Cervical Spine
Examination of the cervical spine involves determining whether the injury or pathology occurs in the cervical spine or in a portion of the upper limb. Cyriax1 called this assessment the scanning examination. In the initial assessment of a patient who complains of pain in the neck and/or upper limb, this procedure is always carried out unless the examiner is absolutely sure of the location of the lesion. If the injury is in the neck, the scanning examination is definitely called for to rule out neurological involvement. After the lesion site has been determined, a more detailed assessment of the affected area is performed if it is outside the cervical spine.
Because many conditions affecting the cervical spine can be manifested in other parts of the body, the cervical spine is a complicated area to assess properly, and adequate time must be allowed to ensure that as many causes or problems are examined as possible.
Applied Anatomy
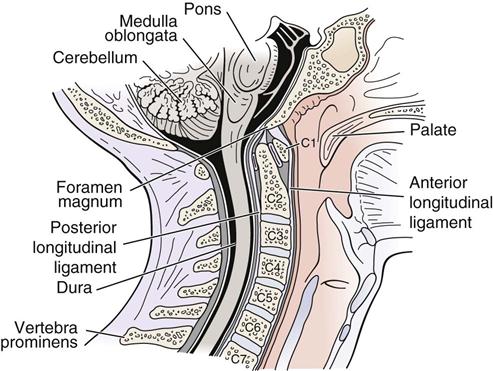
The cervical spine consists of several pairs of joints. It is an area in which stability has been sacrificed for mobility, making the cervical spine particularly vulnerable to injury because it sits between a heavy head and a stable thoracic spine and ribs. The cervical spine is divided into two areas—the cervicoencephalic for the upper cervical spine and the cervicobrachial for the lower cervical spine. The cervicoencephalic or cervicocranial region (C0 to C2) shows the relationship between the cervical spine and the occiput, and injuries in this region have the potential of involving the brain, brainstem, and spinal cord (Figure 3-1).2,3 Injuries in this area lead to symptoms of headache, fatigue, vertigo, poor concentration, hypertonia of sympathetic nervous system, and irritability. In addition, there may be cognitive dysfunction, cranial nerve dysfunction, and sympathetic system dysfunction.2,3
The atlanto-occipital joints (C0 to C1) are the two uppermost joints. The principal motion of these two joints is flexion-extension (15° to 20°), or nodding of the head. Side flexion is approximately 10°, whereas rotation is negligible. The atlas (C1) has no vertebral body as such. During development, the vertebral body of C1 evolves into the odontoid process, which is part of C2. The atlanto-occipital joints are ellipsoid and act in unison. Along with the atlanto-axial joints, these joints are the most complex articulations of the axial skeleton.
There are several ligaments that stabilize the atlanto-occipital joints. Anteriorly and posteriorly are the atlanto-occipital membranes. The anterior membrane is strengthened by the anterior longitudinal ligament. The posterior membrane replaces the ligamentum flavum between the atlas and occiput. The tectorial membrane, which is a broad band covering the dens and its ligaments, is found within the vertebral canal and is a continuation of the posterior longitudinal ligament. The alar ligaments are two strong rounded cords found on each side of the upper dens passing upwards and laterally to attach on the medial sides of the occipital condyles. The alar ligaments limit flexion and rotation and play a major role in stabilizing C1 and C2, especially in rotation.4
The atlanto-axial joints (C1 to C2) constitute the most mobile articulations of the spine. Flexion-extension is approximately 10°, and side flexion is approximately 5°. Rotation, which is approximately 50°, is the primary movement of these joints. With rotation, there is a decrease in height of the cervical spine at this level as the vertebrae approximate because of the shape of the facet joints. The odontoid process of C2 acts as a pivot point for the rotation. This middle, or median, joint is classified as a pivot (trochoidal) joint. The lateral atlanto-axial, or facet, joints are classified as plane joints. Generally, if a person can talk and chew, there is probably some motion occurring at C1 to C2. At the atlanto-axial joints, the main supporting ligament is the transverse ligament of the atlas, which holds the dens of the axis against the anterior arch of the atlas. It is this ligament that weakens or ruptures in rheumatoid arthritis. As the ligament crosses the dens, there are two projections off the ligament, one going superiorly to the occiput and one inferiorly to the axis. The ligament and the projections form a cross, and the three parts taken together are called the cruciform ligament of the atlas (Figure 3-2).
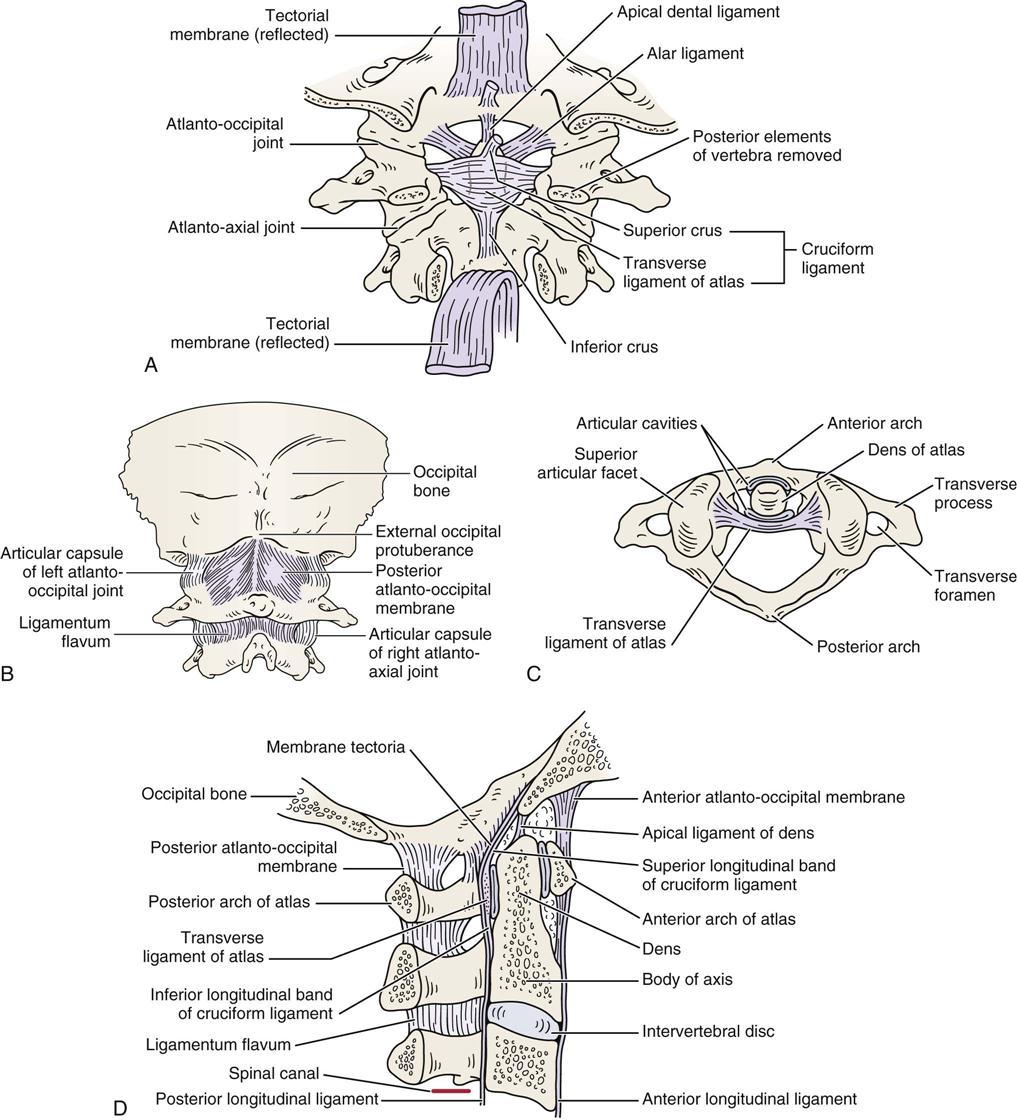
A, Posterior deep view. B, Posterior superficial view. C, Superior view. D, Lateral view.
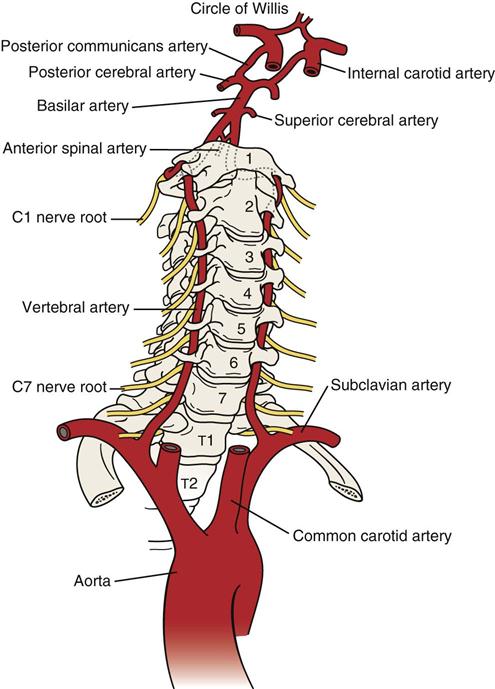
The vertebral artery—part of the vertebrobasilar system that passes through the transverse processes of the cervical vertebrae usually starting at C6 but entering as high as C4—supplies 20% of the blood supply to the brain (primarily the hindbrain) along with the internal carotid artery (80%) (Figure 3-3).5,6 In its path, the vertebral artery lies close to the facet joints and vertebral body where it may be compressed by osteophyte formation or injury to the facet joint. In addition, in older individuals, atherosclerotic changes and other vascular risk factors (e.g., hypertension, high fat or cholesterol levels, diabetes, smoking) may contribute to altered blood flow in the arteries.7 The vertebral and internal carotid arteries are stressed primarily by rotation, extension, and traction movements, but other movements may also stretch the artery.8–10 Rotation and extension of as little as 20° have been shown to significantly decrease vertebral artery blood flow.11,12 The greatest stresses are placed on the vertebral arteries in four places: where it enters the transverse process of C6, within the bony canals of the vertebral transverse processes, between C1 and C2, and between C1 and the entry of the arteries into the skull.13,14 These latter two areas have the greatest potential for problems (e.g., thrombosis, dissection, stroke) related to treatment and their concomitant stress on the vertebral arteries.15 Dutton13 reports that the most common mechanism for non-penetrating injury to the vertebral artery is neck extension, with or without side flexion or rotation.16,17 Given the type of injury possible, symptoms may be delayed.18,19 Symptoms related to the vertebral artery include vertigo, nausea, tinnitus, “drop attacks” (falling without fainting), visual disturbances, or, in rare cases, stroke or death.
The lower cervical spine (C3 to C7) is called the cervicobrachial area, since pain in this area is commonly referred into the upper extremity.2,3 Pathology in this region leads to neck pain alone, arm pain alone, or both neck and arm pain. Thus, symptoms include neck and/or arm pain, headaches, restricted range of motion (ROM), paresthesia, altered myotomes and dermatomes, and radicular signs. Cognitive dysfunction and cranial nerve dysfunction are not commonly symptoms of injuries in this area although sympathetic dysfunction may be. Injury to both areas, if severe enough, may result in psychosocial issues.
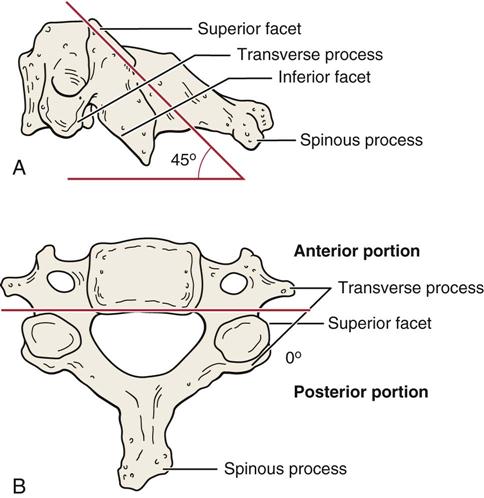
There are 14 facet (apophyseal) joints in the cervical spine (C1 to C7). The upper four facet joints in the two upper thoracic vertebrae (T1 to T2) are often included in the examination of the cervical spine. The superior facets of the cervical spine face upward, backward, and medially; the inferior facets face downward, forward, and laterally (Figure 3-4). This plane facilitates flexion and extension, but it prevents simple rotation or side flexion without both occurring to some degree together. This is called a coupled movement with rotation and side flexion both occurring with either movement.20 Ishii et al.21,22 reported that between C0 and C2, as well as C7 and T1, the two movements occur in opposite directions while between C2 and C7, they occur in the same direction. These joints move primarily by gliding and are classified as synovial (diarthrodial) joints. The capsules are lax to allow sufficient movement. At the same time, they provide support and a check-rein type of restriction at end range. The greatest flexion-extension of the facet joints occurs between C5 and C6; however, there is almost as much movement at C4 to C5 and C6 to C7. Because of this mobility, degeneration is more likely to be seen at these levels. The neutral or resting position of the cervical spine is slightly extended. The close packed position of the facet joints is complete extension.
