Chapter 7 Chiropractic Technique
Subluxation, mobilization, manipulation, adjustment, long lever arm, short lever arm, force, thrust, facilitation, nociceptors, somatic dysfunction, trigger points, spondylotherapy
After reading this chapter you should be able to answer the following questions:
| Question 1 | What has led to the multiplicity of chiropractic techniques? |
| Question 2 | What causes cavitation? Is it a necessary outcome of manipulation? |
| Question 3 | What distinguishes manipulation from mobilization? |
| Question 4 | How can the amount of force be minimized in manipulative procedures? |
| Question 5 | What are the common mechanical, soft tissue, neurologic, and psychologic effects of manual therapy? |
| Question 6 | What is the proposed effect of chronic segmental facilitation? |
| Question 7 | What is the rationale for the use of manual therapy to ameliorate negative somatoautonomic reflexes? |
Chiropractic has maintained that the most specialized and significant therapy employed involves the adjustment of the articulations of the human body especially the spinal column. This may be done manually or mechanically, actively or passively, with the purpose of restoring normal articular relationships and function, as well as reestablishing neurologic integrity and thereby influencing physiologic processes. Although most chiropractic techniques impart a thrust, many techniques are designed to affect physiologic processes without involving the use of a thrust procedure. This chapter discusses the theory and evidence supporting these procedures.
Historical Perspective
Osseous manual thrust techniques have been used to treat various conditions since early recorded history. Records of 4000-year-old artwork from Thailand depict the use of manual therapy, as do artifacts from early Egyptian, Polynesian, Japanese, Chinese, and Native American cultures. It appears that many ancient civilizations developed various forms of manipulation for the treatment of various disease processes.1,2
In the Corpus Hippocratum, Hippocrates (The Father of Medicine, 460-370 BC) described a form of spinal manipulation assisted by long axis distraction. The patient lay prone and was stretched by applying long axis distraction. When sufficient long axis distraction was applied, the physician would make palmar contact, reinforced by the opposite hand, over the “hump.” The doctor could then deliver a straight thrust in a posterior to anterior direction or, if indicated, change the line of correction superiorly or inferiorly (Figure 7-1). Hippocrates also described variations of this manipulative technique; instead of contacting the hump with a palmar contact, the physician could sit on the hump or even place a foot over the hump. When even more force was indicated, a board was used. With one end anchored to the wall and the middle of the board resting over the hump, the physician could push down on the free end of the board, using it as a lever to induce a posterior to anterior force onto the hump.3 Galen, Celisies, and Orbsius all used spinal manipulation techniques for various spinal deformities, neurologic deficiencies, and disease processes.

Figure 7-1 Spinal manipulation as described by Hippocrates.
(From Schoitz EH. Manipulation treatment of the spinal column from the medical-historical standpoint. Part I. Journal of the Norwegian Medical Association 1958; 78:359-72. Norske Laegeforening.)
During the Middle Ages, there exists a void in writings describing manual procedures. By the nineteenth century, a renewed interest in manual therapy was seen. In the early 1800s, Doctor Edward Harrison was renowned in London for his expertise in manual procedures. Like many others in the nineteenth century, he was shunned by his colleagues, who were more interested in practicing pharmacology and surgery.
In the days of the bonesetters, knowledge and techniques were passed down from generation to generation without formal training. After Palmer organized chiropractic into a system, he opened the first chiropractic college in 1896.4 Many of his early students went on to establish schools of chiropractic that in turn produced students who opened other schools.
In the next century, more than 100 “named techniques” were developed.5 It is necessary to understand that because a wide variety of methods exists, the assumption that all forms of manual therapy are equivalent must be avoided.6 Many of the developed technique systems do not use high velocity low amplitude thrusts. One can only speculate about the reasons why technique systems not using thrust procedures developed. One such reason may be that certain patient presentations would either contraindicate or at least not indicate the use of a thrust technique. Examples are patients who are elderly or osteoporotic, in extremely acute pain, in later stages of pregnancy, or who have specific pathologies. Another reason might be the doctor’s inability to produce a thrusting force that is capable of making a joint change. If the doctor’s size, strength, or ability to develop the needed speed is inadequate to produce the appropriate force, some other type of technique application is necessary. Most of these “named techniques” had their origins in devoted and inquiring practitioners. These practitioners may have modified a particular technique to fit their own physical needs or to fit the needs of their subluxation conceptual model. Some observed a phenomenon of patients’ improvements and developed a technique around this phenomenon. Regardless, many of the named techniques were developed out of the desire to improve the practitioner’s ability to deliver health care.
Terminology
As the chiropractic profession developed into the second largest health care delivery system outside of medicine, it also developed in many directions. With the lack of communication between the practitioners of different chiropractic techniques, each school of thought evolved as an independent entity. Schools expanded philosophies, refined techniques, and redefined terms. Although communication was a necessity for survival, there existed a severe communication gap. After the 1975 National Institute of Neurological Communicative Disorders and Stroke (NINCDS) Conference that evaluated the research status of spinal manipulative therapy, manual procedures were no longer considered invalid and became the object of study for a number of professions besides chiropractic. Practitioners of medicine, naturopathy, and physical therapy, in addition to osteopathy, began to study and employ manipulation and other manual techniques. The chiropractic profession was being forced to communicate with other branches of medicine, but a common language no longer existed to allow successful dialogue. Out of this dilemma, a subcommittee of the Standards of Care Committee from the Consortium for Chiropractic Research began to develop nomenclature through consensus. (See Chapter 1.) Through this consensus process, Gatterman and Hansen7 defined the terms manual therapy, manipulation, mobilization, adjustment, subluxation, subluxation complex, and subluxation syndrome (Box 7-1).
BOX 7-1 Manual Therapy Terminology
From Gatterman MI, Hansen D. J Manipulative Physiol Ther 1994;17:302-9.
The term technique should not be confused with the terms therapy or treatment. Technique should be reserved for describing a specific manual procedure, whereas therapy and treatment include the application of the primary and ancillary procedures indicated in the management of a patient with a given health disorder. These procedures are limited by individual statutory practice acts, but they may include such procedures as joint mobilization, therapeutic muscle stretching, soft tissue manipulation, sustained and intermittent traction, meridian therapy, physiological therapeutic modalities, application of heat or cold, dietary and nutritional counseling, therapeutic and rehabilitative exercises, and biofeedback and stress management.2
Manual therapy is therefore applied in many forms, including massage, mobilization, traction, muscle energy techniques, adjustment, and manipulation. The common characteristic in all of these methods is the application of external forces to the body for the purpose of affecting the flexibility and pain-free function of the spine and its contiguous tissues.8 Moreover, all of these methods act on sensory receptors, usually in the region where the pain is felt or where it originates to produce a reflex response.9 Pain warns us mainly against harmful functioning, and it is disturbance of function that is the most common cause of pain originating in the locomotor system. Movement restriction (blockage) at the segmental level and disturbed motor patterns at the central level may serve as examples.10 The form of therapy used must vary according to the structures upon which it is to act. The optimal treatment for joint or spinal segment movement restriction is some form of manual therapy (Box 7-2).9
BOX 7-2 Goals of Manual Therapy
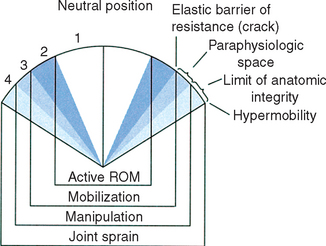
Sandoz11,12 defines the chiropractic adjustment as a passive manual maneuver during which the three-joint complex is suddenly carried beyond the normal physiological range of movement without exceeding the boundaries of anatomical integrity (Figure 7-2). However, various forms of manual therapy exist affecting different aspects of joint function and without the use of a thrust. (See Figure 7-2.) Regardless of the procedure used, the therapeutic emphasis is not on forcing a particular anatomical movement of a joint, but on restoring normal joint mechanics. Most forms of manual therapy result in movement of joint surfaces either actively or passively with the purpose of restoring normal articular relationships and function as well as restoring neurologic integrity and influencing physiologic processes.
