Type 1: Impacted condyle fractures
Type 2: Condyle fractures with fractures of the subcranium
Type 3: Sprain fracture of one or both condyles
The advantage of this classification is its therapy-decisive character, as types 1 and 2 can be seen as stable and should be healed with a cervical collar for 6 weeks. In the case of type 2 injuries, an additive injury of the cerebral nerves VII–XII should be considered. The difficulty of unstable fractures of type 3 can be seen in the not-rare appearance of an atlanto-occipital instability.
Diagnosis
With the routine use of the thin-slice CT, diagnosis is made more frequently. Although axial CT images are useful in assessing the presence of occipital condyle fractures, they do not usually enable visualization of the entire condyle (Fig. 15.1).
In the event of compression fractures, fragments can impinge into the foramen magnum. Sprain fractures can reach the region of the clivus and cause clinical symptomatic hemorrhage. Osseous tears of the condyles mainly impress saucer-type in the course of the Ligg. alaria, adjusted medio-caudally. In general, these injuries should be treated conservatively, even though distinctive atlanto-occipital instabilities are not accordable with life. For a reliable diagnostic apart from the axial, coronal slices of the thin-slice CT are particularly useful. The slice thickness should not exceed 1–2 mm. For ligmantous visualization, MRI is essential.
Therapy
The therapy of the above-described injuries should be decided with regard to the overall situation of the mostly severe injured patient. Unstable type 3 fractures require either an occipitocervical fusion or can be treated with immobilization via a halo fixator for 8–12 weeks. Complications include anterior luxations of a fractured condyle with dislocation around or into the foramen magnum. Aside from these rare complications, the prognosis of the OCF is rather good, although painful constrictions, especially of head joint function, can remain.
Ligamentic Instabilities of the Upper Cervical Spine
The traumatic ligamentic instabilities of the upper cervical spine are seldom seen and can be subdivided into four groups:
Occipitocervical dislocation
Translatoric atlantoaxial instability
Axial atlantoaxial instability
Rotatoric atlantoaxial instability
15.2.3.2 Atlanto-occipital Dislocations
Epidemiology
Atlanto-occipital dislocations are a rarity and represent profound and life-threatening injuries. In most cases, shearing motion in terms of translation is causative for these lesions. A rupture of the membrana tectoria is the consequence. High-energy trauma most often accounts for the mechanism of injury. A distraction with hyperextension and flexion is common, usually combined with a rotation component. Because of the relative ligamentous insufficiency in infancy and the additive horizontal course of the bearing area C0/C1, children are significantly more frequently affected. A second accumulation can be seen in pedestrians struck by a car.
Classification
According to Harris, there are three types of occipitocervical dislocations with regard to the direction of the head luxation [15] (Fig. 15.2):


Fig. 15.2
Atlanto-occipital dislocations according to Harris. (a) Type 1: Anterior dislocation – the most common form, unstable sagittal or combined sagittal and axial; (b) Type 2: Posterior dislocation – a rarity; (c) Type 3: Axial decompression – the most unstable form, global instability or complete separation of the head from the cervical spine
Type 1: Anterior dislocation – the most common form, unstable sagittal or combined sagittal and axial
Type 2: Posterior dislocation – a rarity
Type 3: Axial decompression – the most unstable form, global instability or complete separation of the head from the cervical spine
Diagnostics
Dislocation can often be seen in conventional X-ray images, but the CT scan is the gold standard, especially to detect additive injuries like condyle fractures, type 3 fractures according to Anderson and Montesano, or type 1 fractures of the dens. Functional images can be useful to evaluate ligamentous injuries, and MRI is useful here as well to show any neurological damage.
Several methods are described to quantify the spatial relationship between the occiput, atlas, and axis. The most common in the setting of trauma are the basion-dental interval (BDI) and the basion-posterior axial line interval (BAI), originally described by Harris et al. [15]. In their studies, Harris and colleagues measured the BAI and BDI on lateral radiographs of 400 healthy adults; the BAI and BDI did not exceed 12 mm in 98 %. Today, the BDI and BAI have come to be known as “Harris measurements,” or, more descriptively, as the “rule of twelve” (Fig. 15.3).
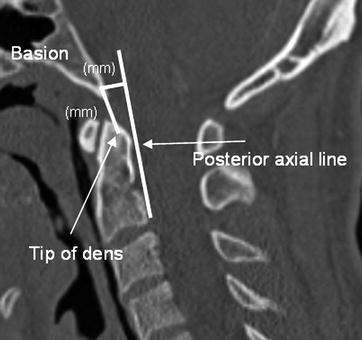
Fig. 15.3
Measurement technique for the BDI and BAIs. “Rule of the twelve” Harris measurement: The most inferior and posterior aspect of the basion is marked as well as the superior tip of the odontoid process (arrow). The distance between these two points (BDI) is measured in millimeters: a value >12 mm is highly suggestive of occipitoatlantal dissociation. A vertical line is drawn along the posterior vertebral border of the C2 body (arrow). This line should extend superiorly, just past the level of the foramen magnum. A perpendicular line is drawn from this line to the basion mark. This distance is then measured in millimeters (BAI). A value >12 mm should be considered indicative of an anterior occipitoatlantal dissociation
Ratio according to Powers: The line of the posterior border of the anterior arc of the atlas to the posterior border of the foramen magnum on the one hand or the posterior border of the pars basilaris to the anterior part of the posterior arc of the atlas (Fig. 15.4) can provide helpful information and lead to faster orientation.
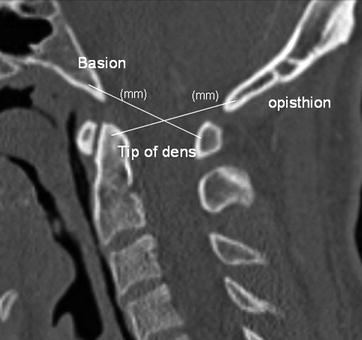
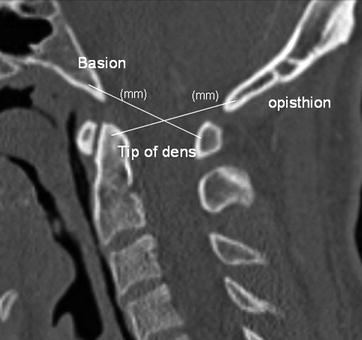
Fig. 15.4
Powers ratio
Functional examination under fluoroscopic guidance can discover hidden instabilities; again, a thin-slice CT scan is the standard, completed with 3-D reconstructions. Additionally, an MRI should be performed, when the patient has been stabilized, to diagnose a contusion of the medulla. Injured patients may show no or only marginal neurological symptoms, though the injury is highly unstable. Apart from osseous injuries, ligamentous lesions have a notable impact. In particular, the craniocervical ligaments (Membrana tinctoria, Lig. transversum, Lig. alarium and apicale) are of importance for the stability of the craniocervical transition zone [9], along with the epidural amplifying ligaments. The lateral craniocervical ligaments (Lig. nuchae, flavum, and the posterior and anterior atlanto-occipital ligament) have only a minor effect on stability, as does the atlantoaxial membrane [34]. In case of an atlanto-occipital dislocation (AOD), one or more ligaments are usually ruptured. Neurological symptoms are caused by traumatic lesions of the Medulla oblongata or the cranial nerves. As additive injuries, subarachnoid hematoma have been described [6], along with injuries of the A. carotis, A. vertebralis, and the anterior spinal artery. Therefore, an angio CT scan should be included in the diagnostic algorithm.
Therapy
Excessive traction should be avoided, especially during the primary treatment, as more dislocation can lead to iatrogenic neurological symptoms. The patient should be monitored during a reduction process. The maneuver starts with controlled traction and ends with axial compression to minimize dislocation or translation of the segment C0/C1 [26]. In case of an emergent therapy, a closed reduction with a temporary immobilization with a halo fixator, then a planned posterior spondylodesis with C0–C1/C2 (C3) should be performed. If the patient survives the injury, a loss of motility, measured up to 23° in the sagittal plane and 50° in rotation, can occur [18]. Intensive physiotherapy is essential for recovery of the function of the head joints after consolidation of the fractures (Fig. 15.5).
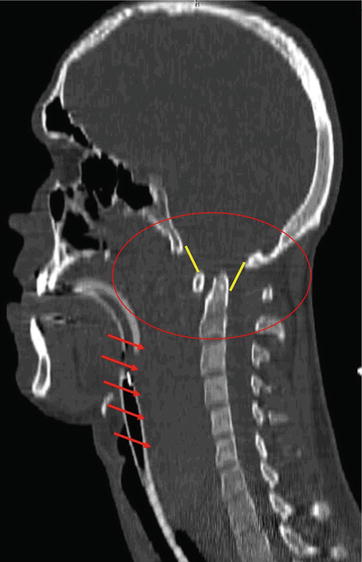
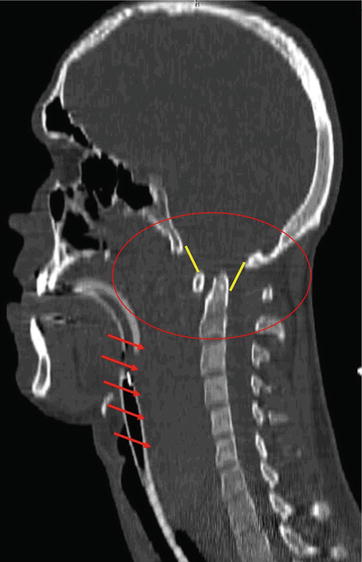
Fig. 15.5
Example of anterior dislocation: 22-year-old patient after car accident, death 3 h after accident. Note the soft tissue swelling (red arrows) and the reduced BDI (yellow line). The red oval shape marks the injury zone
Translatoric Atlantoaxial Instability
Epidemiology
Translatoric atlantoaxial injuries are seldom seen, as the Ligamentum atlantis brings more resistance towards the incoming forces than the Dens axis.
Classification
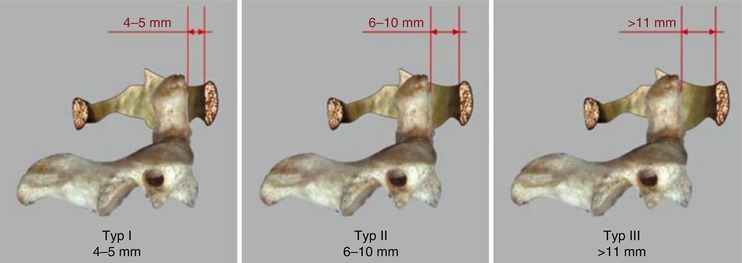
These injuries occur through a rupture or an osseous tear of the Lig. transversum atlantis [20] and are classified regarding to De la Caffinière [7] with consideration of the anterior atlantodental interval (AADI), with measurements normally up to 3 mm (Fig. 15.6).
Diagnostics
The instability can sometimes be seen in conventional X-rays, whereas osseous tears are detected by CT scan. Arbitrative for the diagnostic findings are the functional images, showing the ligamentic instability. Another helpful measurement technique is shown in Fig. 15.7.


Fig. 15.7
The ADI (atlanto dens interval, normal 3 mm) and the PADI (posterior atlanto dens interval, normal 12 mm): The craniocaudal midpoint of the anterior ring of C1 is marked. A line parallel to the ring of C1 is drawn from this point toward the odontoid process. The distance between the C1 mark and intersection with the anterior aspect of the odontoid process is measured in millimeters
Therapy
Differentiation between osseous tears and interligamentic ruptures is of importance in therapy. In the case of osseous tears, the grade of dislocation is crucial. For marginal dislocations with remaining osseous contact, conservative treatment can be chosen with a hard cervical collar for 6 weeks. Larger dislocations with only a poor chance of osseous reunion should be treated with atlantoaxial fusion, even in younger patients, as atlantoaxial instability and arthrosis can occur through a relative elongation. As the interligamentic ruptures also show no tendency for healing, atlantoaxial fusion is recommended.
