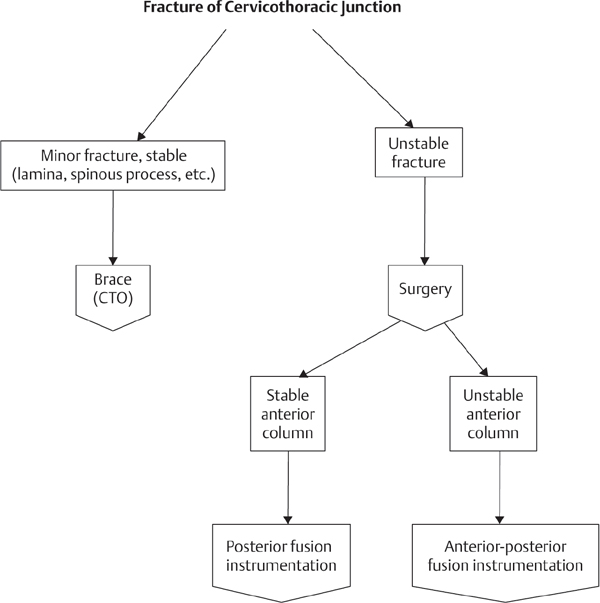
8 Facet dislocations are flexion-distraction injuries to the cervical spine that result from high-energy trauma. Motor vehicle crashes and falls are common modes of injury, and many patients may present with multiple other injuries in addition to their facet dislocation. Depending on the nature of the dislocation, the presence of associated fractures, and the amount of concomitant soft-tissue injury, the spine may be highly unstable. This instability may in turn lead to neurologic injury. Prompt recognition and treatment are essential for these injuries. Facet dislocations represent a spectrum of injury. Allen and Ferguson described four levels of severity: (1) facet subluxation, (2) unilateral facet dislocation, (3) bilateral facet dislocation, and (4) complete dislocation or spondyloptosis. These injuries are often also associated with facet fractures, endplate or vertebral body fractures, and discoligamentous injury. Radiographically, facet subluxation may appear with widening of the facet joint or with the facets “perched,” with the inferior artciular process from the superior level sitting atop the superior articular process from the subjacent level. Unilateral facet dislocations involve frank dislocation of one set of facet joints and subluxation of the contralateral joint. Generally, anterolisthesis of the superior body is less than 25% of anterior-posterior diameter of the vertebral body. Bilateral dislocations may have 50% anterolisthesis or more. Any patient suspected of having a facet dislocation should undergo a complete physical exam. As these injuries are associated with high-energy trauma, all patients should have a thorough examination of the head, body, and extremities to exclude any other injuries. A complete neurologic examination is essential and should include evaluation of sensation, motor function, reflexes, and rectal tone and sensation. Historically, all patients suspected of having a cervical spine injury or involved in a high-energy trauma were initially screened with plain-film radiographs. Recently, the increased availability and accuracy of computed tomography (CT) have led to plain films’ being bypassed and patients’ being sent directly for CT scans. The CT scan should include the entire cervical spine, including the occipitocervical and cervicothoracic junctions. The images should be reviewed to identify any associated fractures of the facets or vertebral bodies. Imaging of the thoracic and lumbar spine (either by plain-film radiographs or CT) should be obtained to exclude noncontiguous fracture. While magnetic resonance imaging (MRI) should be obtained on all patients with a facet dislocation, the timing of the study is a matter of debate (this is discussed further in the Treatment section of this chapter). Regardless of the time, the MRI should be used to evaluate for compression of the spinal cord or exiting nerve roots, herniations and injuries to the intervertebral disk, and ligamentous injury. The treatment of facet dislocation depends on the nature and severity of the injury, the presence or absence of any concomitant fractures, the neurologic status of the patient, and whether or not a reliable neurologic exam can be obtained from the patient. Facet subluxations can represent a spectrum of injury, ranging from relatively minor “sprains,” or injuries only to the facet capsule, to full dislocations that have spontaneously reduced prior to radiographs’ being obtained. An MRI may help to demonstrate the extent of ligamentous injury. Minor injuries may be treated in a hard collar, with frequent radiographs taken to ensure that no late-onset instability has occurred. Injuries that become unstable or that demonstrate extensive soft-tissue injury should be stabilized with surgery. Patients with either unilateral or bilateral facet dislocations will require reduction of the joint. Early reduction may help to reduce any tension on the spinal cord and neural elements, minimize swelling, and theoretically help to reduce the risk of or treat any existing neurologic injury. The timing of the reduction depends on the neurologic status of the patient and the ability to obtain a thorough neurologic exam on the patient. The need for MRI prior to reduction is a matter of great debate. Patients who are awake and who have complete neurologic injuries should be treated with immediate high-weight reduction. There is no need for MRI prior to reduction. Expedient reduction relieves pressure on the spinal cord as quickly as possible and gives the patient the best chance for recovery. An MRI should be obtained after reduction to identify any sites of continued spinal cord compression and to evaluate for any epidural hematoma. Surgical stabilization is then undertaken. Controversy exists regarding whether or not to obtain MRI prior to reduction in both patients who are awake with intact neurologic exams and patients with only radicular-type symptoms. This concern is driven by a case report describing a patient who was initially neurologically intact but then underwent anesthesia while a posterior open reduction and fusion was performed. She awoke quadriplegic. Subsequent radiographic evaluation revealed an anterior disk herniation, which was believed to have extruded into the canal during the reduction maneuver. This has led some to suggest that MRI should be obtained prior to any attempt at reduction to identify disks that may be at risk for possible posterior extrusion. These patients could then be treated with anterior discectomy prior to reduction to minimize the risk of further spinal cord injury. However, there is no clear definition as to what constitutes a disk that is at risk for hernitation. If no disk herniation is present, the patient can be treated with high-weight reduction, with careful observation to make sure that there is no change in the neurologic exam. For patients whose neurologic status cannot be assessed, either because the patient is unconscious, uncooperative, or intoxicated or because there are communication barriers or distracting injuries, an MRI should be performed to assess the patient’s injury fully and to exclude the presence of a large disk herniation. Treatment can then be based on the MRI findings. Traction can be used to perform a closed reduction of facet dislocations. This can be used in patients with complete neurologic deficits or in patients who are neurologically intact and from whom a reliable neurologic exam can be obtained. To perform a high-weight reduction, the patient is first positioned onto a bed with the traction apparatus attached at the head. Gardner-Wells tongs, made of stainless steel to prevent pin bending during reduction, are then applied to the skull with the pins 1 cm superior to the pinnae of the ears. Local anesthetic agents as well as narcotics should be used to help with the pain. The bed can be tipped into a reverse Trendelenburg position to help counter the force of the traction. The pulleys should be arrayed such that they enable both axial traction and slight flexion of the head. Flexing the head allows the facet joints to disengage and will permit reduction. Traction is started at 5 or 10 lb and then increased in 5 or 10 lb increments. In between the placements of additional weight, the patient’s neurologic status should be assessed and a lateral radiograph taken. Weight is added until the cephalad facets appear to have cleared the caudal facets. At this point, the neck can be extended and the traction shifted to a more axial vector. A lateral cervical spine film is again obtained, and if it shows reduction of the dislocation, the weight is gradually reduced. During the course of the reduction procedure, the process should be aborted if the lateral radiograph demonstrates excessive disk space widening, roughly defined at a disk space 1.5 times as great as that of adjacent levels. Likewise, if there is any change in the neurologic status, the weight should be removed and the patient taken for an emergent MRI scan. In addition to a disk herniation, other causes of neurologic injury, such as an epidural hematoma, should be excluded. The patient should then be taken emergently to the operating room for surgical decompression, reduction, and fusion. Surgery is indicated if a reduction cannot be obtained by closed reduction, if there is evidence of neural compression resulting in a neurologic deficit, or if the injury is felt to be unstable even after reduction. The approach selected depends on the goals of the surgery. Most dislocations without significant disk herniations can be treated with posterior instrumentation, reduction, and fusion. A large herniation may necessitate an anterior approach to remove the disk material, followed by reduction, grafting, and plate fixation. Some authors have asserted that anterior fixation alone may provide enough mechanical stability; however, many feel that anterior surgery alone is not sufficiently stable and should be backed up by posterior instrumentation. Injuries that are highly unstable or that are in patients with complete paralysis may be treated with both anterior and posterior fixation to provide maximal stability. Children with minor subluxations generally heal well when treated with collar immobilization. Soft-tissue healing in the adult patient is less predictable, and surgical intervention is often considered. Some patients may develop persistent neck or radicular pain when treated nonoperatively. These patients may be candidates for elective decompression and fusion. The outcome of patients with unilateral and bilateral facet dislocations depends on the severity of their injuries at the time of presentation and, particularly, their neurologic status. Typically these injuries will require surgical stabilization to prevent redislocation, late instability, and persistent pain. Dvorak MF, Fisher CG, Aarabi B, et al. Clinical outcomes of 90 isolated unilateral facet fractures, subluxations, and dislocations treated surgically and nonoperatively. Spine (Phila Pa 1976) 2007; 32(26):3007–3013 PubMed The authors retrospectively reviewed 90 patients with isolated unilateral facet dislocations or fractures. They concluded that these injuries resulted in long-term pain and disability and that patients treated operatively had better outcomes, despite more serious injury patterns, than patients treated without surgery. Grauer JN, Vaccaro AR, Lee JY, et al. The timing and influence of MRI on the management of patients with cervical facet dislocations remains highly variable: a survey of members of the Spine Trauma Study Group. J Spinal Disord Tech 2009;22(2):96–99 PubMed The authors surveyed 25 fellowship-trained spine surgeons regarding the need for MRI and its role in determining whether or not to proceed with open or closed reduction of a dislocated facet type injury. No consensus could be reached on the role of MRI or the type of reduction to be performed. Newton D, England M, Doll H, Gardner BP. The case for early treatment of dislocations of the cervical spine with cord involvement sustained playing rugby. J Bone Joint Surg Br 2011;93(12): 1646–1652 PubMed The authors report a series of 57 patients who sustained a facet dislocation while playing rugby. Thirty-two of these patients were completely paralyzed at presentation. Eight patients had their dislocations reduced within 4 hours. Of these, 5 had a complete recovery. Of the 24 patients who were paralyzed and whose dislocations were reduced after 4 hours, none had a complete recovery, and only 1 had meaningful improvement. CTO, cericothoracic orthosis
Cervical Facet Dislocations
![]() Classification
Classification
![]() Workup
Workup
Physical Exam
Imaging
![]() Treatment
Treatment
High-Weight Reduction
Surgery
![]() Outcomes
Outcomes
Suggested Reading
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







