9 Fractures of the cervicothoracic junction account for 9% of all cervical fractures. These injuries can frequently be missed on initial radiographic evaluation because of the difficulty imaging this area with plain-film radiographs. The problem is more often found in muscular or obese individuals. The cervicothoracic junction, like the occipitocervical and thoracolumbar junctions, is at particular risk for injury. This is because the cervicothoracic junction is a transition zone between the flexible and mobile cervical spine and the rigid thoracic spine. The complex biomechanical forces acting on this region make immobilization with external orthosis challenging. For unstable injuries and in patients with neurologic deficits in particular, surgical stabilization is preferred. Very little has been written on cervicothoracic injuries, and there is no specific classification system. They have often been classified using systems devised for the subaxial cervical spine. The system most frequently used was developed by Allen and Ferguson et al. A newer classification system, called the Subaxial Injury Classification system (SLIC), was recently proposed by the Spine Trauma Study Group (Table 9.1). This scoring system is helpful in guiding treatment. Scores of 5 or higher usually require surgical management, and scores of 3 or lower can usually be treated nonoperatively. A score of 4 may be considered for either operative or nonoperative management. The biomechanical differences between the subaxial cervical spine and the cervicothoracic junction may make using a subaxial classification scheme less ideal, but to date it is the best option to help guide treatment. Common fracture patterns seen in this region include unilateral or bilateral facet dislocations, burst fractures, and fracture dislocations. Table 9.1 Subaxial Injury Classification Scoring System
Cervicothoracic Fractures and Dislocations
![]() Classification
Classification
Points | |
Morphology | |
No abnormality | 0 |
Compression | 1 |
Burst | +1 = 2 |
Distraction (e.g., facet perch, hyperextension) | 3 |
Rotation/translation (e.g., facet dislocation, unstable teardrop or advanced-stage flexion-compression injury) | 4 |
Discoligamentous complex (DLC) | |
Intact | 0 |
Indeterminate (e.g., isolated interspinous widening, MRI signal change only) | 1 |
Disrupted (e.g., widening of disk space, facet perch, or dislocation) | 2 |
Neurological status | |
Intact | 0 |
Root injury | 1 |
Complete cord injury | 2 |
Incomplete cord injury | 3 |
Continuous cord compression in setting of neuro deficit (neuro modifier) | +1 |
 Workup
Workup
Physical Examination
Initial management of patients with cervicothoracic injuries should follow the same principles as for any trauma patient. Cervical spine immobilization should be maintained during the resuscitation and evaluation phase. The multiply injured patient is at increased risk for missed fractures as attention is focused on other, more obvious injuries.
Spinal Imaging
A thorough radiographic evaluation is mandated in these patients. The lateral cervical spine view should include the top of T1 and allow visualization of the C7–T1 disk space and the C7–T1 facet joints posteriorly. If the lateral cervical spine view is inadequate, a swimmer’s view should be obtained. This can sometimes be difficult to interpret because of overlying structures, particularly in patients who are muscular or obese or who have short necks. If there is any question with the swimmer’s view, a computed tomography (CT) scan with thin cuts and sagittal reconstructions should be performed (Fig. 9.1). Most trauma centers now routinely obtain cervical CT scans in trauma patients. When a disk herniation, epidural hematoma, or ligamentous injury is suspected, a magnetic resonance imaging (MRI) scan can be helpful. Widening of the interspinous distance or subtle facet subluxation needs to be carefully evaluated to rule out a ligamentous injury.
 Treatment
Treatment
Management of cervicothoracic injuries depends on the stability of the specific fracture. Stable fractures, such as spinous process fractures, lamina fractures, stable burst fractures, and facet fractures without subluxation, can be treated with an external orthosis, such as a rigid cervical collar, a cervicothoracic orthosis (CTO), or a halo vest. Patients with unstable injuries (such as facet dislocations, fracture dislocations, or unstable burst fractures) and patients with a neurologic injury are best treated with surgical management. This allows for restoration of normal spinal alignment, immediate stabilization, and rapid rehabilitation. In patients with fracture dislocations or subluxations, immediate closed reduction with traction may be attempted. These injuries are sometimes difficult to reduce closed; however, there are reports of high rates of successful closed reductions using weights up to 60% of body weight or greater.
Options for surgical intervention include anterior procedures, posterior procedures, or combined anterior and posterior procedures. Anterior procedures are primarily indicated for anterior vertebral column injuries, such as burst fractures with canal compromise in patients with a neurologic deficit. The complex anatomy in this region can make this approach quite challenging. In patients with long, thin necks, a low anterior cervical approach may be adequate; however, for many individuals some form of sternotomy is required, particularly at the T2 and T3 levels. Modifications of the classic sternal splitting approach involving osteotomies of the clavicle and medial portion of the manubrium have also been described with less morbidity. The posterior approach is the most widely used approach for the management of cervicothoracic injuries. Most fractures and fracture dislocations can be treated via this approach. Clinical results using thoracic pedicle screws and cervical lateral mass screws have shown a high rate of success and are biomechanically superior to wiring or hook instrumentation.
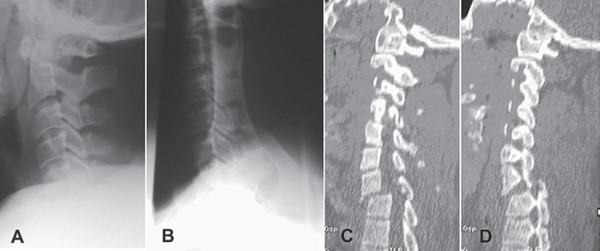
Fig. 9.1 A 36-year-old man fell 70 feet from a scaffold. (A) Inadequate initial lateral. (B) Inadequate swimmer’s view. (C,D) Sagittal reconstruction CT showing C7–T1 fracture dislocation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