Axial Atlantoaxial Instability
Epidemiology
Axial atlantoaxial instability is seldom seen. It occurs through axial translation between atlas and axis. A rupture of the atlantoaxial (Lig. supra- and intraspinale, Lig. flavum) and occipitocervical ligaments (Fasciculi longitudinalis, Ligg. alaria, Lig. apicis dentis) takes place. This injury is linked with occipitocervical instabilities.
Classification
The classification still is heterogeneous. Incomplete forms are distinguished from the complete form with or without translation [32].
Diagnostics
In conventional X-rays, the distinctive instability can be seen. The CT scan detects osseoligamentous tears. Again, functional images can prove the ligamentous injury using axial force. In the MRI, the ligamentous and neurological lesions can be seen.
Therapy
The therapy for atlantoaxial instabilities should be performed with a closed reduction with temporary fixation with a halo fixator, followed by definite therapy consisting of a occipitoatlantoaxial spondylodesis. Although initial images present dramatic pictures with the suspicion of disruption of neurological structures, patients mainly show only a few neurological symptoms.
Rotatoric Atlantoaxial Instability
Epidemiology
Traumatic rotatoric instabilities are seldom seen. A rotatoric instability occurs mainly through the interligamenteric rupture or a osseous tear of the Ligg. alaria. Pathophysiologically crucial is the ligamentic lesion between the condyle of the occiput and the dens axis, which permits an excessive rotation of occiput and atlas on the axis. Especially in children, a rotational atlantoaxial malposition, even without a rupture of the Ligg. alaria, can occur as an atlantoaxial subluxation.
Classification
According to Fielding and Hawkins [12], four types of rotational instability occur (Fig. 15.7):
Type I: Rotational instability with unilateral translation without ventral sliding of the atlas intact L. transversum.
Type II: Ventral and unilateral dislocation between C1 and C2, enlargement of the atlantodental distance 3–5 mm, possible rupture of the Lig. transversum in adults.
Type III: Atlantodental distance >5 mm, ruptured Lig. transversum, subluxation of both facet joints in the ventral direction.
Type IV: Rotational dislocation with shifting of the atlas in the dorsal direction in case of a destructed dens axis.
Diagnostics
Instability can sometimes be seen with the decentric located dens axis. The CT shows osseous tears of the ligaments as well as condyle fractures type 3 according to Anderson and Montesano or type-1 fractures of the dens. The MRI shows the ligamentic structures, though a functional assessment of the Lig. alaria is not possible. As conventional functional images, also in anteroposterior (a.p.) view, are difficult to interpret in this injury, functional rotational CT is recommended for the diagnosis of a rotational instability [3, 27]. In case of a deviation of the sides of more than 5°, a rupture of the Ligg. alaria can be assumed. Figure 15.8 shows the most recommended measurement technique [17, 22] (Fig. 15.9).
