Chapter 22 Care of the Newborn
Preconception and Intrapartum Health
Preconception Counseling
Preconception counseling regarding genetic diseases such as cystic fibrosis and Huntington’s disease, as well as the dangers of tobacco, alcohol, and substance abuse, should be addressed with women of childbearing age. All women considering pregnancy should be encouraged to take in 400 μg (0.4 mg) of folic acid per day. Oral folic acid supplementation before conception can significantly decrease the risk of neural tube defects (Czeizel and Dudas, 1992; MRC Vitamin Study Research Group, 1991). Women who have had a previous pregnancy affected by a neural tube defect should take 4000 μg (4.0 mg) of folic acid daily beginning 1 month before pregnancy (Centers for Disease Control and Prevention [CDC], 1992).
During pregnancy, maternal illness can adversely affect the fetus and lead to adverse neonatal outcomes. Maternal hypertension, preeclampsia, alcohol and tobacco use, illicit drug use, and autoimmune diseases can cause intrauterine growth restriction (IUGR) and preterm birth. Children born to women with diabetes mellitus or gestational diabetes are at risk for shoulder dystocia, operative delivery, hypoglycemia, and birth trauma (American College of Obstetricians and Gynecologists [ACOG], 2005). Maternal hyperglycemia at delivery also puts the infant at risk for hypoglycemia. Poorly controlled maternal hypothyroidism and hyperthyroidism are associated with low birth weight (LBW) and preterm delivery (ACOG, 2005). Fetal alcohol syndrome is directly caused by maternal alcohol use and abuse, and other illicit drug use is associated with preterm birth, congenital abnormalities, neurobehavioral abnormalities, and neonatal drug withdrawal syndromes (ACOG, 2005). Box 22-1 lists the more common human teratogens seen in the United States.
Box 22-1 Selected Teratogenic Agents in Humans
Modified from Shepard T. Catalog of Teratogenic Agents. 11th ed. Baltimore, Johns Hopkins University Press, 2004.
Transition from Fetus to Newborn
Neonatal Resuscitation
The successful transition to extrauterine life depends heavily on the ability of the neonatal pulmonary system to adapt quickly and provide oxygen to the infant. Any illness or injury that interferes with oxygenation puts the infant at great risk and should be identified and treated promptly. It is important that with every delivery, at least one person trained in neonatal care and resuscitation be assigned to care specifically for the infant. Caregivers should have immediate access to the necessary equipment for a complete resuscitation. If there is concern that the newborn will be at high risk for complications (e.g., thick meconium, fetal heart rate decelerations, known fetal anomalies), appropriate equipment should be set up and ready to use immediately (Box 22-2).
Box 22-2 Neonatal Resuscitation Supplies and Equipment for Delivery of a Term Infant
Modified from Kattwinkel J (ed): Textbook of Neonatal Resuscitation, 5th ed. Elk Grove Village, Ill, American Academy of Pediatrics and American Heart Association, 2006.
The American Academy of Pediatrics and American Heart Association developed specific protocols for neonatal resuscitation (AAP and AHA, 2006). An adapted resuscitation algorithm is given in Figure 22-1. This chapter does not cover the protocol in sufficient detail to produce competency in neonatal resuscitation and should not be used as a substitute for participation in the AAP/AHA Neonatal Resuscitation Program (NRP). The ABCs of neonatal resuscitation are the same as adult resuscitation: clear and position the airway, make sure the infant is breathing (whether spontaneously or with support), and ensure circulation of oxygenated blood.
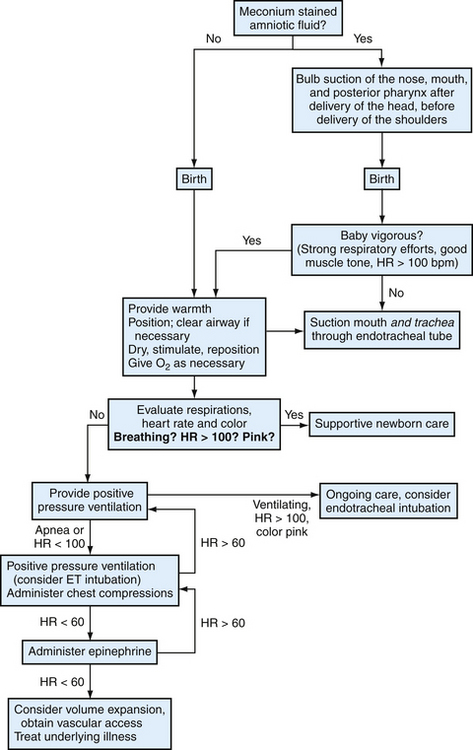
Figure 22-1 Algorithm for neonatal resuscitation. ET, Endotracheal; HR, heart rate.
(Modified from John Kattwinkel J (ed). Textbook of Neonatal Resuscitation. 5th ed. American Academy of Pediatrics and American Heart Association, Elk Grove Village, Ill, 2006.)
Infants should also receive 1.0 mg of vitamin K intramuscularly early after delivery to prevent vitamin K–deficiency bleeding (VKDB, previously hemorrhagic disease of the newborn) (AAP, 2003b; Puckett and Offringa, 2000). Concerns about a correlation between intramuscular (IM) vitamin K and childhood leukemia have not been validated, and there is insufficient data to show that oral vitamin K prevents late-onset VKDB; therefore, IM vitamin K should be administered to all newborns (AAP, 2003b).
The Apgar Score
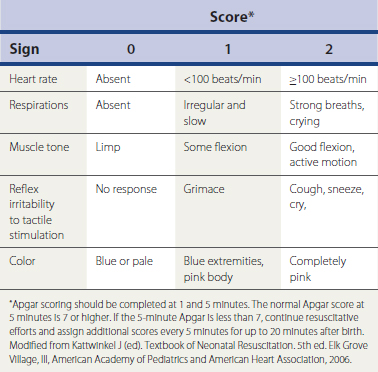
The Apgar score is widely used as a part of the early assessment of the newborn (Table 22-1). A score of 0, 1, or 2 is assigned to each of the five physical signs at 1 and 5 minutes after birth. The Apgar score should not be used as a substitute for assessing the ABCs in neonatal resuscitation, and resuscitation efforts should not be delayed or interrupted to assign an Apgar score. However, the Apgar score does allow a quick and consistent way for different providers to describe an infant’s condition. A score of 7 to 10 is considered normal. If the 5-minute Apgar score is abnormal, less than 7, appropriate resuscitation measures should be continued and Apgar scores assigned every 5 minutes until the infant is stabilized.
Initial Newborn Evaluation
Within the first 12 to 18 hours of life, a comprehensive physical examination should be completed and discussed with the parents. During the examination, the infant should be kept in a comfortable environment. Keeping the infant quiet and calm is important for adequate examination in the newborn period. The examination should begin with observation of activity, skin color, muscle tone, and respiratory effort while the infant is quiet. Listening to the heart and lungs should be completed next, disturbing the infant as little as possible. An infant often begins to cry at the touch of a cold stethoscope or cold hands, making the cardiopulmonary examination particularly difficult. The rest of the examination can then be completed in a calm and thorough manner.
General Appearance
After collecting the history, it is important to observe the calm newborn. The normal term newborn rests with all extremities in some degree of flexion. Breathing should be quiet and effortless, but it can be very irregular. Episodes without breathing lasting 5 to 10 seconds are common and normal in newborns. Skin should be warm to the touch, soft, and smooth. Table 22-2 lists normal vital signs in the first days of life. Box 22-3 lists some common benign findings on the newborn examination. These are generally self-limited and require no further evaluation or treatment in the otherwise asymptomatic newborn.
Table 22-2 Vital Signs in the First Days of Life
| Vital sign | Normal value |
|---|---|
| Heart rate | 100-180 beats/min |
| Respiratory rate | 24-60 breaths/min |
| Systolic blood pressure | 65-90 mm Hg |
| Diastolic blood pressure | 50-70 mm Hg |
| Temperature | <101.4° F (38.0° C) >96.8° F (36.0° C) |
Data from Gunn VL, Nechyba C. The Harriet Lane Handbook, 16th ed, St Louis, Mosby, 2002; Rudolph AM. Kamei RK, Sagan P. Rudolph’s Fundamentals of Pediatrics, 2nd ed. Norwalk, Conn, Appleton & Lange, 1998.
Neurologic Examination and Newborn Reflexes
Genitalia and Anus
The genitalia of the female child should have a visibly patent vaginal orifice, with the labia majora covering the labia minora, clitoris, and vaginal opening. The labia majora should be completely separate from each other (ensuring the absence of labioscrotal fusion). The labia majora should be palpated to evaluate the presence of inguinal hernia or ectopic gonads.
Muscles, Skeleton, and Hips
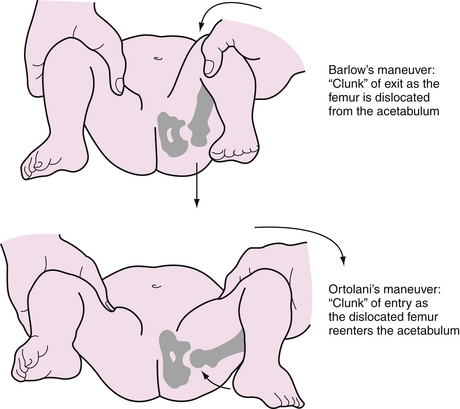
There are two maneuvers in the neonatal hip examination: the Ortolani maneuver and the Barlow maneuver (Fig. 22-2). Each hip should be examined separately using gentle but firm pressure. Too much force can injure the hip in a normal infant.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree