Chapter 12 Buckling: A Biomedical Model of Subluxation
After reading this chapter you should be able to answer the following questions:
| Question 1 | What are the characteristics of spinal motion segment buckling? |
| Question 2 | What factors precipitate spinal motion segment buckling? |
| Question 3 | What factors are required to resolve buckling behavior? |
For over 100 years, the notion of vertebral subluxation has provided a conceptual basis for the chiropractic profession. Throughout that history, there has been little change in the reasoning underpinning the theory of subluxation. Parallel hypotheses have evolved as justifications for treatment by osteopathic and manipulative manual medicine practitioners1 under the terms osteopathic lesion and joint dysfunction, respectively. Acceptance of the subluxation lesion by the broader health care community and health policy makers has been hindered primarily by the absence of tangible evidence of its existence or its mechanism. It has been essentially a heuristic theory explained only by empirical observation and thought experiments. For the profession, the subluxation denotes structural failure altering body function.
Good theory should reliably account for clinical observations. Classical explanations of subluxation do not. Like most advances in health care, breakthroughs are triggered by the accumulation of observations that are not explained within the theory. Early efforts to resolve these apparent conflicts gave rise to the notion of the subluxation complex.2,3 This modification of the traditional theory sought to develop subcategories of mechanisms explaining different symptom subsets but with limited success. Within the past two decades, specific evidence has accumulated to explain the subluxation mechanism with a more complete, biomechanically based theory able to account for clinical observations. This chapter will first review the theoretical inconsistencies followed by more recent evidence that helps to reconcile them.
If science proved tomorrow, that our theory of subluxation was incorrect, it would not alter what I do… I would simply find another theory.4
Inconsistencies of Chiropractic Theory
The fundamental basis of the subluxation hypothesis was set out by Palmer5 and specifies a cascade of events. They are (1) displacement or relative malposition between two vertebra, (2) irritation of the intervertebral spinal nerve, (3) interference of the nerve function, and (4) functional or pathological abnormality in the end organ innervated by the nerve. A direct examination of the first two tenets of the cascade demonstrates inconsistency with clinical and experimental observation.
The clinical observation that fails to be explained by the Palmer cascade is the fact that no reliable relationship has been found between vertebral position and any health disorder, including spine pain. Figure 12-1 shows two patients, one evaluated with a history of repeated episodes of spine pain and one with no spine symptoms. Both were otherwise healthy. It is the patient with the normal appearing spine that has all of the symptoms. Indeed, this observation is a basis for two different schools of thought within the chiropractic discipline. The Logan approach, historically, would be to make every effort to straighten a curvature of the spine simply because it is present. The Palmer approach has been to assert that the spine developed in this manner and for this individual is normal and there should be no intervention to correct the curve.
The work of Frymoyer et al.6 illustrates the dilemma of intervertebral position as a chiropractic premise. Their study was directly targeted to test for such a relationship. Radiographs of the lumbar spine were obtained for various clinical reasons. Each was distributed to both medical and chiropractic radiologists with instructions to identify two features: first, all of the clinically relevant findings, and second, the radiographs of patients with back pain. While the chiropractic participants were much more consistent than the medical providers in identifying factors they believed were clinically important, neither group was any more successful in correctly identifying the patients with spine complaints.
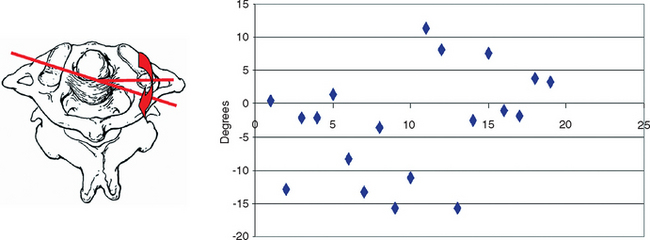
A second problem for the bone position tenet of subluxation comes with modern knowledge of spine biomechanics. However, the influence of biomechanical function on observations could be seen in clinical studies as early as 1982. Schram7 attempted to quantify the change in position of the atlas following treatment. Figure 12-2 shows the typical type of radiographic measure used clinically for position. The location of osseous landmarks is used to determine the orientation of a vertebra with respect to some “normal” position or with respect to an earlier position. The result of treatment was a random orientation of C1 with respect to C2. There was no relationship between the position after treatment either to the pre-treatment condition or to any presumed normal position. In fact, the result appeared to be completely random and could be replicated by computer simulation.
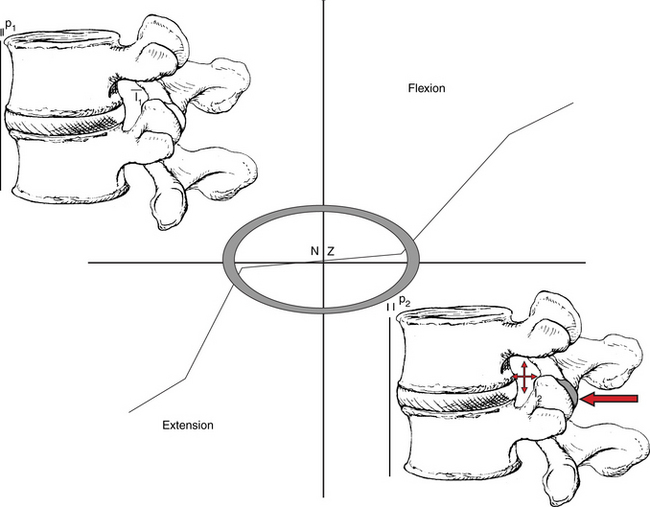
A normal biomechanical phenomenon of vertebral joint function is now known that makes Schram’s results perfectly reasonable. It is the normal presence of the articular neutral zone (Figure 12-3). The neutral zone is a region in which the vertebra will come to rest following a movement. Another description of the neutral zone is that it is a central region where there is almost no resistance from the ligamentous or discal attachments to applied loads. Disproportionately large movements occur within this neighborhood in response to spinal loads compared to outside the region where the resistance from ligaments is engaged. The neutral zone of the atlas is one of the largest of all spinal segments. Under normal circumstances, return of the head to midline following a rotation could leave the atlas rotated to one side or it may overshoot to the other. Such behavior is completely consistent with Schram’s findings of random orientation following manipulation.
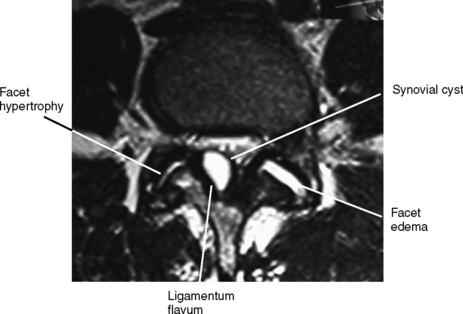
After positional abnormality, the Palmer cascade calls for nerve irritation with altered nerve expression. Other than the appearance of pain, itself an ambiguous symptom, rarely is there clinical evidence of direct nerve root involvement. Similarly, electrodiagnostic studies have been found to show sensitive or specific changes in nerve function at the intervertebral foramina unless pathoanatomical disease is present. The most common diseases that produce such changes include chemical neuritis associated with internal disc derangement, stenosis, and disc protrusion. Indeed, imaging studies may show significant effacement of the dura or deformity of the nerve root without any reliable change in nerve amplitude, conduction velocity, or reflex response (Figure 12-4).
In the absence of consistent evidence for nerve root involvement, supplemental theories have been developed to offer mechanisms of altered proprioception and reflex changes as a basis for the claim of nerve irritation. Some evidence exists to support these ideas; however, they fail to represent mechanisms of true nerve irritation. Rather, they are normal physiological responses to altered mechanical joint behavior as with changes in proprioceptor firing rates. Whether such changes, if they occur, are persistent or accommodate with time are unknown. Reflex responses may also vary,8–12 but they represent secondary mechanisms that are not consistently found in patients.
Various alternative explanations have been proposed that attempt to describe the different clinical presentations that patients have. (See Chapter 10.) They include such factors as entrapped synovial tags or joint menisci and local muscle spasm. Both accounts might explain pain and are intended to give a basis for how the lesion persists. Menisci are hypothesized to create a blockage of the joint, and local spasm restricts motion. Joint adhesions may develop to chronically block motion or cause it to be asymmetrical. Inconsistencies, however, remain. Menisci do exist.13 However, because motion opens and closes the joint depending on the direction, it is not clear why an entrapped meniscus is not released with an alternate movement. Local muscle tension may exist for some; however, it has not been shown to occur uniformly. Moreover, muscles fatigue. What keeps the tension and prohibits motion then? Inflammatory conditions do cause adhesions in and around connective tissue. However, the organization of granulation tissue that yields adhesions takes time. What process retains the necessary conditions long enough?
Lantz2,3,14 and Mootz15,16 contributed to alternative reasoning, adding to the structured picture entitled the subluxation complex. (See Chapter 9.) This portrayal is useful since it collects the symptomatology and purported mechanisms frequently encountered into common manifestations involving muscle (myopathology), swelling, redness and inflammation (vascular pathology), scar formation (connective tissue pathology), and neural changes (neuropathology). The consolidation, however, fails to explain the underlying mechanism of the lesion or the wide variation in the clinical presentations observed in practice. Moreover, neither the traditional subluxation theory nor the revised subluxation complex account for the clinical experience of patients with known organic pathology17,18 (Box 12-1) who may respond to spinal manipulation or adjustment.