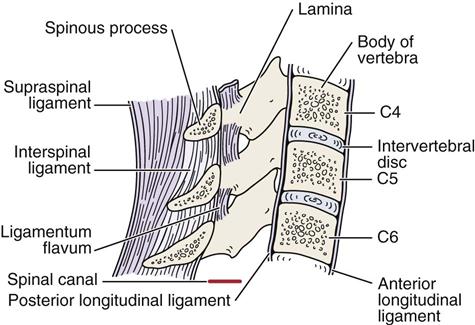
The recurrent meningeal, or sinuvertebral, nerve innervates the anterior dura sac, the posterior annulus fibrosus, and the posterior longitudinal ligament. The facet joints are innervated by the medial branch of the dorsal primary rami.23 For C3 to C7, the main ligaments are the anterior longitudinal ligament, the posterior longitudinal ligament, the ligamentum flavum, and the supraspinal and interspinal ligaments (Figure 3-5). There are also ligaments between the transverse processes (intertransverse ligaments), but in the cervical spine, they are rudimentary.
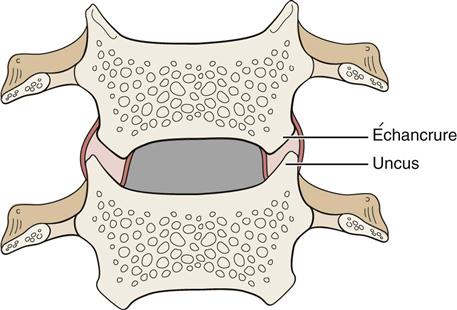
Some anatomists24–27 refer to the costal or uncovertebral processes as uncinate joints or joints of Luschka (Figure 3-6). These structures were described by von Luschka in 1858. The uncus gives a “saddle” form to the upper aspect of the cervical vertebra, which is more pronounced posterolaterally; it has the effect of limiting side flexion. Extending from the uncus is a “joint” that appears to form because of a weakness in the annulus fibrosus. The portion of the vertebra above, which “articulates” or conforms to the uncus, is called the échancrure, or notch. Notches are found from C3 to T1, but according to most authors,24–27 they are not seen until age 6 to 9 years and are not fully developed until 18 years of age. There is some controversy as to whether they should be classified as real joints because some authors believe they are the result of degeneration of the intervertebral disc.
The intervertebral discs make up approximately 25% of the height of the cervical spine. No disc is found between the atlas and the occiput (C0 to C1) or between the atlas and the axis (C1 to C2). It is the discs rather than the vertebrae that give the cervical spine its lordotic shape (Figure 3-7). The nucleus pulposus functions as a buffer to axial compression in distributing compressive forces, whereas the annulus fibrosus acts to withstand tension within the disc. The intervertebral disc has some innervation on the periphery of the annulus fibrosus.28,29
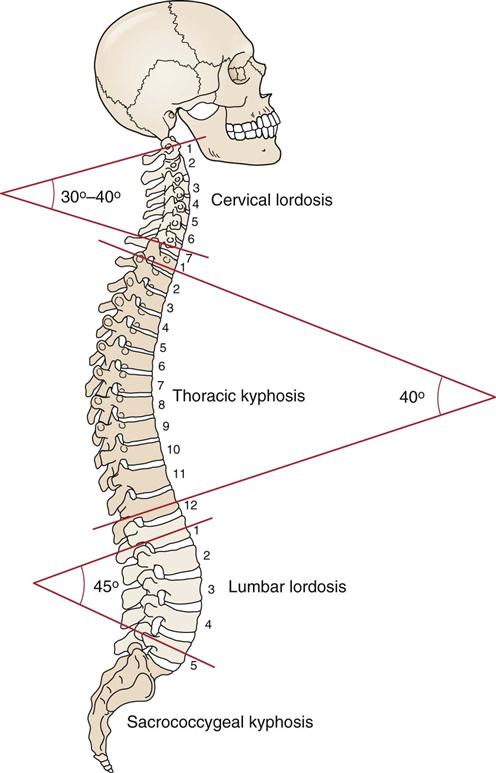
The curvatures represent the normal resting postures of the region. (Modified from Neumann DA: Kinesiology of the musculoskeletal system—foundations for physical rehabilitation, St Louis, 2002, Mosby, p. 276.)
There are seven vertebrae in the cervical spine with the body of each vertebra (except C1) supporting the weight of those above it. The facet joints may bear some of the weight of the vertebrae above, but this weight is minimal if the normal lordotic posture is maintained. However, even this slight amount of weight bearing can lead to spondylitic changes in these joints. The outer ring of the vertebral body is made of cortical bone, and the inner part is made of cancellous bone covered with the cartilaginous end plate. The vertebral arch protects the spinal cord, while the spinous processes, most of which are bifid in the cervical spine, provide for attachment of muscles. The transverse processes have basically the same function. In the cervical spine, the transverse processes are made up of two parts: the anterior portion that provides the foramen for the vertebral body, and the posterior portion containing the two articular facets (see Figure 3-4, B). In the cervical spine, the spinous processes are at the level of the facet joints of the same vertebra. Generally, the spinous process is considered to be absent or at least rudimentary on C1. This is why the first palpable vertebra descending from the external occiput protuberance is the spinous process of C2.
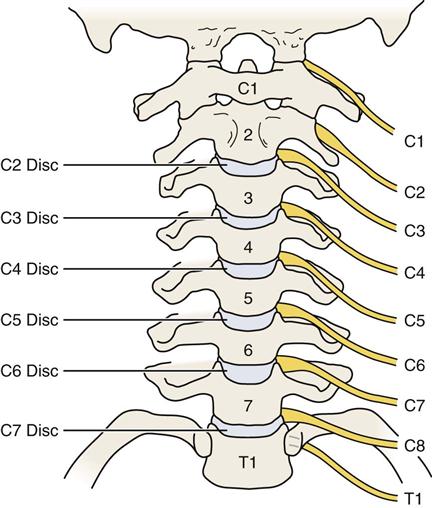
Although there are seven cervical vertebrae, there are eight cervical nerve roots. This difference occurs because there is a nerve root exiting between the occiput and C1 that is designated the C1 nerve root. In the cervical spine, each nerve root is named for the vertebra below it. As an example, C5 nerve root exists between the C4 and C5 vertebrae (Figure 3-8). In the rest of the spine, each nerve root is named for the vertebra above; the L4 nerve root, for example, exists between the L4 and L5 vertebrae. The switch in naming of the nerve roots from the one below to the one above is made between the C7 and T1 vertebrae. The nerve root between these two vertebrae is called C8, accounting for the fact that there are eight cervical nerve roots and only seven cervical vertebrae.
Patient History
In addition to the questions listed under Patient History in Chapter 1, the examiner should obtain the following information from the patient:
1. What is the patient’s age? Spondylosis (also called spondylosis deformans) is often seen in persons 25 years of age or older, and it is present in 60% of those older than 45 years and 85% of those older than 65 years of age.30,31 It is a generalized disease of aging initiated by intervertebral disc degeneration. Symptoms of osteoarthritis do not usually appear until a person is 60 years of age or older (Table 3-1).
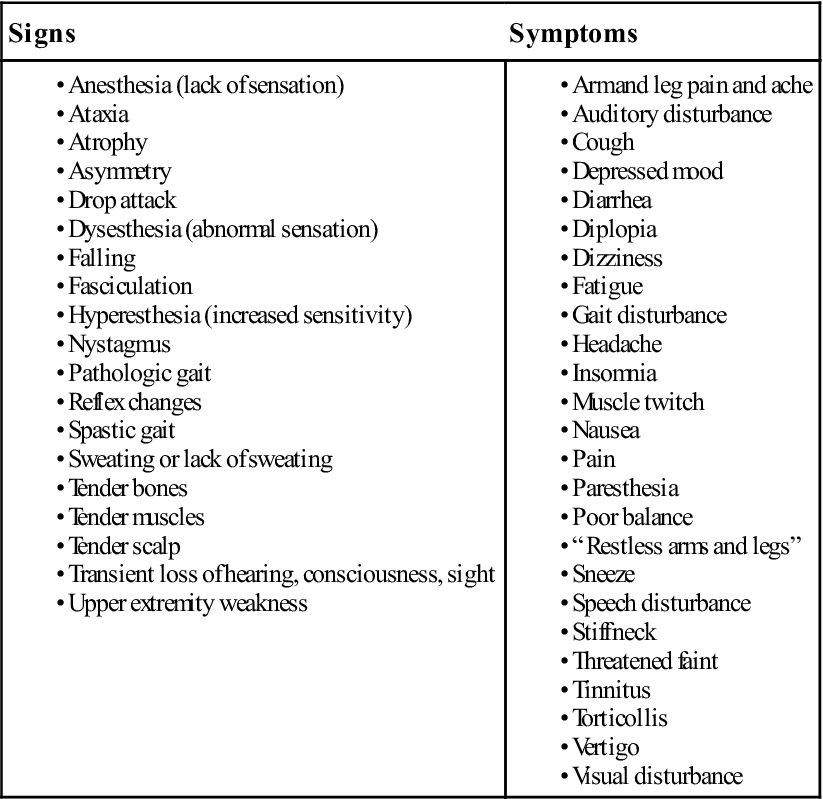
2. What are the symptoms, and which are most severe? Table 3-2 outlines many of the signs and symptoms that may arise from cervical spine pathology.32 Where are the symptoms most severe—in the neck, the shoulder, above or below the elbow, in the hands, and/or fingers?33 Location of the symptoms may help determine what level of the cervical spine is involved (e.g., tingling in the middle finger may indicate a problem at C6 to C7). Are the symptoms constant, intermittent or variable?33 The Bone and Joint Decade 2000–2010 Task Force on Neck Pain and its Associated Disorders recommended that neck pain sufferers be divided into four groups (Table 3-3).34
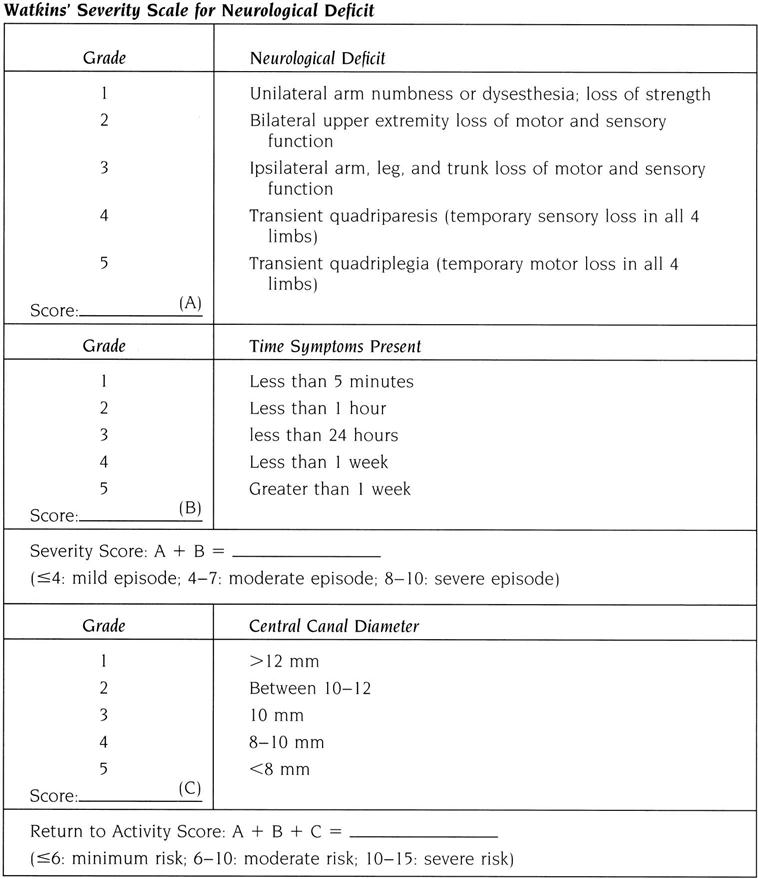
Watkins35 provided a severity scale for neurological injury in football that can be used as a guideline for injury severity involving the cervical spine, especially if one is contemplating allowing the patient to return to activity (Figure 3-9 ). A combined score (A+B) of 4 is considered a mild episode, 4 to 7 is a moderate episode, and 8 to 10 is a severe episode. This scale can be combined with radiologic information on canal size (score C) to give a general determination of the possibility of symptoms returning if the patient returns to activity. In this case, a score of 6 (A+B+C) indicates minimum risk, 6 to 10 is moderate risk, and 10 to 15 is severe risk. Watkins35 also points out that extenuating factors (such as, age of patient, level of activity, and risk) versus benefit, also play a role and, although not included in the score, must be considered. Table 3-4 outlines some of the factors that increase the chances of recovery from neck pain. Chronic post whiplash syndrome can lead to anxiety, pain catastrophizing (negative or heightened orientation toward pain), and other adverse psychosocial factors over time, and it can play a major role in the symptoms felt by the patient.36 Table 3-5 outlines yellow flags related to fear-avoidance beliefs.
3. What was the mechanism of injury? Was trauma, stretching, or overuse involved? Was the patient moving when the injury occurred? Table 3-6 outlines warning signs and symptoms (red flags) of serious cervical spine disorders. These questions help determine the type and severity of injury. For example, trauma may cause a whiplash-type (acceleration) injury or whiplash associated disorder (WAD) (Table 3-7),37 stretching may lead to “burners,” overuse or sustained postures may result in thoracic outlet symptoms, and a report of an insidious onset in someone older than 55 years of age may indicate cervical spondylosis. Was the patient hit from the side, front, or behind? Did the patient see the accident coming?38 “Burners” or “stingers” typically occur from a blow to part of the brachial plexus or from stretching or compression of the brachial plexus (Table 3-8; Figure 3-10). The answers to these questions help the examiner determine how the injury occurred, the tissues injured, and the severity of the injuries.
4. Has the patient had neck pain before? Table 3-9 outlines factors that decrease chances of a new episode of neck pain.34
5. What is the patient’s usual activity or pastime? Do any particular activities or postures bother the patient? What type of work does the patient do? Are there any positions that the patient holds for long periods (e.g., when sewing, typing, or working at a desk)? Does the patient wear glasses? If so, are they bifocals or trifocals? Upper cervical symptoms may result from excessive nodding as the patient tries to focus through the correct part of the glasses. Cervicothoracic (lower cervical/upper thoracic spine) joint problems are often painful when activities that require push-and-pull motion (such as, lawn mowing, sawing, and cleaning windows) are performed. What movements bother the patient? For example, extension can aggravate symptoms in patients with radicular signs and symptoms.39
6. Did the head strike anything, or did the patient lose consciousness? If the injury was caused by a motor vehicle accident, it is important to know whether the patient was wearing a seat belt, the type of seat belt (lap or shoulder), and whether the patient saw the accident coming. These questions give some idea of the severity and mechanisms of injury. If the patient was unconscious or unsteady, the character of each episode of altered consciousness should be noted (see Chapter 2).
7. Did the symptoms come on right away? Bone pain usually occurs immediately, but muscle or ligamentous pain can either come on immediately (e.g., a tear) or occur several hours or days later (e.g., stretching caused by a motor vehicle accident). Seventy percent of whiplash patients reported immediate symptom occurrence while the rest reported delayed symptoms.32,40–44 How long have the symptoms been present? Myofascial pain syndromes demonstrate generalized aching and at least three trigger points, which have lasted for at least 3 months with no history of trauma.45
8. What are the sites and boundaries of the pain? Have the patient point to the location or locations of the pain. Symptoms do not go down the arm for a C4 nerve root injury or for nerve roots above that level. Cervical radiculopathy, or injury to the nerve roots in the cervical spine, presents primarily with unilateral motor and sensory symptoms into the upper limb, with muscle weakness (myotome), sensory alteration (dermatome), reflex hypoactivity, and sometimes focal activity being the primary signs.46–49 Acute radiculopathies are commonly associated with disc herniations, whereas chronic types are more related to spondylosis.47 Disc herniations in the cervical spine commonly cause severe neck pain that may radiate into the shoulder, scapula and/or arm, limit ROM, and an increase in pain on coughing, sneezing, jarring, or straining.44 Cervical myelopathy, or injury to the spinal cord itself, is more likely to present with spastic weakness, paresthesia, and possible incoordination in one or both lower limbs, as well as proprioceptive and/or sphincter dysfunction (Tables 3-10 and 3-11).50
9. Is there any radiation of pain? It is helpful to correlate this answer with dermatome and sensory peripheral nerve findings when performing sensation testing and palpation later in the examination. Is the pain deep, superficial, shooting, burning, or aching? For example, when an athlete experiences a “burner,” the sensation is a lightning-like, burning pain into the shoulder and arm, followed by a period of heaviness or loss of function in the arm. Figure 3-11 shows the radiation of pain with facet (apophyseal) joint pathology.51
11. Does the patient have any headaches? If so, where? How frequently do they occur? For example, do they occur every day, two times per day, two days per week, or one day per month?52 How intense are they? How long do they last? Are they affected by medication and, if so, by how much medication, and what kind? Are there any precipitating factors (e.g., food, stress, posture)? See Tables 2-11, 2-12, and 2-13, which indicate the influence of time of day, body position, headache location, and type of pain on diagnosis of the type of headache that the patient may have. Table 2-14 outlines the salient features of some of the more common headaches. Craniovertebral joint dysfunction commonly is accompanied by headaches. For example, C1 headaches occur at the base and top of the head, whereas C2 headaches are referred to the temporal area.
12. Does a position change alter the headache or pain? If so, which positions increase or decrease the pain? The patient may state that the pain and referred symptoms are decreased or relieved by placing the hand or arm of the affected side on top of the head. This is called Bakody’s sign, and it is usually indicative of problems in the C4 or C5 area.53,54
13. Is paresthesia (a “pins and needles” feeling) present? This sensation occurs if pressure is applied to the nerve root. It may become evident if pressure is relieved from a nerve trunk. Numbness and/or paresthesia in the hands or legs and deteriorating hand function all may relate to cervical myelopathy (see Table 3-10).
