CHAPTER 84 Bursitis
INTRODUCTION
It is unlikely that the following discussion will do a great deal to alter the rather menial significance attributed to the bursae:
Ensuring the smooth and frictionless working of the body corporate, usually uncomplaining, inconspicuous, hard-working, and very modest in their requirements, the bursae have been so neglected that, even when one of them misbehaves, this is usually misattributed to some more important structure.30
Olecranon bursitis is the most commonly involved site followed by the bicipital radial bursa. The latter is particularly involved in partial ruptures of the biceps tendon insertion. The presence of these structures is even variable and is probably developmental, because not all bursae are present at birth.43
ANATOMY
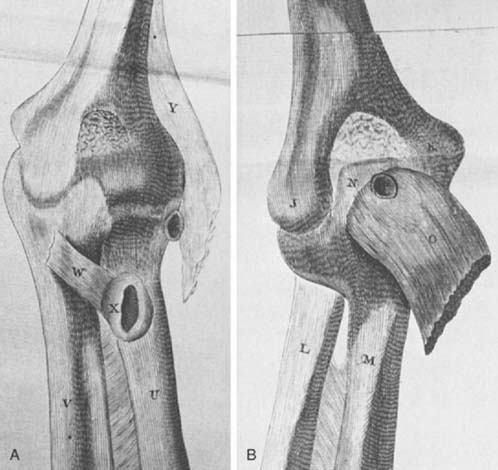
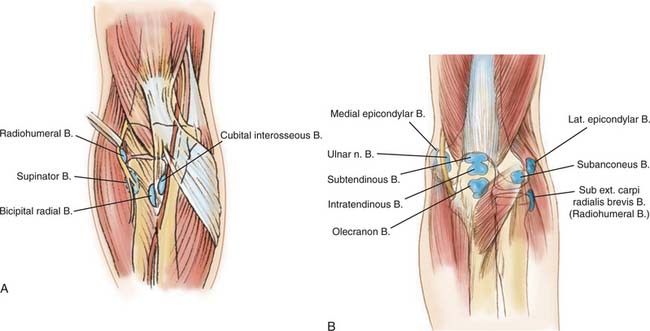
As early as 1788, Monro described several deep bursae about the elbow (Fig. 84-1). Through the years, additional bursae have been described. They may be divided into deep and superficial types (Fig. 84-2). Anatomically, the deep bursae are situated between muscles or between muscle and bone, which makes anatomic recognition somewhat difficult and clinical involvement almost impossible to diagnose. The superficial bursae consist only of those over the epicondyles and that over the olecranon, which is by far the most important one.
DEEP BURSAE
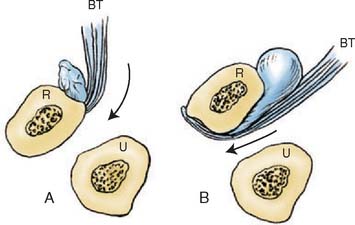
Pathologic involvement of any of the deep bursal structures is rather uncommon. This fact, coupled with the difficulty of identifying some of these structures by anatomic dissection, brings into question the very existence of certain structures. The most significant of the deep bursae is the bicipital radial bursa, which occurs at the radial tuberosity (Fig. 84-3). Owing to its anatomic site, inflammation of the bursa may occur with pronation and supination and can be confused with distal biceps tendinitis.20 Distinguishing between impending distal biceps tendon rupture and bicipital radial bursitis is not simple.1 In fact, one of the few cases of cubital bursitis reported by Karanjia and Stiles showed degeneration of the biceps tendon insertion.20 Crepitus on pronation and supination suggests impending rupture. Fullness or swelling of the cubital space that is accentuated on pronation is more consistent with bicipital radial bursitis.20 I have used selective lidocaine injections to help localize the lesion to the tuberosity, but this does not distinguish between the two processes. Usually the diagnosis is presumptive and the treatment is symptomatic–rest, ice or heat, and anti-inflammatory agents.
Tennis elbow and irritation of the radial nerve have been reported to result from inflammation of the radiohumeral bursa, which lies under the extensor carpi radialis brevis.5 Although bursitis was once thought to be a common cause of tennis elbow, according to our current understanding of lateral epicondylitis the association seems to be uncommon. Yet this structure does exist and has been demonstrated in anatomic dissections.30,31 I have had one patient who developed adventitial epicondylar bursitis after a common extensor tendon slide. Symptoms resolved after excision.
Deep bursae have been associated with the triceps tendon. The significance of the two deep bursae around the triceps (Fig. 84-4) is a matter of speculation, because no recognizable clinical presentation has been documented for these structures. It is possible that inflammation of either the intratendinous or subtendinous bursae could be mistaken for tendinitis or that of the subtendinous bursae for tendinitis, synovitis, or capsulitis. Idiopathic calcific involvement of the subtendinous bursae has been described.41 Yet calcification of bursae around the elbow is distinctly unusual, in contrast to calcific tendinitis in the region of the shoulder. Calcium appears to form in response to anoxia, which causes a cellular response with giant cell reaction. The result is an inflamed, “hot”-looking joint or bursa.
SUPERFICIAL BURSAE
The olecranon and the medial and lateral epicondylar bursae are the only superficial bursae about the elbow. I have occasionally observed an inflamed medial epicondylar bursa associated with chronic subluxation of the ulnar nerve. This probably rather uncommon lesion is treated by attending to the primary pathologic process involving the ulnar nerve. It is interesting to note that the olecranon bursa is not present at birth and has been shown to develop after the 7th year.6 This is consistent with others’ observations that bursae increase in size with age. Spontaneous rupture of the triceps tendon (see Chapter 35) may be related to tendon degeneration, as has been documented with disruptions of the insertion of the bicipital tendon.10 This process could masquerade as bursitis.
OLECRANON BURSITIS
The olecranon is the site of the most common type of superficial bursitis.33 Olecranon bursitis is caused by a number of pathologic conditions that are traumatic (overuse or direct impact), inflammatory, infectious, or noninfectious. Since 1975, it has been associated with dialysis in the ipsilateral extremity.17 I have also observed olecranon bursitis after reconstructive procedures when a posterior approach was used (Fig. 84-5).
Inflammation of the superficial olecranon bursa can also result from direct trauma or repetitive stress, the so-called miner’s elbow or student’s elbow. Larson and Osternig have also shown that olecranon bursitis is a common football injury and is often associated with artificial turf.24
Involvement with systemic inflammatory processes such as rheumatoid arthritis,27 gout, chondrocalcinosis,12 or hydroxyapatite crystal deposition29 has been reported. Diffuse pigmented villonodular synovitis has also been shown to give rise to olecranon synovitis,28 and xanthoma has been reported to involve this region.38 In lesions due to chronic overuse–for example, coal miner’s bursitis–the synovial cells that are least subject to mechanical stress have been shown to be those that elaborate the synovial fluid.26
The distinction between septic and aseptic olecranon bursitis can be somewhat difficult to make. About 20% of cases of acute bursitis have a septic cause.18,38 Distinguishing between a septic and an aseptic inflammatory bursitis has been the subject of a detailed study by Ho and Tice15 and is discussed in Chapter 68. Fever, tenderness, and parabursal cellulitis are common with septic bursitis; however, these findings are not specific, and a more detailed study by Smith and associates revealed that the skin over a septic bursa is almost 4°C warmer than that over the nonseptic contralateral extremity.37 The sepsis causes pain in approximately 80%, whereas nonseptic bursitis is tender in only about 20%. It should be noted that Gram stain results are positive in only about 50% of patients. Approximately 80% are caused by Staphylococcus aureus or another gram-positive organism.44 Particular care must be exercised in evaluating dialysis patients because they may present with a sterile inflammatory process but have pain and warmth that suggest an infection.17 The problem is compounded by the fact that about 20% of these patients are also found to have a septic process.19 The correct diagnosis is suggested when aspirate from the bursa demonstrates a high leukocyte count. Thus, a presumptive diagnosis can usually be made before the culture results have been obtained. Contiguous spread of septic olecranon bursitis leading to osteomyelitis of the olecranon has been thought to be possible, although it is probably rare. Excision of the olecranon has been recommended to avoid this possibility.25
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree