Cemented Femoral Components
Andrew J. Timperley, Jonathan R. Howell, Matthew J.W. Hubble, Graham A. Gie and Sarah L. Whitehouse
Key Points
• Cemented stems (Fig. 67-1) are indicated in patients in all age groups who require a hip arthroplasty for any pathology (Fig. 67-2).
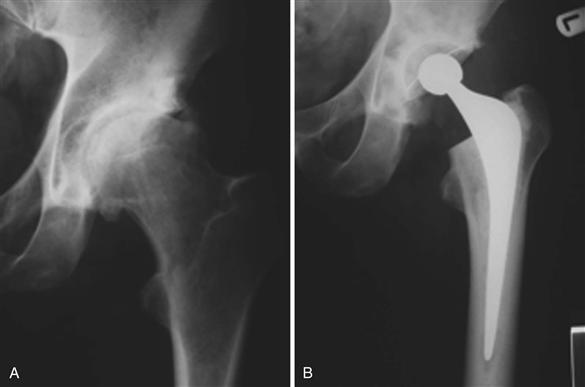
Figure 67-1 A cemented femoral component can reliably reproduce the biomechanics of the hip because femoral offset, leg length, and version all are independently variable.
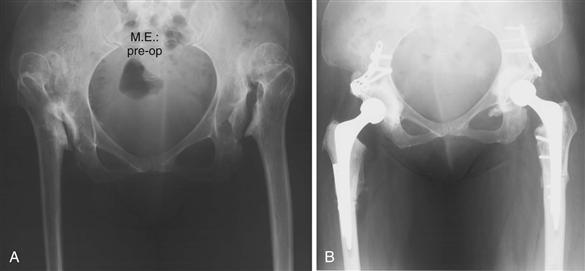
Figure 67-2 Cemented femoral components can be used for any pathology. In the case illustrated, subtrochanteric femoral osteotomies have been necessary in the treatment of bilateral Crowe IV developmental dysplasia of the hip (DDH).
Introduction
Although Philip Wiles1 of the Middlesex Hospital in London must be credited with the introduction of the first total hip replacement in 1958, it was Charnley who was the first to use acrylic cement to anchor the stem of an intramedullary femoral prosthesis,2 and McKee and Watson-Farrar3 of Norwich who were the first to use cement for fixation of the acetabular cup. It can be argued that acrylic bone cement is probably the most abused biomaterial, literally and figuratively, in use in orthopedic surgery. A cursory review of the literature shows that the surgical techniques employed when cement is chosen as the method of fixation are of great importance, but surgeons have blamed failure of cemented hip arthroplasty on fundamental failings of cement as a biomaterial,4 rather than on failure of the surgeon to appreciate the surgical steps necessary to use the material appropriately. Polymethylmethacrylate bone cement (PMMA) has no adhesive properties, and fixation using this material mandates that the surgeon establish a strong mechanical interlock with cement against host bone.5 Lars Linder6 pointed out that osseointegration “should be regarded not as an exclusive reaction to a specific implant material, but as the expression of a non-specific and basic healing potential in bone.” Malcolm7 demonstrated, in man, that acrylic bone cement can remain osseointegrated over the long term, thereby maintaining sound mechanical fixation of the implant. The cement-bone interface is thereby protected from intrusion of fluid under pressure containing particulate debris.
Detractors of the use of cement ignore the other beneficial attributes that are a corollary of its use. As it is used today, acrylic cement subserves several functions: Not only is it the means by which the implant is fixed to the bone, it is also an integral part of the mechanism of load transmission into the femur and is fundamentally just as much a part of the “implant” as the metallic component. Moreover, the viscoelastic properties of PMMA allow it to act as a load spreader, a shock absorber, and a decoupler of differential movements of structures of different modulus and structural rigidity.8
General Considerations
Shen,9 an engineer, suggested that cemented femoral components can be divided into two basic types (Fig. 67-3). Taper-slip or force-closed stems are exemplified by the original polished flatback Charnley (Zimmer, Warsaw, Indiana) and the polished Exeter (Stryker Inc., Newbury, United Kingdom) stems that routinely subside within the cement mantle without fracturing it. With these stems, stability is maintained by a balance of forces across the stem-cement interface with no form of bond between the two. Composite-beam or shape-closed stems cannot, by definition, subside within the cement, and stability is maintained by the bond that arises when the surface contours of the stem are matched and cement is applied to it.10 Kärrholm showed in a radiostereometric assay (RSA) study11 that subsidence of the stem at the stem-cement interface regularly occurred not only with taper-slip stems, but also with composite-beam stems, thus calling into question the whole concept of the composite-beam stem.
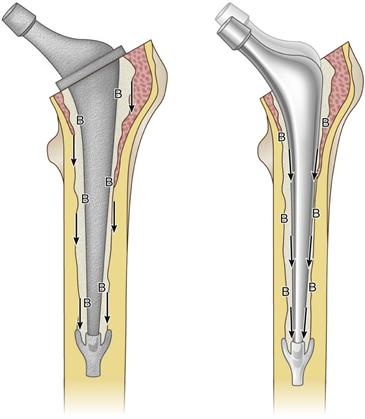
Figure 67-3 A composite beam stem is demonstrated on the left. The stem is bonded to cement (B), and shear forces are transmitted directly to the cement-bone interface (arrows). A taper-slip stem is demonstrated on the right. Shear forces are transmitted to the stem-cement interface, where subsidence occurs (arrows) and the cement-bone interface is protected (B).
Good results can be obtained using composite-beam stems, but they are less forgiving in terms of surgical technique.12,13 The basic surgical techniques described here for contemporary femoral cementing are valid for both types of stem. If a composite-beam stem is to be used, it is essential that a complete cement mantle of adequate thickness is established, as well as solid fixation at both the stem-cement interface and the cement-bone interface. Scheerlinck12 points out that although in vivo both concepts of stem fixation have proved effective, they cannot work together, and it is important to understand on which principle a particular stem relies.
In contrast to the variable results of composite-beam components, taper-slip stems have been demonstrated to yield excellent results in all existing national joint registries,14–16 as well as in individual publications from multiple centers. In engineering practice, the taper is one of the strongest and most reliable methods of transmitting not only axial but also torsional forces between one component and another. In the context of the cemented stem, subsidence of the tapered stem is analogous to engagement of the taper; if the stem is to function effectively as a taper, it must not in any way be fixed to the cement or end-bearing. Shen9 and Howie17 point out that the taper-slip system is more forgiving in terms of surgical technique, and the success of the concept is demonstrated by the fact that all major manufacturers of hip implants now have such stems in their portfolio. In contemporary practice, they are by far the most widely used cemented stems throughout the world.
To function by the taper-slip principle, a stem must be tapered in shape and must have a polished surface; also, there must be no feature on the device, such as a collar, that could prevent the stem from subsiding within the cement mantle. A stem with these characteristics can take advantage of the viscoelastic behavior of acrylic bone cement in that movement is allowed at the stem-cement interface without damage to the internal surface of the cement mantle. This subsidence has three important effects:
• As the stem subsides, it generates hoop tensile forces and radial compression within the cement (Fig. 67-4). Radial compressive forces serve to protect the cement-bone interface from any shear forces; they also load the bone. During periods of rest, tensile strain persists and stress relaxation of cement occurs, dissipating hoop tensile stresses.18 This mechanism protects the cement against fatigue fracture, and the whole loading regimen is dominated by compressive forces. Crowninshield and associates19 noted, “Load transmission by compression across the stem-cement boundary may be the only reliable mechanism of loading in vivo.”
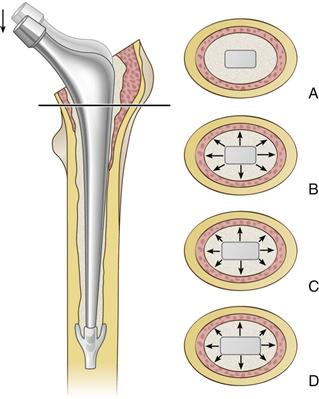
Figure 67-4 Transverse sections at the level of the line on the femur are shown. A, The unloaded situation. B, On loading, radial compressive stresses are induced in the cement. C, As the stem has subsided, a larger cross-section is accommodated by the cement, generating hoop tensile stresses within the cement mantle. D, On resting, residual hoop strain persists, and stress relaxation occurs within the cement of these tensile forces. The loading regimen is now dominated by compression at the stem-cement interface, within the cement, and across the cement-bone interface.
• Subsidence of the polished taper within the cement increases the torsional stability of the stem.20
With contemporary cementing, observed subsidence of the stem within the cement is approximately 1.3 mm at 17 years’ follow-up.21 It continues very slowly throughout the life of the implant, but with contemporary cementing, this is not of clinical importance with regard to leg length.22
Indications/Contraindications of Cemented Femoral Components
Cemented femoral stems can be considered for any patient who requires a hip arthroplasty. Cemented, taper-slip devices are recognized as delivering the gold standard in terms of long-term fixation.21–23 Use of a collarless, polished, tapered, cemented stem confers significant advantages over cementless designs in that stem size, stem offset, leg length, and version all are independently variable, allowing faithful re-creation of hip biomechanics no matter what the original deformity. Over the longer term, use of a taper-slip stem also confers an advantage if an additional operation is required to address problems with the hip other than femoral fixation. The device is, in effect, modular at the stem-cement interface, and the stem can be knocked out of a well-fixed cement mantle and another stem of similar design cemented into the existing cement mantle at the end of the procedure.24 This technique allows for correction of leg length, offset, and version, even in the revision situation.
In complex cases in which distortion of the anatomy occurs, femoral shortening procedures and de-rotation osteotomies can be carried out. The osteotomy site can be protected from cement intrusion by the use of autograft or allograft bone chips impacted into the endosteal surface. Cement fixation confers an advantage in cases of previous septic arthritis of the hip, because acrylic bone cement can be loaded with an appropriate antibiotic to reduce the risk of recrudescence of infection.
For any patient in whom a hip arthroplasty is indicated, there are no specific contraindications for the use of cement fixation.
Preoperative Planning
The aim of preoperative planning is to determine the correct position of the components to allow restoration of the anatomic center of rotation of the joint, and to re-create the correct leg length and offset. Preoperative planning also helps the surgeon predict, before the start of the procedure, the need for appropriate instrumentation, prostheses, and, occasionally, bone graft. A major advantage of scaled digital templating is that implant templates can be imported at the correct size rather than at the assumed 120% magnification, as is the case with acetates. The image taken for templating must be taken with a scale on the image. An ideal scale for hip replacement is a total hip replacement (THR) on the contralateral side, where the size of the femoral head is known. The next best system is for a marker of known size to be placed in the plane of the femoral head. We have established a convention to position a HipScaler (www.hipscaler.com) on all anteroposterior (AP) x-rays of the pelvis taken at our institution, thereby reducing the need to take additional films for this purpose.
Clinical examination of the patient is an essential part of the preoperative assessment, so that the surgeon is aware of any true or apparent leg length discrepancy or fixed contracture of the hip, or the presence of fixed pelvic obliquity. In the absence of a navigation system, it is the responsibility of the operating surgeon personally to position the patient on the operating table so that he or she is aware of the relative position of the pelvis to the horizontal and vertical planes.
Radiologic Assessment
X-rays ideally should be taken with the hip internally rotated by 15 degrees. If the film is not taken in this position, with the x-ray beam perpendicular to the femoral neck, the x-ray will suggest a more valgus femoral neck with reduced offset and a higher center of rotation in relation to the femur than is actually the case. In addition to the clinical assessment, the x-ray profile of the lesser trochanter will give the surgeon a clue to any rotational deformity of the femur.
The surgeon should determine whether there is deficiency or excess of bone and should identify (1) the presence of any leg length discrepancy, (2) the center of rotation of the acetabulum and the femur, and (3) the offset of the hip (the distance from the neutral axis of the femur to the center of rotation of the femoral head). If the contralateral hip is normal, this makes planning easier, because the goal is usually to re-establish native hip biomechanics.
This process allows the surgeon to plan the following:
• Position of the center of rotation of the prosthetic socket
• The need to remove any bone or to undertake a bone grafting procedure
• Offset of the stem to be inserted (Fig. 67-5)
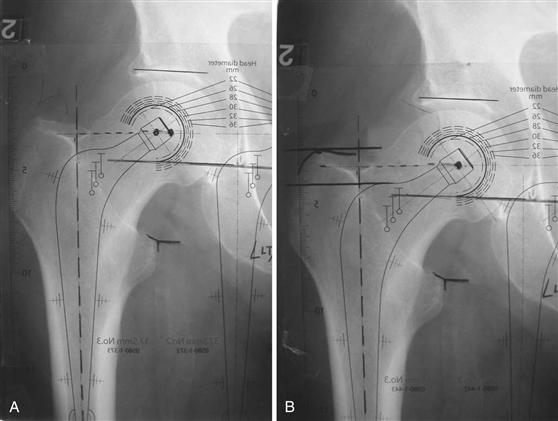
Figure 67-5 A, A template of a femoral component of insufficient offset has been laid on the x-ray. B, A femoral component with a greater offset is chosen, and it now can be seen that the center of rotation of the prosthesis coincides with that of the native hip. Leg length is unchanged.
• Stem size within the range of stems of the desired offset
• Depth of the stem insertion in relation to the tip of the greater trochanter
Results
Survivorship data with the longest follow-up when a double-tapered, collarless, polished cemented stem has been used have been published by the Exeter team (from the Exeter stem). At the 33rd year of follow-up, stem survivorship with the endpoint of revision for aseptic loosening was 93.5% (95% confidence interval [CI], 90.0% to 97.0%).22 In the “worst case scenario,”25,26 in which all cases lost to follow-up are regarded as failures from aseptic stem loosening, survivorship was 85.8% with a 95% CI of 81.3% to 90.3%. Of 433 hips in the series, 14 have been revised for aseptic stem loosening (3.46%). Two of these were re-revisions, and two had previously undergone intertrochanteric osteotomy. None have been revised for aseptic loosening since the 20th year of the survivorship study, and none have been lost to follow-up since that time. These results were achieved with first-generation cementing techniques and with surgeons of widely differing experience, illustrating that excellent results can be attained with a stem functioning by the taper-slip principle, despite relatively poor quality cementing by today’s standards. The Exeter Universal stem, which had an identical surface finish and a very slight difference in stem geometry but functions in exactly the same way, was introduced in 1988. The 17-year survivorship with the endpoint of revision for aseptic stem loosening was 100% in the series published by the design center.21 In a separate study of results in patients younger than 50 years27 at the time of surgery (average age at surgery, 42 years), with no case lost to follow-up, stem survivorship was 100% with revision for aseptic stem loosening as the endpoint, and 99% for all causes of stem revision, including periprosthetic fracture. This occurred at 10 to 17 years’ (average, 12.5 years’) follow-up. No case showed focal femoral osteolysis.
Many reports from other centers have described results with stems that function by the taper-slip principle.28–49 Burston50 reported results in patients younger than 50 and concluded, “… the performance of polished tapered stems in patients younger than 50 years is excellent, with stem survival and subsidence equivalent to the older, standard hip arthroplasty population. They compare very favorably with other stem designs that have been reported among the younger patients. With ease of insertion and such predictable behavior, this type of stem has to be the benchmark for comparison to other stem designs, including uncemented stems and resurfacing implants, in this young age group.” All papers cited reported a consistent pattern of behavior with regard to femoral components, irrespective of the experience of the operating surgeon, and demonstrated similar results to those obtained in Exeter with benign radiologic appearances, a small degree of subsidence within the cement mantle, and satisfactory clinical outcomes.
Survivorship analysis, as used in hip registries, is a powerful tool in the long-term assessment of arthroplasty because it gives a more realistic presentation of longevity than is provided by simple examination of failure rates. The behavior of the polished Exeter Universal stem in the Swedish and Norwegian Hip Registries is, in general, in line with results from elsewhere.15,51-55 Furnes and associates55 reported that the Exeter had the lowest percentage revision rate at 15 years (3.0%) and the smallest increment in revision rate between 10 and 15 years (from 2.2% to 3.0%) among the 10 most commonly used cements in Norway. A study from Finland56 of patients aged 55 years or older undergoing surgery for osteoarthritis found that the only femoral and acetabular component combination to have a survivorship greater than 90% at 15 years was the Exeter Universal/Exeter All-Polyethythene couple. The most recent study from the Swedish Registry15 includes a detailed analysis of implant survival for all diagnoses and all reasons for revision from 1992 to 2007, and allows separation of the results of different cups with the same variety of stem. The combination of the Cenator flanged cemented cup with the Exeter polished Universal stem (660 hips) shows survivorship at 5 and 10 years of 99.5% and 98.8%, respectively.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