15. Are there any lower limb symptoms? This finding may indicate a severe problem affecting the spinal cord (myelopathy; see Table 3-10). These symptoms may include numbness, paresthesia, stumbling, difficulty walking, and lack of balance or agility. All of these symptoms could indicate cervical myelopathy. Likewise, signs of sphincter (bowel or bladder) or sexual dysfunction may be related to cervical myelopathy.
16. Does the patient have any difficulty walking? Does the patient have problems with balance? Does the patient stumble when walking, have trouble walking in the dark, or walk with feet wide apart? Positive responses may indicate a cervical myelopathy. Abnormality of the cranial nerves combined with gait alterations may indicate systemic neurological dysfunction.55
17. Does the patient experience dizziness, faintness, or seizures? What is the degree, frequency, and duration of the dizziness? Is it associated with certain head positions or body positions? Semicircular canal problems or vertebral artery problems (Table 3-12) can lead to dizziness. Dizziness from a vertebral artery problem is commonly associated with other symptoms. Falling with no provocation while remaining conscious is sometimes called a drop attack.56 Has the patient experienced any visual disturbances? Disturbances such as diplopia (double vision), nystagmus (“dancing eyes”), scotomas (depressed visual field), and loss of acuity may indicate severity of injury, neurological injury, and sometimes increased intracranial pressure (see Chapter 2).53
18. Does the patient exhibit or complain of any sympathetic symptoms? There may be injury to the cranial nerves or the sympathetic nervous system, which lies in the soft tissues of the neck anterior and lateral to the cervical vertebrae. The cranial nerves and their functions are shown in Table 2-1. Severe injuries (e.g., acceleration/whiplash type) can lead to hypertonia of the sympathetic nervous system.2 Some of the sympathetic signs and symptoms the examiner may elicit are “ringing” in the ears (tinnitus), dizziness, blurred vision, photophobia, rhinorrhea, sweating, lacrimation, and loss of strength.
25. Does the patient display any cognitive dysfunction? If a possible head injury is suspected, the clinician should also consider testing for mental status (see Chapter 2).
TABLE 3-1
Differential Diagnosis of Cervical Spondylosis, Spinal Stenosis, and Disc Herniation
| Cervical Spondylosis | Cervical Spinal Stenosis | Cervical Disc Herniation* | |
| Pain | Unilateral | May be unilateral or bilateral | May be unilateral (most common) or bilateral |
| Distribution of pain | Into affected dermatomes | Usually several dermatomes affected | Into affected dermatomes |
| Pain on extension | Increases | Increases | May increase (most common) |
| Pain on flexion | Decreases | Decreases | May increase or decrease (most common) |
| Pain relieved by rest | No | Yes | No |
| Age group affected | 60% of those older than 45 years 85% of those older than 65 years | 11 to 70 years Most common: 30 to 60 years | 17 to 60 years |
| Instability | Possible | No | No |
| Levels commonly affected | C5–C6, C6–C7 | Varies | C5–C6 |
| Onset | Slow | Slow (may be combined with spondylosis or disc herniation) | Sudden |
| Diagnostic imaging | Diagnostic | Diagnostic | Diagnostic (be sure clinical signs support) |
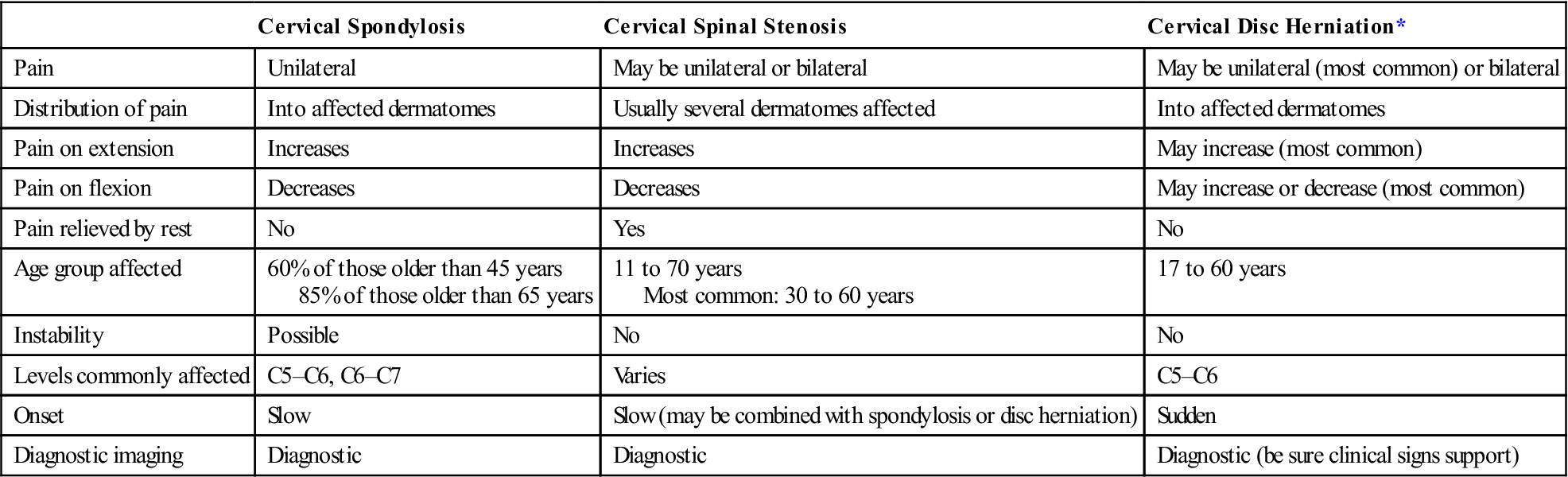
TABLE 3-2
Signs and Symptoms Arising from Cervical Spine Pathology
| Signs | Symptoms |
Modified from Bland JH: Disorders of the cervical spine, Philadelphia, 1994, W.B. Saunders Co., p. 161.
