Chapter 20 Chronic Leg Pain
CHAPTER CONTENTS
Introduction
As the general population in the United States has become more active, orthopaedists have observed an increase in the incidence of sports-related injuries. Nonspecific complaints of pain in the foot, ankle, calf, or shin are often reported, with shin pain as the most common presentation.1,2 Evaluation of leg pain not only requires knowledge of the anatomy and biomechanics of the lower extremity but also an understanding of the pathology of the injury. Conducting a thorough history and physical examination and appropriately interpreting diagnostic tests are essential to the establishment of an accurate diagnosis. In addition, specific details regarding physical activity, including training regimens, surface conditions, and shoewear must be determined, because these factors also play a significant role in the diagnosis.
Because several etiologies may present with similar characteristics, patients must be evaluated for multiple conditions.3 The differential diagnosis of chronic leg pain includes the following conditions: bony or soft-tissue tumors, chronic exertional compartment syndrome (ECS), claudication, isolated leg trauma, medial tibial stress syndrome (MTSS), muscle strains, nerve entrapment, popliteal artery entrapment syndrome (PAES), radiculopathy, referred pain from meniscal pathology, stress fractures, and tendinitis. Despite this wide range of diagnoses, several studies demonstrate that certain conditions are more prevalent among athletes, in particular.1,4–6 In a retrospective review of 72 track and field athletes with athletic-related injuries, 28% of injuries were due to overuse of the leg.4 Furthermore, chronic exertional shin pain accounts for approximately 10% to 15% of all running injuries and may be responsible for approximately 60% of all leg pain syndromes.1 In another retrospective study of 150 patients with exercise-induced leg pain, chronic ECS was the most prevalent cause of pain, representing 33% of cases; stress fractures and MTSS accounted for 25% and 13% of cases, respectively.6 Conversely, in our experience MTSS has been more prevalent than either chronic ECS or stress fractures. This chapter focuses on common causes of chronic leg pain in athletes, including MTSS, stress fractures, chronic ECS, nerve entrapment, and PAES. The incidence, pathology, clinical presentation, and treatment options are discussed for each condition.
Medial Tibial Stress Syndrome
“Shin splits” is a nonspecific diagnosis of posteromedial leg pain commonly used to describe not only MTSS but also a wide variety of other lower leg pain conditions, including chronic ECS, fascial hernia, muscle strains, periostitis, and stress fractures.2,3,5,7–9 One of the most common sites of overuse pain is the distal one third of the medial border of the tibia.9–12 Several terms, including medial tibial syndrome, MTSS, tibial stress syndrome, posterior tibial syndrome, soleus syndrome, and periostitis have been proposed to link this common clinical presentation to a specific condition.2,11–19 Medial tibial stress syndrome may be the most accurate of these terms, however, because it describes both the location and the likely pathophysiology of the syndrome.5,11,12,20
MTSS typically is observed in runners and individuals involved in jumping activities such as basketball and volleyball.3,8,11,18,21,22 In our experience it also represents the most common cause of chronic leg pain. Both biologic and biomechanical factors have been reported as possible causes of MTSS.10–12 Although the tibialis posterior muscle historically has been implicated as the source of this condition,9,16,22–24 a recent study of 50 cadaveric legs revealed that the tibial posterior muscle was more lateral, indicating that this muscle was not a likely source of MTSS.10 Other recent studies have identified the soleus, flexor digitorum longus (FDL), and crural fascia as sources of the pain.10,15,25 More specifically, a three-phase bone scan study of 10 patients with MTSS demonstrated low-grade uptake along a diffuse region of the posteromedial tibia, suggesting that the condition is related to the soleus muscle.15
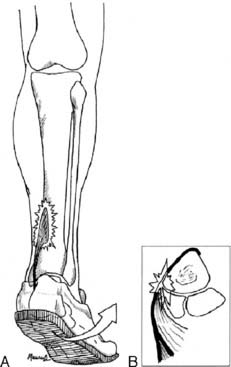
During running, heel strike occurs in relative supination, with pronation of the foot increasing until midstance.11,17,26 Because the soleus is the primary plantarflexor and invertor of the foot, it has been theorized that the medial portion of this muscle contracts eccentrically as the foot pronates (Fig. 20-1).17 The repetitive eccentric contraction that occurs in hyperpronating athletes may explain the increased incidence of MTSS observed in such athletes.5,9,11,14,17,25,27–29 In addition, hyperpronation is a compensatory mechanism that occur in patients with hindfoot and forefoot varus,25,26 tibia vara,26 tight Achilles tendon,26,28,29 and tight gastrocnemius and soleus muscles;26 therefore such patients also are at increased risk for developing MTSS.
History
The most common complaint associated with MTSS is a recurring, dull ache localized over the distal one-third posteromedial cortex of the tibia (Case Study 1). In our experience, MTSS tends to occur late in the sport season after prolonged activity, whereas stress fractures tend to occur early in an athletic season as stresses increase rapidly. Early in the development of MTSS, patients may experience pain at the beginning of a workout or run but feel a relief of symptoms with continued activity, only to be followed by a recurrence of pain either at the conclusion of the activity or some time afterward. Pain usually is alleviated with rest and generally does not occur at night. However, as this condition progresses, pain may occur throughout training or during low activity, such as walking, and possibly may continue during rest.
Diagnostic studies
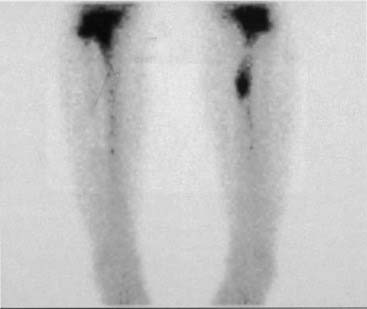
Roentgenograms generally are normal in patients with MTSS3,7,11,17,30 but are recommended to rule out abnormalities associated with other conditions such as stress fractures and tumors.3,11,12 A three-phase bone scan is warranted to rule out stress fractures if a conservative treatment program does not alleviate pain. This type of bone scan is a valuable diagnostic tool used to differentiate between MTSS and stress fractures, because each condition has a distinct scintigraphic pattern.7,9,11,15,17,31,32 A bone scan demonstrating a longitudinal and diffuse pattern in the distal one third of the tibia is indicative of MTSS (Fig. 20-2).9,11,15,32 In general, only delayed images are positive in cases of MTSS, whereas both early and delayed images demonstrate uptake in cases of stress fracture.11,15 In addition, magnetic resonance imaging (MRI) is another diagnostic tool for MTSS recommended by some authors.11,31 However, we believe that MRI has a limited role in the evaluation of MTSS because of its higher cost compared with other imaging options7 and its difficulty in delineating MTSS from stress fractures.
Treatment
Conservative
The recommended management of MTSS is multimodal, consisting of rest, nonsteroidal anti-inflammatory drugs (NSAIDs), and ice.3,12 Physical therapy modalities such as iontophoresis and ultrasound also may be used.3,12 Initially, rest or a decrease in training for 2 to 3 weeks is suggested and may be curative without further workup.12 Cardiovascular conditioning may be maintained during this period with swimming, upper body weightlifting, and deep-water running.11,12 Stationary biking is another option but should be performed with the heel on the pedal, a precaution that will diminish muscular stress transmission to the leg. NSAIDs often are prescribed to relieve pain11,12 and to decrease possible inflammation. Ice may be used to further reduce swelling and inflammation.12,31 Addressing biomechanical abnormalities is also recommended.12,33,34 For example, excessive pronation may be corrected with the use of custom or off-the-shelf orthotics.33 Physical therapy modalities, including massage, electrical stimulation, iontophoresis, and ultrasound also have been used.10,31,35 If pain is present with walking or at rest, range-of-motion boots and/or walkers are used. In rare cases, crutches may be necessary.
If the patient has not experienced pain during conservative treatment, a gradual return to training may be initiated. Warm-up and cool-down routines, including stretching, are advised with each workout to prevent recurrence of symptoms. If the patient remains asymptomatic, progression of training is recommended at increments of 10% to 25% for 3 to 6 weeks.11 If symptoms return, activity should cease for at least 2 weeks before training is resumed at a lower intensity and duration.
Operative
Fasciotomies of the posterior compartments of the tibia are possible treatment options in patients with intractable MTSS.6,11,14,34,36 In these rare cases, fasciotomies may alleviate the pull of the soleus and deep compartment muscles on the corresponding fascial insertions.6,11,14,34,36 However, in our experience, conservative management alone has been successful in treating MTSS cases, eliminating the need for surgical intervention.
Stress Fractures
Repetitive loading caused by overuse or overloading of the lower leg results in microtrauma to the bone that eventually may lead to stress fracture.6,35,37–39 Stress fractures of the tibia are more frequent3,11,37,40–44 and more problematic to treat than those of the fibula. Fibula stress fractures tend to heal more rapidly and generally do not require adjunctive therapy.41,43 The focus of this section is on tibial stress fractures because most fibula stress fractures occur about the ankle and are covered elsewhere.
Most fractures of the tibia occur in the proximal metaphyseal or upper diaphyseal regions,35,44,45 whereas tibial fractures that are longitudinal in nature46–49 or occurring in the midanterior region9,35,37,38,50,51 are less prevalent. Athletes, in particular, are subject to stress fractures of the leg. Specific stress fractures also are related to certain types of activities. For example, the more common posteromedial stress fracture usually is associated with running activities.11,35,46 Conversely, midanterior tibial cortex stress fractures often are associated with dancers and athletes involved in cutting and jumping activities.35,38,50–54
Risk factors for developing a stress fracture include excessive training, training errors, biomechanical variants, and menstrual irregularities with corresponding changes in bone density.9,11,40,42,46,55,56 Excessive training, particularly common early in the athlete’s season, causes overuse or overloading, which may result in stress fracture.6,35,46 In addition, overlapping of sport seasons, which often occurs when teenage athletes participate in multiple sports, also may lead to an overuse scenario. Training errors, including changes in training surface, shoewear, and technique often result in overloading, which may result in stress fracture.6,35,37 Weather and seasonal differences affect surface conditions for many outdoor sport activities and may increase the risk of stress fracture. For example, dry conditions and the fall season are both associated with hard ground surfaces, which result in an overloading environment for soccer players. Simple measures, such as watering soccer fields when the ground is hard, may reduce the risk of stress fracture and other injuries by minimizing loading conditions. Biomechanical factors, such as cavus feet, leg-length inequality, and muscular imbalance also may increase the risk of developing a stress fracture.9,11,40,44 Finally, low body weight and menstrual abnormalities in female runners have been associated with an increased incidence of stress fractures.39,40,42,55
The cause of stress fractures is multifactorial in nature and often results from an imbalance of natural bone formation and resorption cycle because of repetitive loading.37,44,51,56 One theory proposed to explain the mechanism of stress fracture suggests that muscle fatigue results in the transmission of excessive forces to the underlying bone, ultimately leading to stress fracture.20,37,44,51,55 Another hypothesis asserts that simple, repetitive weight bearing leads to a concentrated rhythmic muscle action, which causes excessive transmission of forces beyond the threshold of bone, thereby resulting in fracture.20,37,44,51,57 Forces from large posterior muscle groups, in particular, may cause increased tension on the anterior cortex of the tibia, possibly leading to the problematic midanterior tibial stress fracture.51
History
Pain associated with tibial stress fractures is more proximal than that caused by MTSS (Case Study 2). Although pain typically is localized to the fracture site, diffuse pain also may occur. Stress fracture pain will develop gradually, occurring initially as a mild ache following a specific amount of exercise and then subsiding. As the condition progresses, pain may become severe and occur during earlier stages of exercise and after cessation of activity. In rare cases, night pain also is possible. Any complaints of constitutional symptoms, including fever and fatigue, should raise concern of a possible tumor or infectious process.
Diagnostic studies
A clinical diagnosis of stress fracture often may be made solely on the basis of the history and physical examination,37,56 but diagnostic imaging may confirm the diagnosis or assist in identifying the stress fracture in questionable cases. Plain roentgenograms should be performed as the first imaging step but may be negative, because radiographic abnormalities often are not observed until 2 to 3 weeks after the onset of symptoms.3,37,44,46 Radiographic abnormalities may appear as a faint periosteal reaction, a fluffy area of callus, or a cortical lucency.39 If radiographic examination demonstrates the presence of a stress fracture, no further imaging is necessary.
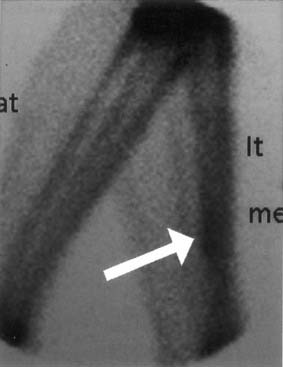
A three-phase bone scan is indicated when suspicion of stress fracture remains despite negative radiographs.39,46 The specific scintigraphic pattern of a stress fracture demonstrates focal uptake in the area of fracture (Fig. 20-3).37,58 MRI, another diagnostic option, differentiates among fracture, tumor, and infection and also localizes the pathology.31,44,46,56,59 However, because a diagnosis often may be determined by plain radiograph or bone scan, both of which are more cost effective than an MRI, we reserve MRI for special cases, including a history of allergic response to dye, an aversion to needles, or an atypical presentation. An MRI also is useful in differentiating between longitudinal stress fractures and MTSS, the more commonly observed overuse injury, because bone scans of these conditions demonstrate identical diffuse uptake in the distal one third of the tibia (Case Study 3).
Case Study 3
Neurovascular and physical examinations were grossly normal. No swelling was observed, but palpation revealed mild tenderness along the distal tibia. Plain radiographs did not reveal the presence of a fracture or periosteal reaction. An MRI was ordered to differentiate between the suspected longitudinal stress fracture and possible MTSS and subsequently demonstrated a longitudinal stress fracture in the tibial metaphysis with surrounding bone edema (Fig. 20-5). Conservative treatment involving a range-of-motion boot and nonweight-bearing ambulation was recommended. Six weeks following treatment, plain radiographs demonstrated a slight callus formation, indicative of the healing process. As a result, the patient was instructed to progress from partial to full weight-bearing ambulation over a 4-week period. Full weight-bearing ambulation in a range-of-motion boot continued for an additional 4 weeks, with subsequent introduction of a regular shoe. At 4½ months, the patient resumed her walking program with a gradual increase in mileage.
In addition to its diagnostic capabilities, imaging also assists in differentiating among the various types of stress fractures. For example, radiographs depicting a small lucency or a “dreaded black line” in the midanterior cortex of the tibia are indicative of a midanterior cortex tibial stress fracture (Fig. 20-4, A).35,46 Because of the relatively avascular nature of this portion of the tibia, a bone scan initially may be interpreted as negative, but closer examination will depict an area of decreased uptake at the fracture site.46,54 If this type of fracture is not initially diagnosed and treated, a complete fracture may result. Conversely, plain radiographs of longitudinal tibial stress fractures often are normal, whereas bone scans will demonstrate increased uptake in the lower tibia.60
Treatment
Conservative
Conservative treatment for stress fracture is focused on pain relief and protection from further injury.39,46 Improvement in muscular strength and endurance, continuation of cardiovascular fitness, and management of biomechanical factors also are important. Relative rest, possibly with weight-bearing restriction, is recommended for a minimum of 2 to 4 weeks. Mild analgesics or NSAIDs also may be prescribed in conjunction with physical therapy modalities, such as ice or cross training.38,46 Cardiovascular fitness should be maintained with cycling, swimming, deep-water running, or other nonloading activities.39,44,46,58 Upper body strength training is recommended to maintain muscle mass and is not likely to jeopardize fracture healing.44 Bracing or casting may be required for 3 to 12 weeks to immobilize the fracture adequately in severe cases or if pain is not relieved after the initial 2- to 4-week rest period.33,61 Because prompt return to activity is a priority for elite athletes, electrical stimulation is highly recommended. Electrical stimulation also has been effective in healing nonunioned traumatic fractures.35,46,50,51
Contributing factors, such as training errors, improper shoewear, and muscle imbalance that were identified in the history and physical examination also must be addressed.6,39,44 Training regimens should be individualized for each patient. Treatment plans for athletes with eating disorders or females with menstrual irregularities should involve dietary counseling and/or estrogen replacement therapy to accelerate healing and to prevent future problems.37,46 Shoes should be examined for signs of wear and inadequate support and also must be replaced every 500 km.38,46 If necessary, appropriate orthotics should be implemented.
Return to activity should be gradual and individualized according to symptoms, with an emphasis on progress only when activity is accomplished without pain.44,46 It must be stressed that activity should cease if any pain occurs and should not be reattempted until the pain is alleviated.46,58 In addition, once the pain is alleviated, the patient must return to the lower loading activity and not advance until each successive activity has been accomplished without pain. A period of rest also must be implemented between activities before advancing to a higher loading activity. Although athletes may resume full training in 8 to 16 weeks, patients must be aware that a prolonged recovery period may be required for more severe stress fractures.51,54 Midanterior cortex tibial stress fractures, in particular, require a significant period of rehabilitation.3,38,46,50,51,58 Despite this prolonged rehabilitation, conservative treatment is similar to that for other tibial stress fractures and includes avoidance of activity, bracing or casting, and possible electrical stimulation.46,51,54
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 Pearl
Pearl