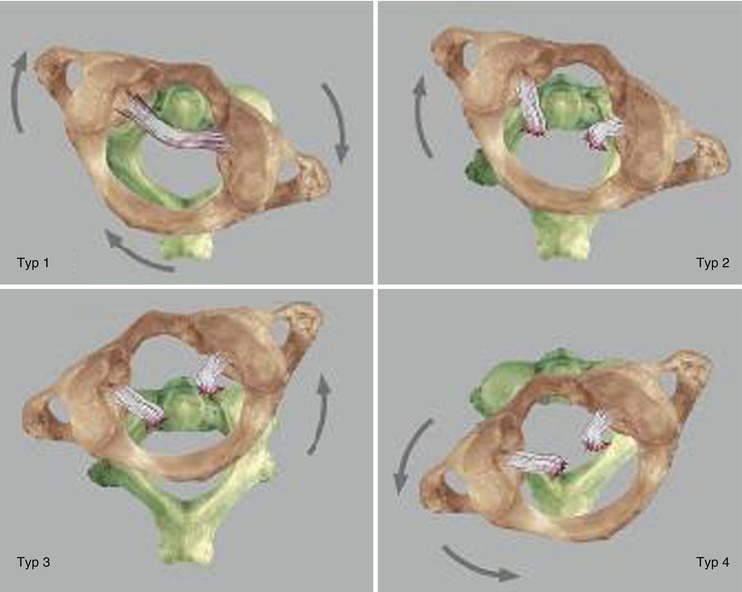
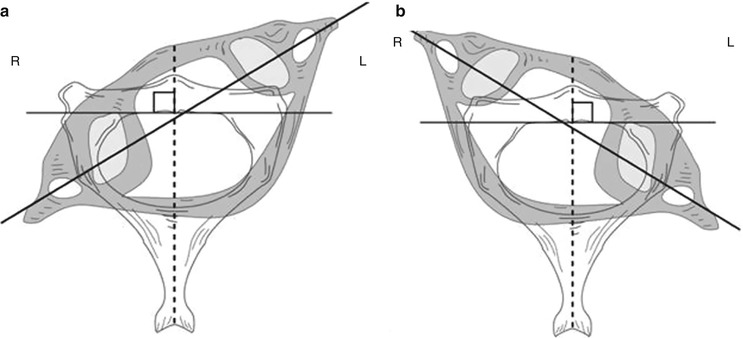
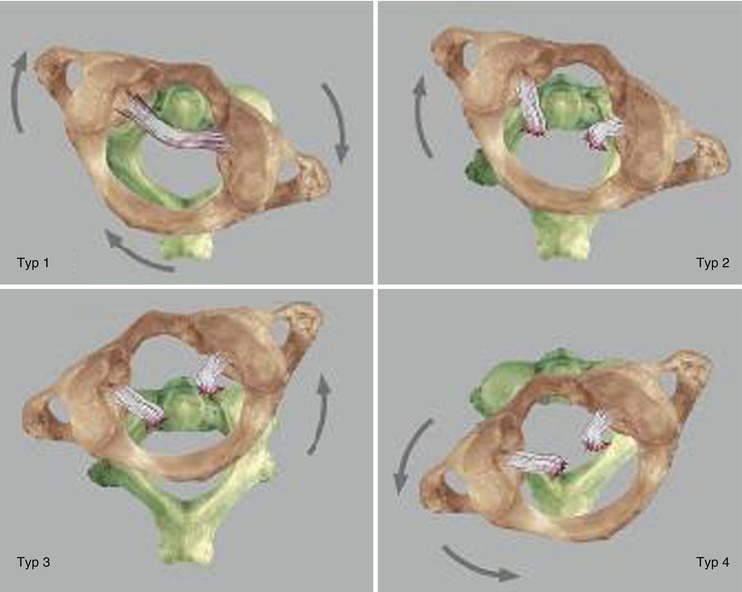
Fig. 15.8
Rotational instability
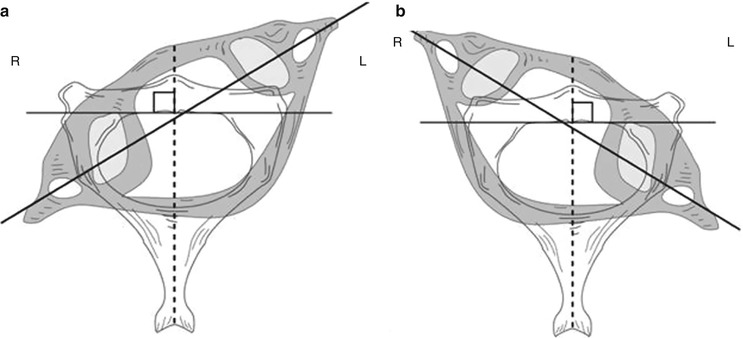
Fig. 15.9
Measurement of right (R) (a) and left (L) (b) atlantoaxial rotation. For optimal measuring, the CT gantry angle should be aligned along the transverse plane of the upper cervical vertebrae. An axial CT slice at the level of the C2 body and C1 ring are then obtained. An anteroposterior line is drawn from the midpoint of the C2 body to the center of the spinous process. A line perpendicular to this line is drawn along the posterior C2 vertebral body. On the best axial slice of C1, the midpoints of the transverse (vertebral artery) foramens are marked, and a line is drawn between them. The angulation between these two lines represents the degree of static atlantoaxial rotatory deformity (subluxation). By convention, the side (right or left) toward which the atlas (head) points is considered the side of the rotation [5]
Therapy
These fractures occur through rotation of the axis adverse the atlas around the longitude axle of the body and are more frequent in children. As a sufficient healing with conservative treatment cannot be expected [4], the therapy results in a spondylodesis C1/C2, in general from posterior. In the case of type-III lesions with ruptured Lig. transversum, a posterior stabilization C1/C2, for example, according to Magerl, should be chosen. Finally, it is important to underline the possibility of an iatrogenic vertical dissociation through tension during the reduction process.
15.2.3.3 Atlas Fractures
Epidemiology
Fractures of C1 seldom occur but are more frequent than the above-mentioned injuries. In the literature, the incidence amounts to 2–13 % of all cervical and 1.3 % of all spine injuries [29]. The Jefferson fracture only represents 2 % of all cervical spine injuries, though it accounts for two-thirds of the atlas fractures [14].
Classification
Jefferson distinguished four different fracture types in 1920:
Type I: Isolated bow fractures
Type II: Combined fractures of the anterior and posterior atlas bow
Type III: Fracture of the massa lateralis
Type IV: Fracture of the processus transversus
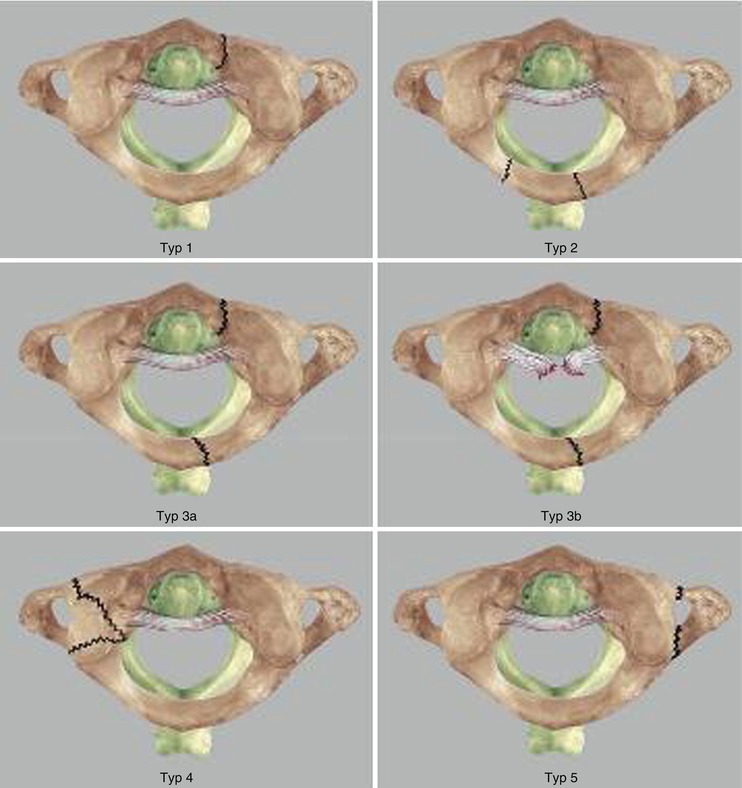
Today, the classification according to Gehweiler has proved its value:
Type I: Isolated fractures of the anterior atlas bow
Type II: Isolated fractures of the posterior atlas bow
Type III: Combined fracture of the anterior and posterior atlas bow (Jefferson fracture)
Type IV: Isolated fractures of the massa lateralis
Type V: Fracture of the processus transversus (Fig. 15.10)