TABLE 3-3
Grading of Patients Suffering from Neck Pain
| Grade | Clinical Presentation |
| 1 | No signs of major pathology |
| Little or no interference with daily activity (ADL) | |
| 2 | No signs of major pathology |
| Interference with daily activity (ADL) | |
| 3 | Pain with neurological signs of nerve compression (radiculopathy) |
| 4 | Signs of major pathology (e.g., instability, infection) |
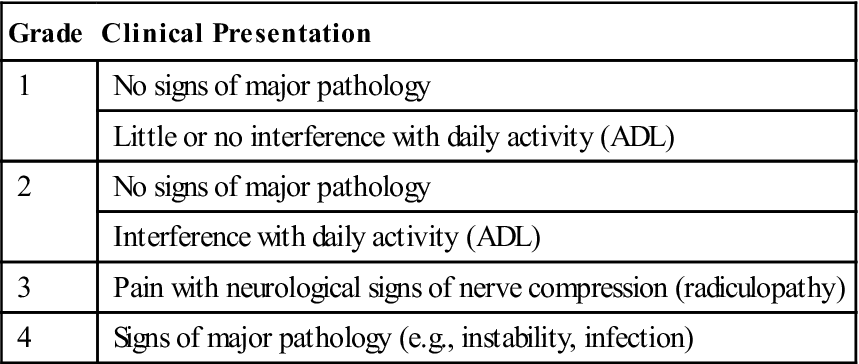
ADL, Activity of daily living.
Adapted from Guzman J, Haldeman S, Carroll LJ, et al: Clinical practice implications of the Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders: from concepts and findings to recommendations. J Manipulative Physiol Ther 32(2 Suppl):235, 2009.
TABLE 3-4
Factors That Increase Chances of Recovery from an Episode of Neck Pain
| Scenario and Grade of Neck Pain | Likely Increase | Might Increase | No Effect | Not Enough Evidence to Make Determination |
| General population | Younger age, no previous neck pain, good physical and psychological health, good coping, good social support | Being employed | — | Gender, general exercise or fitness prior to pain episode, cervical disc changes |
| At work | Exercise and sports, no prior pain or prior sick leave | Changing jobs (for certain job types), white collar job, greater influence over work | Age, ergonomics/ physical job demands, work-related psychosocial factors (but many such factors not studied) | Gender, compensation, litigation, obesity, smoking, cervical disc changes |
| After a traffic collision | No prior pain or sick leave, fewer initial symptoms, less symptom severity, Grade I WAD, good psychological health (e.g., not coping passively, no fear of movement, no post-injury anxiety), no early “overtreatment” | No prior pain problems, good prior health, non-tort insurance, no lawyer involvement, lower collision speed | Collision specific factors (such as, head position when struck, position in vehicle, direction of collision) | Age, gender, culture, prior physical fitness, cervical disc changes |
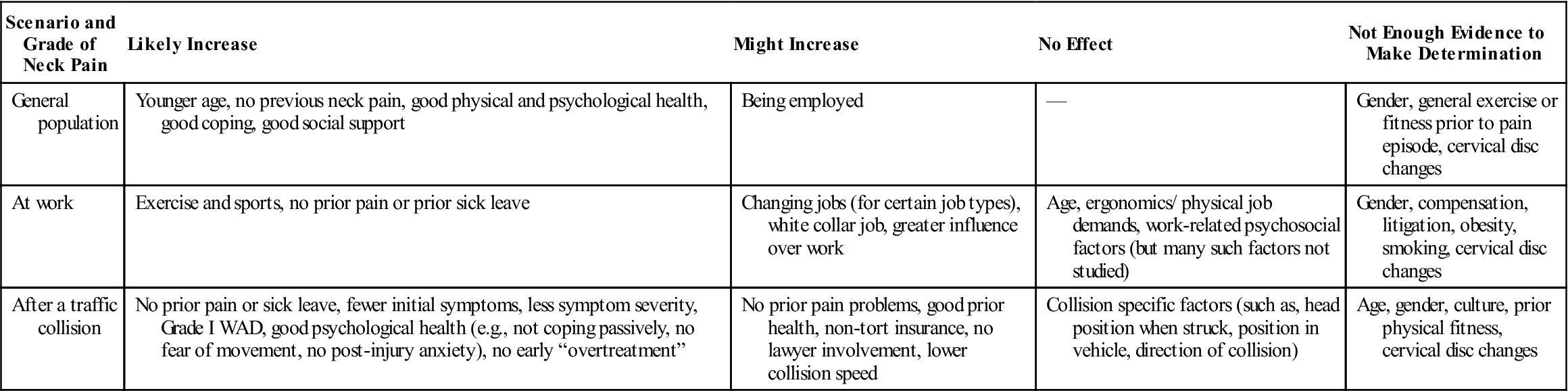
WAD, Whiplash-associated disorder.
From Guzman J, Haldeman S, Carroll LJ, et al: Clinical practice implications of the Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders: from concepts and findings to recommendations. J Manipulative Physiol Ther 32(2 Suppl):234, 2009.
![]() TABLE 3-5
TABLE 3-5
Clinical Yellow Flags Indicating Heightened Fear-Avoidance Beliefs
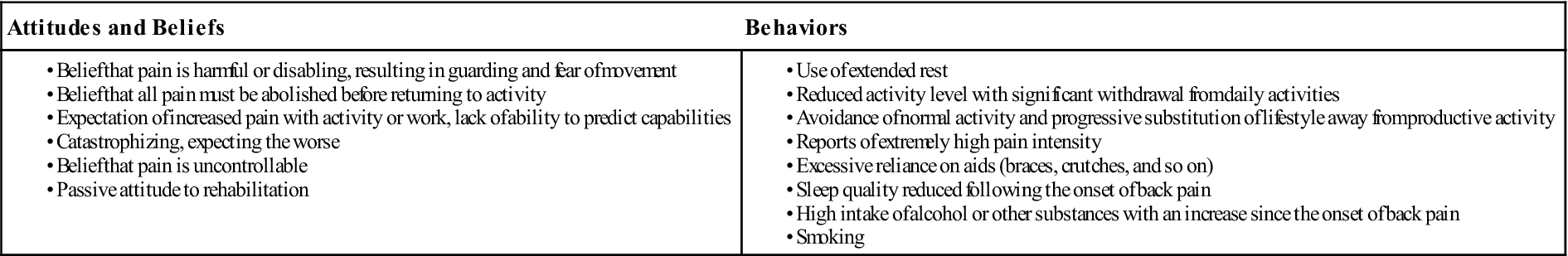
From Childs JD, Fritz JM, Piva SR, et al: Proposal of a classification system for patients with neck pain. J Orthop Sports Phys Ther 34:686–700, 2004. Data from Kendall, et al: Guide to assessing psychosocial yellow flags in acute low back pain: risk factors for long-term disability and work loss, Wellington, New Zealand, 2002, Accident Rehabilitation and Compensation Insurance Corporation of New Zealand and the National Health Committee.
![]() TABLE 3-6
TABLE 3-6
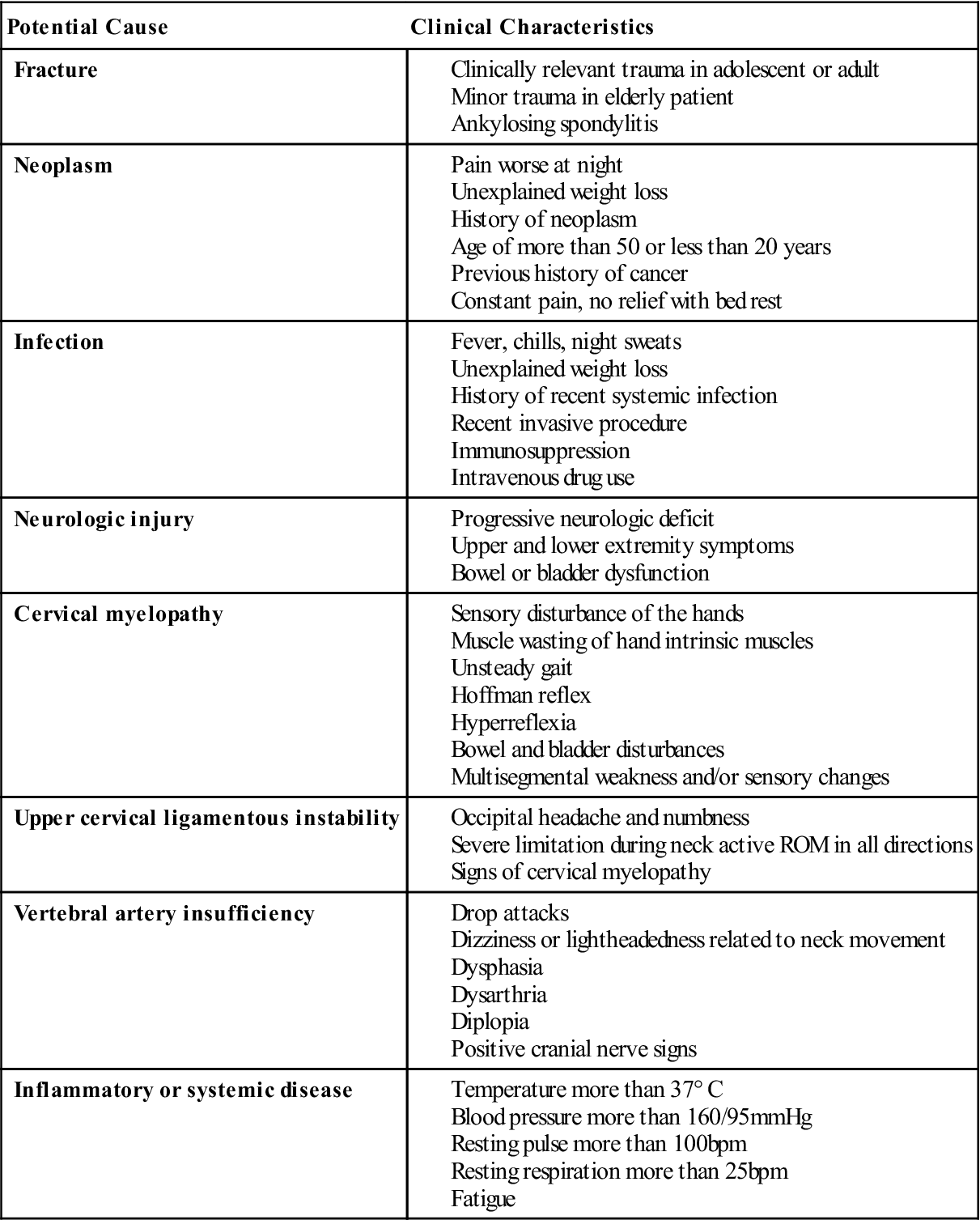
Modified from Rao RD, Currier BL, Albert TJ, et al: Degenerative cervical spondylosis: clinical syndromes, pathogenesis, and management. J Bone Joint Surg Am 89(6):1360–1378, 2007; Childs JD, Fritz JM, Piva SR, et al: Proposal of a classification system for patients with neck pain. J Orthop Sports Phys Ther 34:688, 2004.
TABLE 3-7
The Quebec Severity Classification of Whiplash Associated Disorders
| Grade | Clinical Presentation |
| 0 | No neck symptoms, no physical sign(s) |
| 1 | No physical sign(s); neck pain; stiffness or tenderness only; neck complaints predominate; normal ROM; normal reflexes, dermatomes, and myotomes |
| 2 | Neck symptoms (pain, stiffness) and musculoskeletal sign(s)—such as, decreased ROM and point tenderness; soft tissue complaints (pain, stiffness) into shoulders and back; normal reflexes, dermatomes, and myotomes |
| 3 | Neck symptoms (pain, stiffness, restricted ROM) and neurological sign(s), such as decreased or absence of deep tendon reflexes, weakness (positive myotomes), and sensory (positive dermatome) deficits; x-ray shows no fracture; CT/MRI may show nerve involvement; possible disc lesion |
| 4 | Neck symptoms (pain, stiffness, restricted ROM) with fracture or dislocation and objective neurological signs, possible spinal cord signs |
CT, Computed tomography; MRI, magnetic resonance imaging; ROM, range of motion.
Modified from Spitzer WO, Skovron ML, Salmi LR, et al: Scientific monograph of the Quebec Task Force on Whiplash-Associated Disorders: redefining “whiplash” and its management. Spine 20(8 Suppl):8S–58S, 1995.
TABLE 3-8
Differential Diagnosis of Cervical Nerve Root and Brachial Plexus Lesion
| Cervical Nerve Root Lesion | Brachial Plexus Lesion | |
| Cause | Disc herniation Stenosis Osteophytes Swelling with trauma Spondylosis | Stretching of cervical spine Compression of cervical spine Depression of shoulder |
| Contributing factors | Congenital defects | Thoracic outlet syndrome |
| Pain | Sharp, burning in affected dermatomes | Sharp, burning in all or most of arm dermatomes, pain in trapezius |
| Paresthesia |