Aaron G. Rosenberg
Cementless Acetabular Reconstruction in Revision Total Hip Arthroplasty
INTRODUCTION
As the indications for total hip arthroplasty widen and as the number of patients who have been previously treated with a total hip arthroplasty increases, revision total hip arthroplasty is becoming a more common procedure.1 In the vast majority of these cases where revision of the acetabular component is required, reconstruction can be successfully accomplished with a cementless, porous-coated, hemispherical acetabular component inserted with screws. Previous studies from our center2–6 and others7–20 have documented excellent results with these devices at intermediate-term and now longer term follow-up. The goal of this chapter is to outline the surgical technique for acetabular revision using a cementless component, define the indications and contraindications for this technique, and describe the clinical results associated with this method of reconstruction.
PATIENT EVALUATION
Initial patient evaluation includes a history, physical examination, and plain radiographs. An AP pelvis, AP, and lateral of the involved hip are mandatory for appropriate preoperative planning. In patients with severe acetabular bone loss, oblique radiographs of the pelvis may help to determine the amount of bone loss present and specifically evaluate the posterior column, anterior column, and for the presence of a pelvic discontinuity. A shoot-through radiograph of the hip can also be useful in evaluating the integrity of the posterior column and ischium (Fig. 13-1). Identification of a pelvic discontinuity is particularly important, as independent fixation of the pelvis with a plate or plates has been shown to be critical for a successful outcome, and alternative reconstructive options are oftentimes required for the majority of patients with a pelvic discontinuity.21
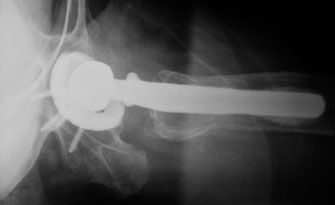
FIGURE 13-1. A shoot-through radiograph of the hip showing the posterior column and ischium.
Radiographic indicators of a pelvic discontinuity include a transverse fracture line seen on anteroposterior or oblique radiographs of the pelvis, medial translation of the inferior portion of the hemipelvis with a break in the ilioischial line, and rotation of the inferior hemipelvis that is seen as an asymmetry of the obturator ring when compared to the contralateral side (Fig. 13-2). Oblique radiographs of the pelvis are helpful in identifying a pelvic discontinuity; a break in the ilioischial line on the iliac oblique view is indicative of posterior column deficiency, and a break in the iliopectineal line seen on the obturator oblique view indicates anterior column deficiency. The acetabular component that is in place has often migrated a substantial distance above the true acetabulum and protrudes across the ilioischial line. Pelvic discontinuity is confirmed at the time of surgery when a transverse defect that spans the acetabulum is encountered. Gross motion of the inferior aspect of the acetabulum independent of the superior portion often is demonstrable.
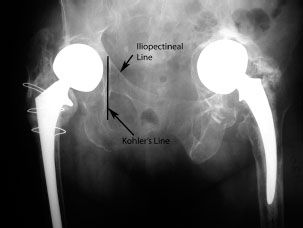
FIGURE 13-2. Pelvic discontinuity of the left hemipelvis. Note the break in the ilioischial and iliopectineal lines with significant superior and medial migration of the acetabulum, a transverse fracture line, and ischial lysis. Rotation of the inferior hemipelvis is seen as asymmetry of the obturator ring when compared to the contralateral side Normal radiographic landmarks are shown on the right hemipelvis.
Although preoperative planning is covered elsewhere, the importance of this portion of the operation cannot be overemphasized to ensure that all of the appropriate instruments and implants will be available to the surgeon at the time of operation. A review of the patient’s prior operative report or reports can also be extraordinarily helpful in planning for the safe removal of existing implants and in ensuring that any modular components needed (including appropriate trial components) will be available at the time of surgery. Preoperative evaluation for periprosthetic sepsis also is mandatory to rule out infection as a cause of failure.
SURGICAL TECHNIQUE
The preference of the authors, in the vast majority of revision total hip arthroplasties, is to use a posterior approach to the hip. This approach is extensile both proximally and distally and allows for access to the posterior column and is compatible with an extended trochanteric osteotomy if needed to facilitate femoral component extraction, improve exposure, or correct femoral deformity. Prior skin incisions are utilized whenever possible, and a continuous soft tissue sleeve is maintained from the posterior border of the gluteus medius (proximally) to the level of the gluteus maximus insertion (distally) to allow for an adequate soft tissue repair at the end of the procedure.
Once the prosthesis has been exposed, the hip is dislocated posteriorly, followed by extraction of the femoral component, or if it is to be retained, retraction of the femoral component anteriorly into a soft tissue pocket. Wide acetabular exposure is a necessity and a complete capsulectomy is routinely performed to accomplish this goal. It is critical to completely expose the interface between the existing acetabular component and the surrounding host bone to facilitate safe removal without damage to the existing host bone stock. Even grossly “loose” components can be difficult to extract secondary to bony remodeling and soft tissue interposition, and great care and patience must be exercised during this portion of the procedure.
Once existing components, bone cement (if present), and soft tissue have been meticulously removed, the acetabulum is then carefully examined (Fig. 13-3). Specifically, the integrity of the posterior column, anterior column, medial wall, and acetabular roof are inspected to determine if adequate bony support is present for cementless acetabular reconstruction. It is also critical to ensure that a pelvic discontinuity is not present as alternative reconstructive measures are required in these situations as previously discussed.

FIGURE 13-3. The previous acetabular component has been removed and the acetabulum cleared of all soft tissue. Note the contained defect seen in the superior dome of the acetabulum.
The acetabulum is then sequentially reamed with hemispherical reamers until an adequate bony bed is created for insertion of the revision component. Reaming is carried out in approximately 45 degrees of cup abduction and 20 degrees of anteversion, which is the desired position of the revision component. When reaming, it is imperative to avoid damage to the posterior column with progressively larger reamers; sacrifice of a portion of the anterior column may be necessary to create a hemisphere, and this technique is compatible with good results. In smaller patients, it is particularly important to ensure that the posterior column (which is oftentimes the main supporting structure for the revision component) is not reamed away in an effort to create a hemisphere. A trial component can then be utilized to determine the amount of host bone that will be in contact with the revision shell and to determine the stability of the proposed construct (Fig. 13-4). Although a “press-fit” is not mandatory, the trial should have stability when a posteriorly directed force is placed upon it; if the construct does not have any inherent stability, alternative techniques for reconstruction should be utilized. In general, a bleeding bed of bone is desired with more than 50% of contact between the host bed and the revision component although lesser percentages of contact may be required for larger diameter components with a correspondingly greater surface area available for bony ingrowth. The acetabulum usually is reamed to a size 2 mm smaller than the proposed revision component, although 3 mm of underreaming can be utilized for larger diameter (>70 mm) components.

FIGURE 13-4. A trial component is placed in the acetabulum to determine construct stability and the amount of host bone in contact with the revision component.
Any bony defects present are then packed with mor-cellized, fresh frozen, cancellous allograft bone (Fig. 13-5). It is imperative at this point to reverse ream the acetabulum to fully impact the allograft bone into the defects and to prevent the interposition of allograft bone between the bony surfaces that will be available for ingrowth and the revision component (Fig. 13-6). The revision component then is impacted into the acetabulum in approximately 45 degrees of abduction and 20 degrees of anteversion. Although a “press-fit” is not mandatory for a successful outcome, it provides additional stability to the construct (which is mandatory for bony ingrowth to occur) and facilitates the insertion of screws. A cup with multiple holes is utilized, and as many screws as possible are inserted into the posterior-superior quadrant to augment cup stability (Fig. 13-7). Screws should be of adequate length to ensure bicortical purchase, and tapping is recommended prior to attempts at screw insertion when the sclerotic bony surfaces of the revision acetabulum may make screw insertion difficult. The overall stability of the construct should then be tested to ensure that adequate stability has been achieved. A trial liner is inserted followed by any additional procedures that are required. It is presently routine in our practice to use larger diameter (36 or 40 mm) femoral heads for our revision total hip arthroplasties to increase construct stability (Fig. 13-8).

FIGURE 13-5. Fresh frozen particulate bone graft is placed into the acetabulum.
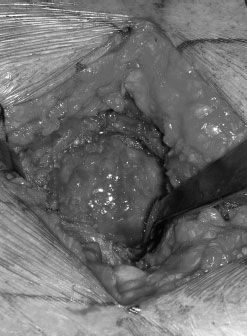
FIGURE 13-6. After reverse reaming of the acetabulum, the bone graft is fully impacted into the defects while clearing graft from all other areas exposing the native acetabular bone

FIGURE 13-7. Insertion of screws into the revision component after it has been impacted

FIGURE 13-8. Final construct with a 36-mm inner diameter liner engaged
RESULTS OF CEMENTLESS ACETABULAR REVISION
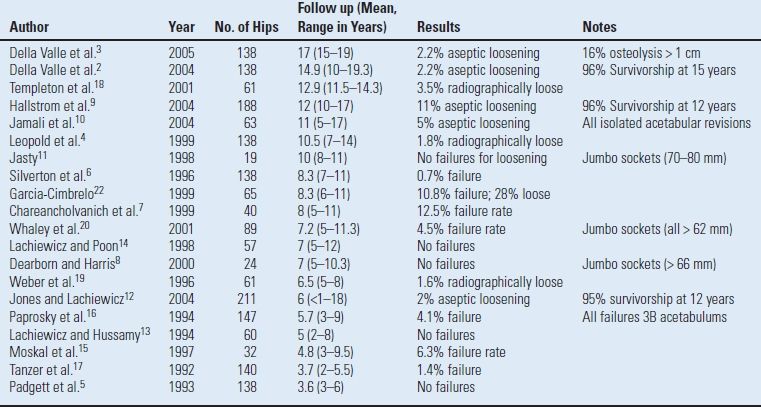
Numerous prior studies have documented the results of cement-less acetabular reconstruction in the setting of revision total hip arthroplasty (Table 13.1). These studies that examined cohorts ranging from 19 to 211 hips at a mean follow-up of 3.7 to 17 years have shown failure rates of zero to 12.5%.2–20,22
TABLE 13.1 Results of Cementless Acetabular Reconstruction in Revision THA
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








