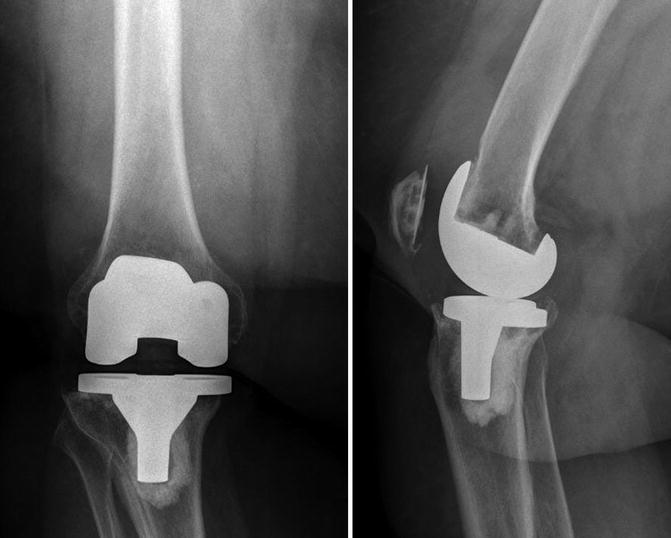
Fig. 18.1
Screw holes in the tibial component are prone to facilitate dissemination of wear particles into the bone, which then causes aseptic loosening
Osteolysis is more common around the tibial component for multiple reasons including its inherent relation to the polyethylene insert and gravity, and occasionally, when screws are used for fixation of the component, their pathway facilitates the migration of polyethylene wear particles into the bone [15] (Fig. 18.1). Moreover, the role of the polyethylene manufacturing technique, wear, and osteolysis has been widely described in the literature [7, 28, 29]. Compression-molded polyethylene has shown less wear than components machined from extruded stock [7, 16]. Early generation ultrahigh molecular weight polyethylene sterilized with gamma radiation in air and stored in oxygen-rich environment showed significantly high wear rates and potential osteolysis [9, 28–30]. This was related to the production of free radicals during radiation, which became entrapped in the crystalline portion of the polyethylene, in addition to its exposure to oxygen either during its shelf life storage or in the joint fluid in vivo, resulting in oxidation and detrimental effects in terms of degradation and deterioration of the material properties through different mechanisms including chain scission, embrittling, decreased fatigue strength, fracture toughness, and wear resistance [7, 31]. In an attempt to overcome this problem, manufacturers applied different sterilization techniques including sterilization in an oxygen-free environment by using either a vacuum or an inert gas (i.e., nitrogen or argon), which avoided the immediate oxidation and potentially decreased wear [32]. Additionally, last generation ultrahigh molecular weight polyethylene is processed using a moderate amount of irradiation to cross-link improving wear properties, complemented with different techniques to minimize the effects of the resulting free radicals. Some of those techniques include sequentially cross-linking and vitamin E doping which significantly decrease the free radicals and wear [32–34]. Not all the attempts to enhance polyethylene have been successful. For example, heat pressing and carbon fiber reinforcement resulted in increased fatigue modes of wear [7, 26, 35]. The cross-linking process also reduces fracture toughness and elevates wear in abrasive conditions, which produces small-particle size wear. Even when this last generation polyethylene has shown a significant decrease on volumetric wear, long randomized trials are needed in addition to implant registry data to determine differences in survivorship [36]. Another factor that plays a role on wear resistance is polyethylene thickness. Bartel et al. [37] showed that the contact stresses in polyethylene inserts with a less than 6 mm thickness increase exponentially as the thickness of the implant decreases. For this reason, the FDA requires a minimum of 6 mm thickness for new knee implant designs. Finally, more conforming or congruent polyethylene inserts exhibit less contact stresses and consequently less wear when compared with flat inserts [12, 26]. However, increased conformity limits the range of motion and increases stresses on the ligaments, implant-bone interface, and tibial base plate fixation and potentially increases backside wear [26, 38].
Mobile-bearing designs were introduced to allow high conformity at the articular surface with more normal kinematics in an effort to decrease wear and osteolysis. Large series have demonstrated good results with such implants [39]. However, these implants are not invulnerable to wear mechanisms. There is still a significant amount of backside wear in addition to the damage produced by debris trapped between the polish metal and insert backside. The wear particle debris type produced with these implants is smaller and more reactive, thus causing significant osteolysis [39, 40].
The mobile-bearing component causes wear on both the upper and lower surface of the bearing [76]. Increased AP-translation or rotation may cause increase polyethylene wear in the long-term perspective. The analysis of inlays, retrieved during revision surgery, showed more wear in the medial compartment in higher polyethylene shelf age and in more varus-aligned knees after a mean time of 8 years. The wear pattern of mobile and fixed bearing was analyzed in a knee simulator [76]. The wear rate averaged 5.38 mg per 106 cycles for the mobile bearings and 3.04 mg per 106 for the fixed bearings showing no reduction in wear despite increased congruency between the femoral component and the polyethylene inlay in the mobile-bearing design.
18.1.2 Mechanical Loosening
This is more common on constrained implants and it is time related. Mechanical loosening in hinge components evident with radiolucent lines occurs as early as 2 years after the procedure [41]. This may be related with an increased congruity and constrain of the articular surface, which decreases the load on the surrounding soft tissues but increases stresses at the implant-bone interface [7, 42]. Increased body mass index and level of activity may also play a role in the accelerated loosening [11]. There are different mechanisms of mechanical loosening, but the main one is related with micromotion between the implants and bone [43]. This is more common in cementless components, where the fixation can be maintained only by weak fibrous tissue especially in the tibia [44]. This type of fixation is avoided in the new type of porous surface components [45]. Moreover, the use of short keels on the tibial component combined with isolated application of cement only to the cut surface and implanting the short keel with a press-fit technique has been associated with a slight increase of early loosening [46].
Another described mechanism of mechanical loosening is the sink or subsidence of the component into the bone. This is also more common in the tibial component [47] (Fig. 18.2). Although some migration can occur within the first year, if this progresses, it may lead to early loosening. This phenomenon is more common on cementless components and when the fibrocartilage has not been removed from the interface between the implant and the bone [43, 48]. Moreover, the bone strength may play a role on the fatigue at the implant-bone interface and component subsidence [49]. This phenomenon can also occur in cemented components. If there is lack of supportive trabecular bone to maintain the cement-bone interface, the tibial component can subside [50]. Since this is more frequent in patients with severe osteoporosis, components with diaphyseal stems may be used to prevent subsidence.
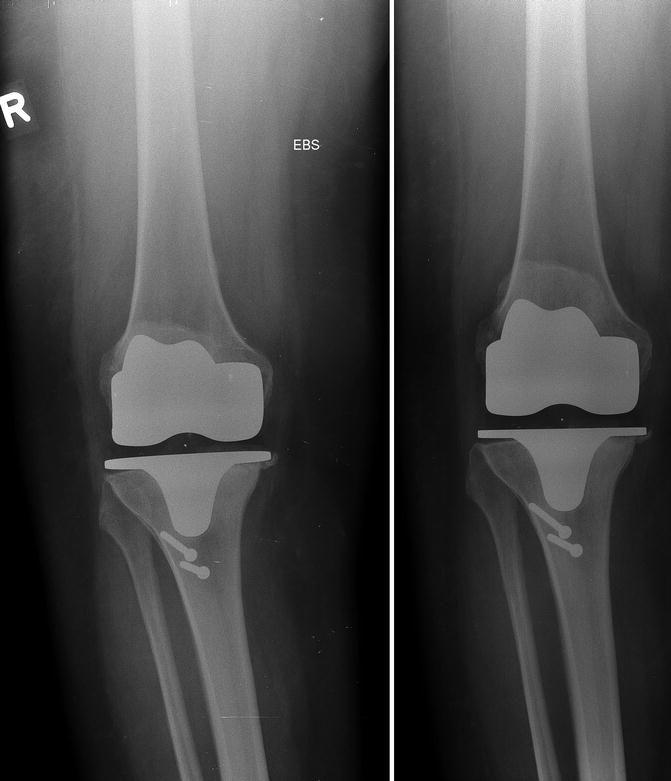
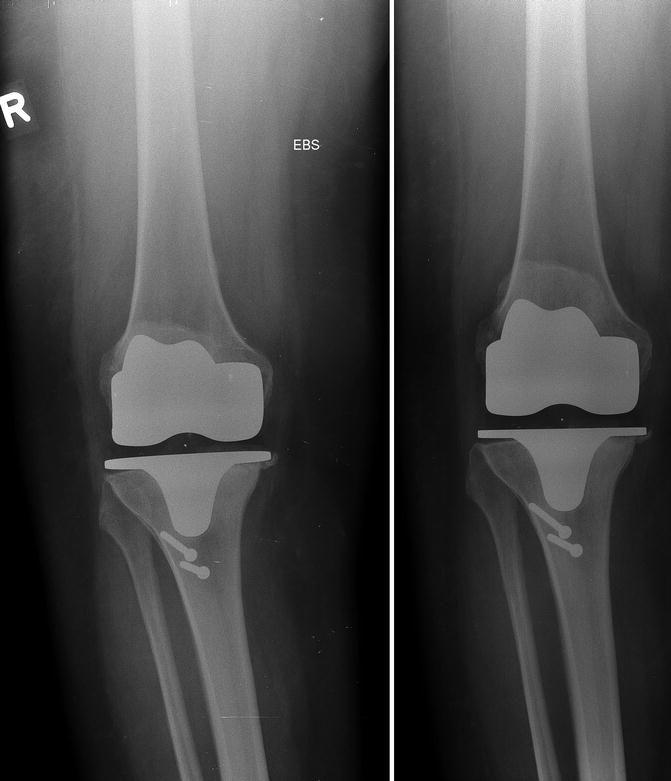
Fig. 18.2
Mechanical loosening of the tibial TKR component with subsidence and sinking
Although loosening of the femoral component is uncommon, it is possible. This loosening may be due to inaccurate bony cuts, poor cementation technique, or deficient bone (Fig. 18.3) [51]. When it occurs, such loosening follows a particular pattern of bone resorption on the posterior condyles and anterior migration and rotation on flexion of the femoral component [52]. This is associated with the high stresses concentrated in this area and osteoporotic bone. Loosening of the patellar component is also a significant cause of TKR revision [53]. Some factors associated with loosening of the patella include poor cementation technique, cementation into sclerotic bone, malposition of the patellar component, subluxation, osteoporosis, and avascular necrosis [51, 54]. Patient-related factors for loosening of the patella include increased weight, increased activity, and male gender [54].


Fig. 18.3
Inaccurate bony cuts are not uncommon in TKR and can be considered as risk factors for early aseptic loosening
18.1.3 Component Malposition and Malalignment
The malposition of the components and extremity malalignment in the coronal, sagittal, or rotational planes change the mechanics of the knee joint, increasing point stress loads on the polyethylene and the tibial component, causing further wear and potentially leading to aseptic loosening [55–58]. This mechanism of failure has been more frequently described in cementless components [24]. In cemented components, the load is distributed more evenly across the tibia, reducing the chance of failure even in the presence of malalignment [7]. If a point-loaded situation occurs in cementless components, it may create bone necrosis under the overloaded tibial component and failure of fixation on the opposite condyle due to the excessive tension at the interface [59]. Varus positioning of the tibial components has been linked to early loosening when using early generation designs [60, 61]. This position can lead to progressive sinkage and migration into the medial tibia. However, the most current designs series have not shown such an increased loosening and failure when placed on varus position [62].
Malrotation of the components can also lead to increased wear and potentially loosening. Some reports documented polyethylene posterior wear patterns caused by a tight posterior cruciate ligament (PCL) and/or external rotation of the tibial tray on PCL-retaining TKR [7, 63]. Moreover, an in vitro mechanical study showed how malrotation of the femoral component can cause patellofemoral maltracking and change the contact mechanics of the articulating patellar polyethylene (Fig. 18.4) [64]. The contact area decreased with progressive maltracking, with a concomitant increase in contact pressure. The amount of contact area that carries more than the yield stress of ultrahigh molecular weight polyethylene significantly increased with progressive maltracking. These elevated pressures could cause accelerated and excessive wear of the patellar component [64].
Fig. 18.4
(a) Knee lateral x-ray showing significant loosening of the femoral component 3 years after cemented PCL-retaining TKR. (b) Sunrise view showing the femoral component was placed in internal rotation which caused maltracking of the patella and significant wear of the patellar component. There was significant loosening of the femoral component
18.1.4 Instability
Ligamentous instability, hyperextension instability, extensor mechanism issues causing buckling, and/or mid-flexion instability may cause loosening due to the inappropriate articulation of the components, increased polyethylene wear, and potential damage of the implant [7, 51]. Instability can be correlated with malposition of the components or overall malalignment of the extremity. If the femoral, tibial, and patellar components do not articulate appropriately, increased stresses on a specific area, maltracking, and subluxation can increase polyethylene wear through the mechanisms described above (i.e., delamination) [7]. Instability is more common on posttraumatic arthritis, rheumatoid arthritis, and neuropathic arthropathy where there is attenuation of the collateral and posterior cruciate ligaments. Posterior-stabilized components or more constrained implants may prevent such complication [65]. When ligamentous laxity has not corrected at the time of surgery or there is instability after posterior-stabilized TKR (i.e., hyperextension), the stresses and impingement on the box post can be higher, possibly resulting in damage (i.e., post fracture) of the post and increase adhesive wear [66]. However, this can also happen without instability [10, 66]. When using such implants, it is important to avoid excessive flexion of the femoral component or posterior slope of the tibia to minimize this potential problem. In cases where PCL-retaining components were used and there is laxity or progressive attenuation of the PCL, the translation of the femur on the tibia increases shear stresses on the polyethylene accelerating wear and potential subsequent failure [12, 42, 65].
18.2 Preoperative Evaluation
A proper and thorough preoperative evaluation is necessary to determine the main cause of the loosening. Most causes of aseptic loosening will elicit symptoms, including knee pain, several years after the primary TKR. If there is knee pain or signs of loosening early after TKR, then periprosthetic joint infection should be considered unless and until proven otherwise. Infection will be addressed in a different chapter. The preoperative evaluation includes a complete history and physical examination, routine radiographs, and standard laboratory tests. More often than not, advanced imaging and additional laboratory tests are required to assist in establishing a diagnosis and developing a plan for surgery. Proceeding with surgery without identifying the cause for failure will likely result in a poor clinical outcome [67].
18.2.1 History
At the initial evaluation, history should be focused on three main factors: duration and timing of symptoms, type of symptoms (pain vs. instability), and associated causes of exacerbation or improvement of such symptoms (i.e., whether symptoms are exacerbated by activity and weight bearing and improved by rest). Additionally, referred pain should always be ruled out. Pain that radiates down the leg to the knee may be originating from the lower back or an arthritic hip. Symptoms that present early after TKR (within 2 years of surgery, excluding sepsis) are more related with instability and component malposition, whereas symptoms from wear, osteolysis, and/or loosening appear later. Other potential sources of pain early after TKR include peripheral neuropathy and regional complex pain syndrome. Aseptic loosening in general is manifested as a combination of pain and instability that is exacerbated by activity and weight bearing and improves with rest. However, start-up pain is correlated with loosening, whereas mechanical symptoms such as catching and giving way are correlated with instability [68]. Sometimes, when loosening is present, pain is severe enough to make patients delay their stance phase during ambulation, until after several steps when the pain decreases due to a probable “settling in” of the prosthesis. However, the pain returns with longer strides due to the micromotion. Occasionally, patients with osteolysis that were initially asymptomatic become symptomatic when loosening, presenting as boggy synovitis and joint effusion, is the culprit [10, 15]. Failure of the tibial insert may be associated with severe pain, effusion, crepitus, and grinding of the knee [51]. In general, aseptic loosening had an asymptomatic period with appropriate knee function prior to the manifestation of symptoms.
As part of the initial history, a detailed review of medical records including the operative report, hospital discharge, and rehabilitation notes aids to identify preoperative range of motion, instability, and other potential sources of pain. If severe deformity (i.e., varus deformity >15° or significant flexion contracture) was present preoperatively, it may cause early tibial loosening [51, 69]. The identification of certain types of implants may explain loosening or failure, if they have already been reported in the literature or registries (i.e., metal-backed patella components [70] or some cementless components [71]). Some specific types of implants have inherent failure mechanisms that should be considered (i.e., PCL-retaining components may have breakage of the tibial insert post). It is important to know in advance what types of implants are going to be revised for preoperative planning. Many components are modular, and therefore having the correct size implants with varying options of constraint, augments, and wedges can minimize intraoperative difficulties. Without proper preoperative planning, unnecessary removal of well-fixed components may be required to insert an available implant, which may lead to added bone loss.
18.4 Radiological Investigation with Regard to Aseptic Loosening
Radiographic evaluation should include a weight-bearing anteroposterior (AP), lateral, and skyline patellar views. These are used to assess fixation, polyethylene wear, osteolysis, radiolucent lines, patellar tilt, and component size and position. Full-length weight-bearing AP radiographs help to evaluate overall limb alignment, as well as pathology in the ipsilateral hip. It is important to have the x-ray beam parallel to the top of the tibial tray to allow measurement of polyethylene wear and evaluate the implant-bone interface. However, the accuracy of this mechanism to measure wear is very low [7]. Moreover, as little as 6° of angulation can obscure radiolucent lines [51, 72]. To overcome this problem, oblique radiographic views facilitate detection of early osteolytic lesions [73]. Radiolucencies typically start on the periphery of the implant-bone interface and work their way around the tibial or femoral component. Sometimes, it is difficult to differentiate stress shielding of the distal femur from osteolysis. Only experience and clinical judgment make this differentiation and diagnosis of osteolysis and loosening more accurate.
In all radiographic views, the overall alignment of the components relative to the mechanical and anatomical axes should be evaluated; alignment of the components relative to each other, size of the components, and the presence of radiolucent lines at the implant-bone interface and cement-bone interface should also be evaluated. Fractures and bone masses should always be considered as potential sources of pain and should be ruled out with the radiographic evaluation. In addition, initial preoperative and serial postoperative radiographs are helpful, especially if the initial operation was performed elsewhere. Loosening is radiographically evident more commonly on the tibial component, showing radiolucencies >2 mm, progressive radiolucent lines around the implant, change in component position, subsidence, and cement fragmentation (Fig. 18.5) [51]. Polyethylene wear may be evident as an asymmetric narrowed joint space on the weight-bearing view and significant osteolysis. It is important to understand that the radiographic findings should be correlated with the patient’s history and symptoms. Not all radiolucent lines necessarily mean that the components are loose. Smith et al. [74] reported the presence of incomplete, nonprogressive radiolucent lines surrounding cemented tibial components at 10 years after TKR in 15 % of a group of 207 patients. No migration or failure was associated with these radiolucent lines. In cases of significant radiolucent lines in asymptomatic patients, it is important to follow them closely with serial radiographs.