Fig. 27.1
Ochronotic involvement of the tendon at the place of its insertion to the bone
In this case report, we present the occurrence of peripheral enthesopathies in a patient with familial occurrence of ochronosis. We also describe the possibility of using musculoskeletal ultrasonography in the diagnostics of enthesopathies.
Case Report: A 56-year-old patient with the occurrence of familial ochronosis in two elder sisters coming from Záhorie region. The disease initially had painless course; the first clinical symptoms occurred after the age of 40 in the form of Achilles tendon pain bilaterally which are rarely presented early symptom of the disease in literature. Back pain and recurrent oedema of the knees and ankles successively appeared. In 2001, the patient underwent arthroscopic synovectomy due to recurrent exudative synovitis of the left knee at the regional orthopaedic department, with the finding of hyperpigmented foci on cartilages. On the basis of arthroscopic finding, typical ochronotic colouration of the scleras, alkaptonuria and positive family history, the patient was diagnosed with ochronosis. From that time, the patient has been followed by his local rheumatologist as well as at the National Institute of Rheumatic Diseases in Piešťany. In the further course of the disease, back pain was escalating with relatively rapid development of ankylosis on the basis of secondary degenerative changes. The patient also had the signs of bilateral gonarthrosis grade III and coxarthrosis grade II with recurrent plastic synovitis and repeatedly inflamed lymphoedema of the right leg that regressed after the administration of haemorheologic agents and enzyme therapy. In March 2010, he underwent implantation of total endoprosthesis of the right knee due to severe deformity and significant functional limitation.
In June 2010, the patient was hospitalised at the National Institute of Rheumatology Diseases due to recurrent oedema and pain of the left knee. Apart from the above-mentioned painful oedema of the left knee, clinical findings included accentuated kyphotic deformity of the spine with limited mobility as well as worsened mobility in the arms, hip joints and knees. In the left knee, there was a severe pressure pain at the site of insertion of the patellar ligament to the tibia that did not correlate with the extent of clinical finding on the knee. Physical examination revealed typical ochronotic colouration of the right sclera and urine darkening on standing in daylight (Fig. 27.2).


Fig. 27.2
Alkaptonuric colouration of urine after a longer stay at daylight
Laboratory examinations showed moderately elevated markers of inflammation (ESR: 35/75, CRP: 12.2 mg/L); blood count, hepatic enzymes, uric acid and renal parameters were in reference range. Negativity of rheumatoid factors, antinuclear (ANA) as well as of anti-citrulline (anti-CCP) antibodies persisted in immunological profile. Radiological examination showed signs of considerable secondary destruction of axial skeleton due to ochronosis with the development of secondary osteoarthrotic changes (Fig. 27.3). There were also bigger enthesophytes in the area of greater trochanters (Fig. 27.4) and one small enthesophyte on the upper pole of patella of the left knee (Fig. 27.5). In the context of differential diagnostics of the left knee involvement with dominant clinical symptoms, we performed musculoskeletal ultrasonography which revealed small anechogenic effusion in the area of suprapatellar recesses with parietally thickened synovium up to 3 mm, more echogenic and reduced intra-articular cartilage and marked enthesitis affecting patellar ligament. At the place of insertion of patellar ligament to tibial tuberosity, ultrasonography showed considerably widening of the tendon up to 7.3 mm, which was hypoechogenic with typical loss of fibrillar structure and anisotropy, with small hyperechogenities and enthesophytes along it and higher congestion during power Doppler mapping (Fig. 27.6). Admixture of hyperechogenities along the tendon was very probably caused by secondary calcifications as the consequence of calcium deposition to ochronotically widened and pathologically changed tendon. The real cause of marked enthesopathy would be clarified by targeted histological examination that was not performed due to ethical reasons. Ultrasonographic examination is a non-invasive, patient-friendly and cheap method for verifying the severe involvement of insertions that often dominates in clinical findings of this relatively frequently diagnosed disease.



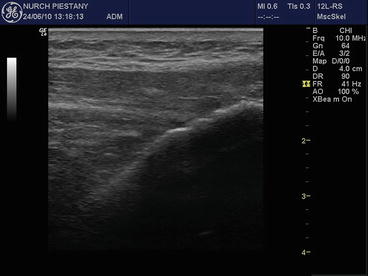

Fig. 27.3
X-ray of thoracic spine with narrowed hyperpigmented intervertebral discs and secondary osteoarthrotic changes

Fig. 27.4
Pelvis X-ray with narrowed articular slits of hip joints, bigger enthesophytes on femur trochanters and fibro-ostoses on the alae of ilium bones of even hyperostotic character

Fig. 27.5
X-ray of the left knee with narrowed articular slit, marginal osteosclerotic changes and small enthesophyte on the upper pole of patella
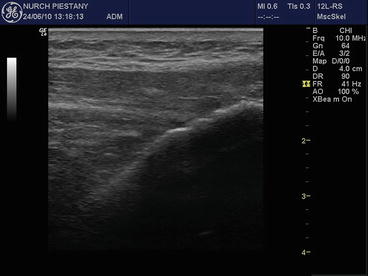
Fig. 27.6
Ultrasonography of the left knee. Widening of the tendon of patellar ligament that is hypoechogenic with typical loss of fibrillar structure and anisotropy. Small enthesophytes and fine hyperechogenic calcifications at the place of insertion on tibial tuberosity
NSAID of diclofenac type in combination with vitamin C was continued in medication; local therapy of the left knee consisted of NSAID gel phoresis, cryotherapy and individual rehabilitation. Comprehensive therapy and rehabilitation resulted in mitigation of the symptoms of acute enthesitis.
In this case report, we wanted to highlight the frequent occurrence and problems of enthesopathy in patients with ochronosis – the topic that has been presented only rarely in the literature. In these cases, polymers of homogentisic acid deposit excessively in the structures of locomotor system. In the highly developed forms of the disease, insertions are mostly affected, resulting in considerable clinical problems. The use of more recent imaging methods like musculoskeletal ultrasonography or MRI can clarify the cause of problems in these patients. High-frequency ultrasonography with at least 10 MHz linear probe should be used. The higher the frequency, the better the imaging of more superficial structures. The advantage can be the use of ‘power Doppler’ mapping to detect increased irritation congestion at the place of insertions. Therapeutic options comprise analgesics or NSAID, NSAID gel sonophoresis. In acute inflammatory irritation signs, cryotherapy and targeted individual rehabilitation can be temporarily used.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





