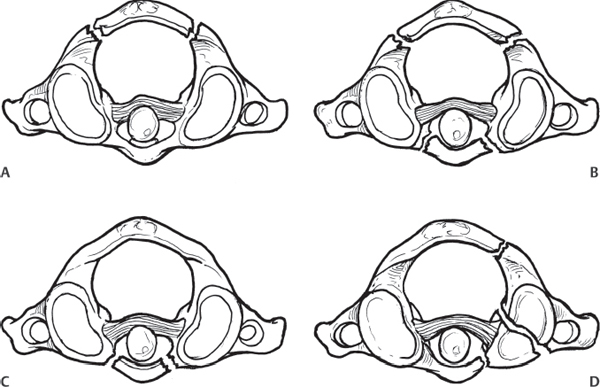
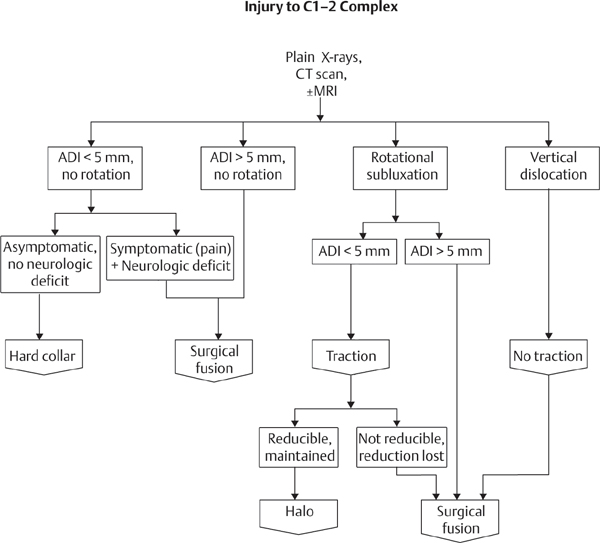
2 Fractures of the C1 vertebra, or atlas, make up 2–13% of all spine fractures and 1–2% of skeletal fractures. C1 ring fractures were first described by Cooper in 1822 but are better known from the descriptions of Jefferson in 1920, whose name is often associated with the four-part C1 ring fracture. Historically, these fractures were thought to be universally fatal, although in reality most fractures were missed until the advent of modern imaging modalities, with many isolated C1 ring fractures recovering without complications. In current practice, over half of C1 ring fractures are associated with other musculoskeletal injuries. The anatomy of the C1 ring is unique and contributes to the typical fracture patterns that are seen. Two arches of bone, one anterior and one posterior, are joined together by two lateral masses to form a ring. Superiorly, the lateral masses support the occipital condyles, and inferiorly they articulate with the upper surface of the axis. The atlas ring surrounds both the odontoid process and the spinal cord. The odontoid process is held firmly to the posterior aspect of the anterior arch of the atlas by the transverse ligament. This complex enables the unique mobility of the head in relation to the spine. The vertebral arteries pass laterally through the foramen transversarium, then curve medially across the posterior/inferior portion of the ring before entering the cranium. Neurologic injuries are rare with isolated C1 ring fractures, because of the ample size of the spinal canal in relation to the spinal cord. There are four basic types of C1 fractures. The most common type is an isolated fracture of the posterior arch (Fig. 2.1A), which accounts for almost two-thirds of all atlas fractures. This injury occurs after forced hyperextension of the skull and cervical spine. The relatively weak posterior arch is compressed between the occiput and the neural arch of the axis. The injury is best seen on a lateral radiograph or sagittal and axial computed tomography (CT) images. Fig. 2.1 (A) A posterior arch fracture; (B) burst (Jefferson) fracture; (C) anterior arch fracture; (D) lateral mass fracture. Burst fractures (Jefferson fractures) (Fig. 2.1B) make up about a third of atlas fractures and result from an axial load applied to the skull. The force is transmitted through the lateral condyles, which fracture and are then forced laterally outward. Classically, there are four breaks in the ring; in front of and behind each of the lateral masses; however, other variations are seen. Severe variants of this injury are associated with a rupture of the transverse ligament, which allows the lateral masses to spread widely. Less common fracture patterns involve anterior arch fractures (Fig. 2.1C) or comminuted fractures of the lateral masses (Fig. 2.1D). Patients with neck pain following trauma should be treated with a high index of suspicion regarding a possible cervical fracture. Initial radiological evaluation includes odontoid (open-mouth), anteroposterior (AP), and lateral views of the cervical spine, which will pick up 80–95% of atlas fractures. CT scans are useful to evaluate the fracture pattern further. A magnetic resonance imaging (MRI) scan is useful for those with associated neurological injuries or suspected ligamentous instability. Fractures of the atlas are considered unstable when the transverse ligament is ruptured. This can be evaluated on plain radiographs by measuring the distance from the lateral edge of C1 to the lateral edge of C2 on both sides on the AP open-mouth radiograph or coronal CT scan. If the sum of these two distances (lateral mass displacement, or LMD) is greater than 7 mm, complete rupture of the transverse ligament is presumed to be present. Approximately 53% of atlas fractures are associated with other spinal fractures. The most common associated fractures involve the odontoid process. Stable, minimally displaced (< 7 mm LMD) atlas fractures are treated by immobilization in a semi-rigid cervical collar or halo vest for 8–12 weeks. Unstable C1 ring fractures can generally be reduced by the application of cranial traction. After 3–6 weeks in traction, when the fracture begins to heal, a halo vest orthosis can be applied for an additional 6–10 weeks. Surgical treatment may be useful for unstable fractures or for polytrauma patients with associated injuries that require early mobilization. Various surgical approaches have been described, including C1–C2 transarticular fixation and occipitocervical (OC) fusion. The treatment of atlas fractures depends on the nature of the fracture and the severity of associated injuries. Patients with isolated, stable fractures generally do well. Those with severe disruption of the joint surfaces of the occiput, C1, and/or C2 may have significant neck pain and stiffness due to post-traumatic arthritis. Most C1 fractures heal with a low associated complication rate. Potential complications include malunion, nonunion, post-traumatic arthritis, greater occipital nerve neuralgia, and injuries to the vertebrobasilar vascular system. Dvorak MF, Johnson MG, Boyd M, Johnson G, Kwon BK, Fisher CG. Long-term health-related quality of life outcomes following Jefferson-type burst fractures of the atlas. J Neurosurg Spine 2005;2(4):411–417 PubMed Long-term follow-up (average 75 months) on 34 patients with Jefferson burst fractures is presented. Patients’ perceived health status had not returned to preinjury levels and was less than that of a comparative normal population. Concomitant injuries and significant bony displacement were associated with poorer outcomes. Kakarla UK, Chang SW, Theodore N, Sonntag VK. Atlas fractures. Neurosurgery 2010;66(3, Suppl):60–67 PubMed A detailed review of atlas fractures, including their incidence, diagnosis, and treatment. Landells CD, Van Peteghem PK. Fractures of the atlas: classification, treatment and morbidity. Spine (Phila Pa 1976) 1988;13(5):450–452 PubMed A review of 35 patients with C1 fractures showed that long-term morbidity is not as low as previously thought, with 13 of 23 patients (56%) followed up a minimum of 1 year posttrauma having significant symptoms of scalp dysesthesia, neck pain, and/or neck stiffness. Levine AM, Edwards CC. Fractures of the atlas. J Bone Joint Surg Am 1991;73(5):680–691 PubMed Thirty-four patients who had fractures of the atlas were reviewed at an average follow-up of 4.5 years. Seventeen patients had bilateral fracture of the posterior arch, six patients had a fracture in the area of the lateral mass, and eleven patients sustained a Jefferson, or burst, fracture. Initial patient management varied depending upon their fracture patterns and confounding injuries. No atlanto-axial instability was evident in any patient at follow-up. Longo UG, Denaro L, Campi S, Maffulli N, Denaro V. Upper cervical spine injuries: indications and limits of the conservative management in halo vest. A systematic review of efficacy and safety. Injury 2010;41(11):1127–1135 PubMed Forty-seven studies including 1078 patients treated in halo vests for C1–C2 fractures were reviewed. A discussion of the safety and efficacy of halo vest is presented. Scher AT. The value of retropharyngeal swelling in the diagnosis of fractures of the atlas. S Afr Med J 1980;58(11):451–452 PubMed A case report discussing the diagnostic value of seeing increased retropharyngeal swelling on plain radiographs and distinguishing a Jefferson fracture from a posterior arch fracture of the atlas. Schlicke LH, Callahan RA. A rational approach to burst fractures of the atlas. Clin Orthop Relat Res 1981; (154):18–21 PubMed Discusses the decision-making process in treating Jefferson fractures, including indications for atlanto-axial arthrodesis. Segal LS, Grimm JO, Stauffer ES. Non-union of fractures of the atlas. J Bone Joint Surg Am 1987;69(9):1423–1434 PubMed Eighteen patients with fractures of the atlas were evaluated clinically by CT at an average of 46 months follow-up to determine the effect of fracture pattern, bony healing, and method of initial immobilization on long-term follow-up. Sherk HH, Nicholson JT. Fractures of the atlas. J Bone Joint Surg Am 1970;52(5):1017–1024 PubMed A review of C1 fracture patterns and classifications. Teo EC, Ng HW. First cervical vertebra (atlas) fracture mechanism studies using finite element method. J Biomech 2001;34(1):13–21 PubMed The authors constructed a detailed three-dimensional finite element model of the human atlas with geometrical data obtained using a three-dimensional digitizer. Then, using material properties from literature, the finite element model was exercised under simulated axial compressive loading stresses to investigate the sites of failure reported in vivo and in vitro. ADI, atlantodens interval; CT, computed tomography, MRI, magnetic resonance imaging
C1 Ring Fractures
![]() Classification
Classification
![]() Workup
Workup
![]() Treatment
Treatment
![]() Outcomes
Outcomes
![]() Complications
Complications
Suggested Readings
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