Regardless of the specific form, the goals of manual therapy include a combination of mechanical effects, soft tissue effects, neurologic effects, and psychological effects. Although these effects are usually considered or discussed separately, the division is purely academic because the effects of manual therapy cannot be specifically directed or limited. In other words, one cannot apply a manual procedure and consistently achieve a single or specified effect. For example, when using a thrust technique to create a motion or alignment change (mechanical effect), input to the joint receptors (neurologic effect) occurs, muscles and ligaments (soft tissue effect) are compressed, stretched, or lengthened, and the patient is aware that something was done (psychologic effect). Therefore these categories are developed and designed only for an easier understanding of the principles for applying the various forms of manual therapy.
Mechanical Effects
The mechanical effects of manual therapy include changes in joint alignment, dysfunctional joint motion, and spinal curvature dynamics. Generally, the mechanical effects of an adjustment will be on derangements of the somatic structures of the body that have altered joint function. Causes of altered joint function are acute injury, repetitive use injury, faulty posture or coordination, aging, congenital or developmental defects, or primary disease states. There are several causes of acute and chronic mechanical joint dysfunction (Box 7-3).
Gatterman13 and Rahlmann14 have reviewed the causes of joint dysfunction (subluxation) and concluded that more than one mechanism is likely to be involved in the development of joint dysfunction, although immobilization due to adhesions had the strongest literature support. Therefore all mechanisms will be considered here. (See Chapter 11.)
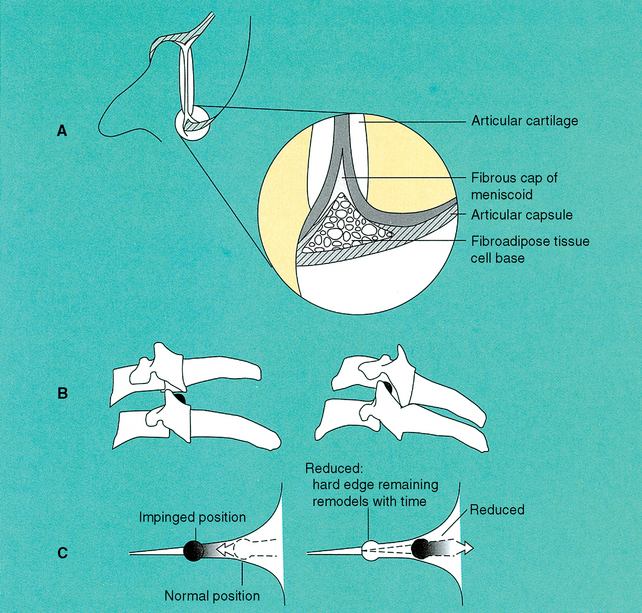
Intraarticular meniscoids are leaflike fibroadipose folds of synovium that are attached to the inner surfaces of the joint capsules and project into the joint cavities (Figure 7-3). These meniscoids have been found to be present in all of the posterior joints of the spine. Bogduk and Jull15 have suggested that extrapment of these meniscoids may be the cause of restricted joint motion. Upon flexion, the inferior articular process of a zygapophyseal joint moves upward, taking the meniscoid with it. Upon extension, the inferior articular process returns towards its neutral position. Instead of reentering the joint cavity, the meniscoid impacts the edge of the articular cartilage and buckles, creating a space-occupying lesion under the capsule. Pain occurs because of capsular tension and extension motion is restricted. The application of a procedure that will separate the articular surfaces may release the extrapped meniscoid.15
Cyriax16 espouses the belief that displaced nuclear material along an incomplete radial fissure is the source of joint fixation. Postmortem dissection studies of degenerated discs have indeed identified radial fissures in the annulus fibrosis. Nuclear migration along these radial fissures has also been demonstrated by CT discography and correlated with the patient’s pain.17 A couple of questions remain unanswered regarding the disc’s ability to restrict motion. First, annular fissures are apparently irreversible and do not mend with manipulation, yet manipulation can have an immediate and, often, lasting effect on joint dysfunction. Moreover, joint dysfunction and fixation can occur at segments where there are no intervertebral discs, such as the atlanto-occipital articulation and the sacroiliac articulations, to say nothing of the extremity joints. Finally, disc pathology can lead to spinal fixation through reflex muscle spasm. A painful and inflamed annular tear or disc herniation will cause reflex muscle spasm that restricts motion.
Specific joint derangements are thought to create a mechanical blockage of movement and an unleveling of the motion segment, resulting in tension on the joint capsule and posterolateral annulus. Because the joint capsule and posterior annulus are pain-sensitive structures, tension on these elements may reflexively induce muscle splinting with further joint restriction. Mechanical joint dysfunction is therefore considered a significant and frequent cause of spinal pain and a potential source of spinal degeneration.
A mechanical effect of manipulation that is intriguing, but not necessarily clinically important, is the process of joint cavitation. Studies performed by Roston et al.18 and Unsworth et al.19 demonstrate that as tension is applied causing a separation of the joint, there is a point where the joint surfaces jump apart, coinciding with a cracking noise. Once the tension is removed from the joint, the surfaces approximate themselves once again but at a distance slightly more apart. As the elastic barrier is passed, the articular surfaces separate suddenly, the cracking noise can be heard, and a radiolucent space appears within the joint space. The explanation of the radiolucent space rests with the fact that there is normally a small negative pressure present in a synovial joint. Its purpose is to maintain the cartilage surfaces in apposition and augment joint stability. Separation of the joint surfaces beyond the elastic barrier creates a drop in the interarticular pressure and gas is suddenly liberated from the synovial fluid to form a bubble in the joint space. The bubble bursts almost immediately with an audible crack. Analysis of the gas produced by synovial fluid cavitation was shown to consist of over 80% carbon dioxide.19
Brodeur20 has presented a slightly different model of joint cavitation and cracking based on a mechanism described by Chen and Israelachvili.21 Within this model, the capsular ligament plays a primary role in the production of joint cavitation and cracking. During the first phase of joint manipulation as the joint is being loaded and the joint surfaces are being distracted, the joint and the capsular ligament invaginate (draw inward) to maintain a constant fluid volume within the joint space. As distractive pressure is increased, the capsular ligament reaches its elastic limits and snaps away from the synovial fluid, producing cavitation at the capsular-synovial interface. A rapid increase in joint volume follows and the gas bubbles formed at the periphery rush to form a single coalesced bubble in the center of the joint space. Brodeur20 speculates that the “snap-back” of the capsular ligament is the event responsible for the audible crack. He also proposes that this mechanism explains why some individuals with very tight or loose joint capsules do not crack:
Soft Tissue Effects
The soft tissue effects of manipulation include changes in the tone and strength of supporting musculature and influences on the dynamics of supportive capsuloligamentous connective tissue (viscoelastic properties of collagen). Connective tissue elements lose their extensibility with immobilization.22 With immobilization, water is released from the proteoglycan molecule, allowing con-nective tissue fibers to contact one another, which encourages abnormal cross-linking that causes loss of extensibility.23 It is hypothesized that certain manual therapies can break the cross-linkages and any intraarticular capsular fibroadipose adhesions, thereby providing free motion and allowing water imbibition to occur. Furthermore, action of these manual therapies can stretch segmental muscles, causing spindle reflexes that may decrease the state of hypertonicity.24 The effects of immobilization are summarized in Box 7-4.25
BOX 7-4 Effects of Immobilization
Microscopic effects:
Loss of parallelism of collagen fibers
Increased randomness of matrix organization
Intraarticular effects:
Pressure necrosis of the articular cartilage
Extension of marrow space into the subchondral plate
Cartilage erosion and ulceration in noncontact areas
Adhesions to articular cartilage
Adapted from Akeson WH, Amel D, Woo SLY. Cartilage and ligament: physiology and repair processes. In: Nicholas JA, Hershman EB, editors. The lower extremity and spine in sports medicine. St. Louis: Mosby; 1986. p. 3-41.
After immobilization, joints become stiff. Although some stiffness results from intraarticular adhesions to surfaces that normally glide past one another,26 there is also evidence that ligamentous structures can shorten (contract) and limit joint motion.27 It is likely that joint stiffness results from a combination of adhesion formation between normally gliding surfaces and active changes in ligament length. Manual therapy applied to restricted joints will presumably tear the collagen cross-links and fibrous adhesions formed during joint immobilization. However, when articular or nonarticular soft tissue contractures are encountered, incorporation of procedures that minimize inflammation and maintain mobility should be considered. Viscoelastic structures are more amenable to elongation and deformation if they are first warmed and then stretched for sustained periods.28 Therefore the application of moist heat, ultrasound, and other warming therapies might be considered before applying sustained manual traction or home-care stretching exercises.2
Neurologic Effects
The neurologic effects of manipulation include reducing pain, influencing spinal and peripheral nerve conduction, thereby altering motor and sensory function, and influencing autonomic nervous system regulation. Wyke29 reported that manipulative procedures can stimulate the mechanoreceptors associated with synovial joints and thereby affect joint pain. He has identified four types of joint receptors. Types I, II, and III are corpuscular mechanoreceptors that detect static position of the joint, acceleration and deceleration of the joint, direction of movement and over-displacement of the joint. The Type IV receptor is a network of free nerve endings that have nociceptive capabilities. Type IV receptors are inactive under normal conditions. However, if noxious mechanical or chemical stimulation or if Types I-III receptors are not able to function, Type IV receptors become active and the sensation of pain is perceived. If manipulative therapy can restore normal function to the joint, allowing Types I-III receptors to function, the Type IV pain receptors should be inhibited, thereby decreasing the patient’s pain. The structures most sensitive to noxious stimulation are the periosteum and joint capsule.
There is also evidence to support the concept that the spinal adjustment increases pain tolerance in the skin and deeper muscle structures, raises beta-endorphin levels in the blood plasma, and has an impact on the nerve pathways between the body wall and viscera that regulate general health.30–35 Furthermore, a significant factor in musculoskeletal function is the musculature and its nerve control. Each individual will have a “postural personality” that is an expression of the individual’s muscular patterns and posture. A frequent cause of joint dysfunction may therefore be faulty neuromotor patterns due to muscular imbalance and postural strain9 or an inability on the part of the patient to consciously control musculoskeletal function.
There are many controversies in the application of manual therapy. Of significance is the role of pain in deciding on the appropriateness of manual procedures. Mitchell36 states that if one treats the part where the patient experiences the pain, one will be treating the wrong part of the body most of the time. He goes on to quote Osler, stating “pain is a liar.” Mitchell bases this idea on the concept that in the musculoskeletal system, pain almost always develops and persists in the structures which are stressed the most by the adaptation to the dysfunction. The opposite idea is extolled by Lewit,9 who states that if a manual therapy treatment is successful, it will usually produce immediate relief of pain. He adds that by far the most frequent cause of pain is disturbed function. This may involve passive joint mobility or active movement patterns. Manual therapy is directed to movement restriction of joints or motion segments of the spinal column. Pain in the locomotor system is therefore looked upon as a warning sign of harmful functioning that should be corrected in time before it causes permanent damage. Lewit also emphasizes that undiagnosed impairment of motor function is the most frequent cause of pain without a specific diagnosis, and that treatment of the pain without a thorough understanding of the functioning of the locomotor system is courting failure.9
Psychologic Effects
The psychologic effects of the laying on of the hands cannot be denied nor overlooked. Paris37 states that with the addition of a skilled evaluation involving palpation for soft tissue changes and altered joint mechanics, the patient becomes convinced of the interest, concern, and manual skills of the clinician. If at the conclusion of the examination, a manual procedure is performed that results in an audible “pop” or “snap,” the placebo factor will be undeniably high. Paris37 states that some patients report total relief within a second or two following such a procedure which he considers far too short a time for any genuine benefit to be appreciated. The astute clinician accepts and reinforces this phenomenon, recognizing that the patient is in need of all possible assistance. It should be noted, however, that the response rate to manipulative treatment cannot be totally accounted for by the placebo effect.
Moreover, the body and mind are not separate, but really one system coordinated by the neuropeptides.38 The tendency in the health care delivery system is to deal primarily with the physical aspects of health and ignore the emotional dimension—thoughts, feelings, the spirit, the soul. Today’s health care provider should recognize the interconnectedness of all aspects of human emotion and physiology. The skin, the spinal cord, and the organs are all nodal points of entry into the psychosomatic network.
Joint Assessment Procedures
Primary health care providers, with whom patients can consult, must as portal-of-entry physicians use findings derived from the case history, physical examination, clinical laboratory, and indicated special testing procedures to assess the patient’s state of health and determine the nature and cause of any ailments. The steps leading to a decision about how and what to treat are the most important part of any interaction between a doctor and a patient.1 The differentiation of many conditions responsible for joint pain, including distinguishing an intervertebral disc lesion from facet or articular involvement, is sometimes based upon clinical intuition rather than true objective procedures. This is especially the case when the back pain is not typical for either. However, the chiropractic spinal examination and joint assessment set chiropractic apart from other areas of the healing arts. Knowing how complex the human body is, specifically the neuromusculoskeletal system, it wouldseem inappropriate to use a single evaluative procedure to decide on the presence of a manipulable lesion. No one evaluative tool should be used or relied on to make clinical decisions.
Structured evaluation of the integrity of the joint systems of the body should be viewed in terms of a multidimensional index of abnormality. The examination of the musculoskeletal system should never be done in isolation, but should be done within the confines of the rest of the clinical evaluation. The methods used in identifying the presence of joint dysfunction (subluxation) include the usual physical examination processes of observation, palpation, percussion, and auscultation. Because of the complexity of the human body and, more specifically, the neuromusculoskeletal system, it is appropriate to employ an evaluative system that combines clinical indicators to decide on those joints in greatest need of intervention. No one evaluative procedure should be used or relied upon to make clinical decisions. The structural evaluation of the spinal column should be viewed in terms of a multidimensional index of segmental abnormality. The mnemonic PARTS (Box 7-5) is used to identify the five diagnostic criteria for identification of joint dysfunction.2,39
BOX 7-5 PARTS Mnemonic for Identifying Characteristics of Joint Dysfunction
T—Tone/Texture/Temperature of Soft Tissues
Characteristics of the Adjustive Thrust
Whereas manual therapy is a term broadly used to define the therapeutic application of a manual force (see Chapter 1), chiropractors emphasize the application of specific adjustive techniques.40 Chiropractic manipulation is a unique form of manipulation characterized by a specific high-velocity, short-amplitude thrust.41
It is necessary to understand that a wide variety of methods exist so that the assumption that all forms of manipulations are equivalent can be avoided.41 Factors that influence the selection of manipulative procedures include age of the patient, acuteness or chronicity of the problem, general physical condition of the patient, clinician’s size and ability, and effectiveness of previous therapy, present therapy, or both. Other factors to consider are knowledge of the local anatomy, including the geometric planes of the articulations, the nature of the condition and presence of comorbidities, and the mechanical characteristics of the manual procedure. These factors determine whether to use a long or short lever procedure, the positioning of the patient, specific contact points, the magnitude and vector of the force, and the type of thrust. Box 7-6 lists the factors governing the selection of adjustment methods.42
BOX 7-6 Factors Governing the Selection of the Specific Application of Manual Therapy
Patient’s age and physical condition
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree