromedial portal located just medial to the patellar tendon, (4) posteromedial portal located adjacent to the posterior aspect of the medial femoral condyle and 3 cm above the joint line, and (5) the posterolateral portal located along the posterior edge of the lateral femoral condyle and 1 cm above the joint line. The last portal is performed if necessary or if a transeptal approach will be performed. Diagnostic arthroscopy allows not only an assessment of the status of the articular cartilage and menisci, but is mandatory for planning all of the following surgical steps. The instability pattern is reassessed and compared to the preoperative diagnosis. In detail, disruption of the meniscotibial or meniscofemoral ligament would result in visible elevation of the meniscus from its attachment site on the tibia or femur (meniscal rise sign), which is repaired during the open part of the procedure. The presence of capsular scar tissue or redundancy is noticeable. The intercondylar notch is inspected and any scar tissue debrided. Care should be taken to note the attachment sites of the cruciate ligament and to preserve the meniscofemoral ligaments, if present, even though the meniscofemoral ligaments are often torn or absent in chronic dislocation (Fig. 15.1). The popliteus tendon can easily be visualized and its tension and femoral attachment carefully inspected [16]. Any abnormal opening of the medial or lateral compartment greater than 1 cm, as determined by the “gap test” [17], with varus/valgus stress at 30° is indicative of an injury (Grade III) to the collateral ligament on that side [18].
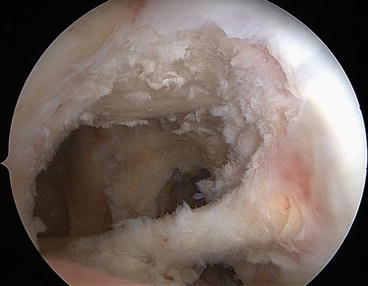
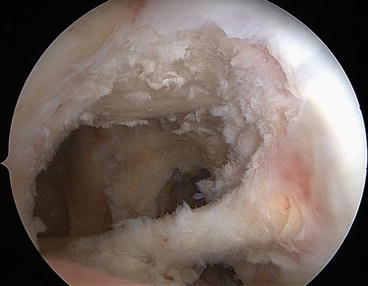
Fig. 15.1
Arthroscopic view of the intercondylar notch, which is “empty” after the removal of scar tissue and preservation of the meniscofemoral ligament
15.7 Skin Incision
The choice of surgical incision is based on the pattern of ligamentous injuries, with the most common injury being to the ACL, PCL, and MCL or LCL. With the knee in 90° flexion, a curved medial skin incision is made beginning midway between the tibial tubercle and the medial collateral ligament and extending proximally over the medial femoral condyle. This approach allows us to harvest the grafts, create tibial tunnels for ACL and PCL and the femoral tunnel for PCL, and perform MCL and POL reconstructions. At the end of the ACL/PCL arthroscopic reconstruction, if necessary, a lateral hockey stick incision can be made parallel to the posterior edge of the ITT. The incision originates distally just proximal to Gerdy’s tubercle and extends proximally to the lateral intermuscular septum. Two or three fascial incisions [19] are made to visualize: (1) the LCL attachment site at the fibula and/or epicondyle, (2) the popliteus tendon and PFL, (3) the biceps tendon, and (4) the peroneal nerve. Neurolysis of the peroneal nerve is routinely performed that is protected throughout the procedure. If the patient has peroneal nerve palsy, we will locate the nerve at this point in the case and decompress it if it is in continuity [10]. In the case of a nerve tear with interruption, we would consider a subsequent surgery for nerve repair and grafting because the rehabilitative protocol for the nerve repair requires a longer period of immobilization.
15.7.1 ACL/PCL Reconstruction
Any autograft tissue is harvested first so that an assistant can prepare the graft on the back table while the surgeon continues the arthroscopic procedure. All of the grafts are kept moist until they are ready to be implanted. We perform an arthroscopically assisted ACL and PCL reconstruction using a single bundle and transtibial procedure for both ligaments. The first tunnel to be created is for the ACL using the Howell tibial guide pin (Arthrotek, Warsaw, IN). The pin is left in place and the tunnel drilled later in order to avoid fluid leakage. For the PCL femoral tunnel, we place only the pin without drilling. Right correct placement of this pin is critical. For single-bundle reconstruction of the PCL, the pin should be located at the center of the anterolateral bundle that is vertical (anterior). Reaching this point is easy using an in-out technique, but the tunnel will be angled too much with a risk of a “killer tunnel.” Therefore, we prefer an out-in technique, but in order to reach a point as vertical (anterior) as possible, we use an abrader blade to make a small notch in the roof at 12 o’clock, 5 mm posterior to the articular cartilage. In this way, the tip of a commercial drill guide can easily be placed in the correct position. The bullet of the guide pin is inserted below the bulk of the vastus medialis with the knee flexed 90° and midway between the femoral epicondyle and articular cartilage. Attention is then turned to the PCL tibial tunnel. The scope is shifted from the AL to the PL or the PM portal and a motorized shaver is introduced from the contralateral portal. The posterior septum is removed using the technique described by Ahn et al. [20]. In PCL surgery, a transeptal approach reduces the potential risk to neurovascular structures by providing complete visualization of the tibial PCL insertion and a larger work space. The wider field of vision allows for constant visualization of the tibial tunnel preparation and easier intra-articular passage of the graft. Furthermore, this technique reduces the need to use a 70° scope to view the posterior compartments. The insertion site of the PCL stump on the tibia is easily identified and the fibers of the remaining PCL remnant are dissected subperiosteally. After the posterior tibial sulcus is identified, the arm of the drill guide is inserted from the anteromedial portal and placed in the footprint of the PCL over the attachment of the anterolateral bundle, approximately 1.5 cm below the articular surface and in the midline of the tibia (Fig. 15.2). The guide pin is advanced until it is visualized through the posterior portal. If the pin needs to be repositioned, parallel guide pins may be useful. After placing the pin, the tunnel is drilled. Both tibial tunnels are drilled in different directions on the anteromedial surface of the proximal tibia in order to avoid crossing tunnels. Next, the femoral PCL and ACL tunnels are drilled. The edges of all tunnels are smoothed with a rasp prior to passing graft material. The grafts are pulled through the tunnels, the PCL graft first, facilitating intra-articular passage. Every graft-tensioning protocol represents a compromise [21] with a risk of stretching out one or both grafts due to excessive tissue forces, and over time we have changed our protocol. Currently, the ACL/PCL grafts are tensioned after all ligaments have been reconstructed but not yet fixed. The PCL is tensioned first in full extension and then fixed with the knee at 70° flexion, maintaining the tibia in a neutral position and with a “normal” step-off of the medial plateau. Before ACL fixation, we check the restoration of intra-articular points of contact and the restoration of the normal meniscal profile from one of the posterior portals. Then, the ACL is tensioned and fixed with the knee in near full extension. The choice of fixation method depends on the type of graft used.


Fig. 15.2
Arthroscopic view from the posteromedial portal of a drill guide placed at the posterior tibial sulcus
15.7.2 MCL/POL Reconstruction
Anatomical restoration will proceed from deeper to superficial structures and from posterior to anterior. The deepest layer consists of the meniscotibial and meniscofemoral ligaments. If they are lax at the time of diagnostic arthroscopy, they are re-tensioned with suture anchors with the knee in full extension. The superficial MCL is repaired with a semitendinosus graft, if available [22]. The tendon is left attached distally and a locking suture placed in the end of the graft to facilitate passage under the superficial layer. Anatomical attachment of the MCL on the femur is identified and the isometry of the selected point tested. When the proper femoral position is found, an eyelet-passing pin is drilled transversely across the femur, and a half-tunnel 25–30 mm in length is reamed according to the measured diameter of the double-looped tendon. With a long-looped suture attached to the eyelet, the tendon is passed through the femoral bone tunnel and secured using an interference screw. While inserting the interference screw, the knee should be held in 30° flexion with varus stress. The free portion of the graft is sutured back to the insertion of the semitendinosus using a permanent suture. An alternative [23, 24] is to perform a “double-bundle” technique that re-creates POL function. A tibial tunnel is drilled to the posterior corner of the medial tibial condyle from anterior to posterior and exits 10 mm below the tibial plateau. The free end of the graft is passed from the femoral condyle through the posterior tibial tunnel opening and fixed with an interference screw (Fig. 15.3). A similar technique has been described with allografts [25, 26]. If the native POL tissue is adequate, a vertical incision is made in the posteromedial capsule between the posterior border of the MCL and anterior border of the POL. The femoral or tibial redundancy is eliminated by imbricating the POL to the MCL in a pants-over-vest fashion or reattaching its insertion to the femur or tibia with suture anchors.


Fig. 15.3




Reconstruction of the superficial medial collateral ligament and the POL using the semitendinosus tendon
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








