CHAPTER 13 Biomechanics of glenohumeral bone loss and treatment mechanics
 The critical width of an anterior glenoid defect is at least 20% of the glenoid length or 25% of the glenoid width.
The critical width of an anterior glenoid defect is at least 20% of the glenoid length or 25% of the glenoid width.Shoulder stability and the glenoid and humeral osseous defects
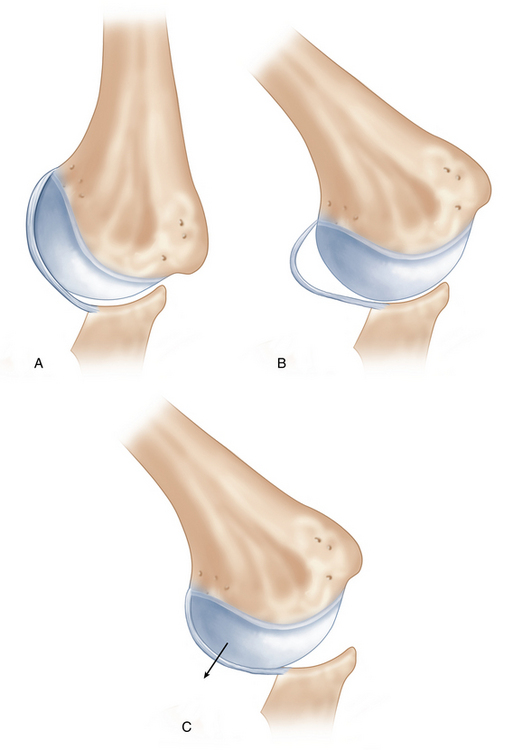
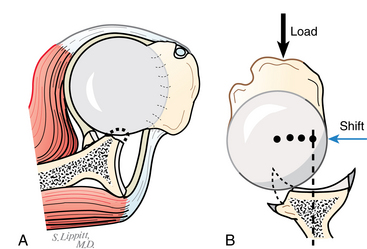
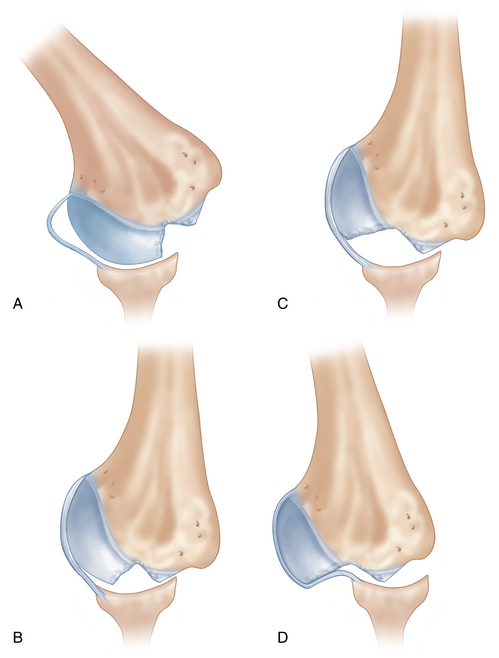
Several authors have reported that both the glenoid and humeral osseous defects cause instability problems in different arm positions.1,2 Although there is a large glenoid bony defect, the shoulder is stable at the end–range of motion as long as the capsule is repaired because the repaired capsule is tight and prevents the anterior shift of the humeral head (Fig. 13-1, A). However, in the mid–range of motion, the capsule becomes lax (Fig. 13-1, B), and the humeral head slips out of the glenoid socket because the socket is very shallow as a result of the bony defect (Fig. 13-1, C). In other words, a glenoid defect causes the mid-range instability, but not the end-range instability.3 The mid-range stability is mainly provided by the glenoid concavity and the compressive force generated by the surrounding muscles (concavity-compression effect) (Fig. 13-2). The presence of a glenoid defect impairs this concavity-compression effect, which causes instability in the mid–range of motion. On the other hand, a Hill-Sachs lesion is the opposite: it causes no instability in the mid–range of motion because the mid-range stability is provided by the glenoid concavity and muscle contraction force, both of which are intact (Fig. 13-3, A). At the end–range of motion, if the Hill-Sachs lesion is still covered by the glenoid, it causes no instability (Fig. 13-3, B). However, if the lesion is larger than the glenoid (Fig. 13-3, C), it engages with the anterior rim of the glenoid and the humeral head dislocates (Fig. 13-3, D). Therefore, a Hill-Sachs lesion causes the end-range instability, but not the mid-range instability. This is an important concept in understanding glenohumeral bone injuries.
Glenoid osseous defect
Recently, computerized tomography (CT) has been recognized as a suitable imaging modality compared with conventional radiography in evaluating glenoid abnormalities associated with glenohumeral instability. Sugaya et al4 evaluated the morphology of the glenoid rim in 100 consecutive shoulders with unilateral recurrent anterior dislocations on three-dimensional (3-D) CT images. Surprisingly, 90% of the shoulders showed bony deficiency of the glenoid, 50% with a fragment-type defect and 40% with an erosion-type defect.
Which size of the glenoid osseous defect should be treated?
Previous studies
Lo et al5 from their clinical experience defined a large osseous defect of the glenoid that required bone grafting as one that was a minimum of 25% to 27% of the entire width of the inferior portion of the normal glenoid. To date, there have been only two biomechanical studies3,6 to clarify the critical size of a glenoid defect. We demonstrated that an osseous defect with a width that was at least 21% of the glenoid length might cause instability even after Bankart repair (Fig. 13-4).3 It is amazing that 21% of the glenoid length (north-to-south distance), which we call the critical size of the defect from our biomechanical study, is very close to 25% of the glenoid width (east-to-west distance), which Lo et al call the critical size from their clinical experience (Fig. 13-5). Gerber et al6 also clarified in a cadaveric study that an anteroinferior glenoid lesion involving a loss of more than half of the glenoid width leads to a loss of dislocation resistance of more than 30%. These figures have been clinically used as an indication for bone grafting. However, these studies were performed on the assumption that the glenoid osseous defect was located anteroinferiorly.
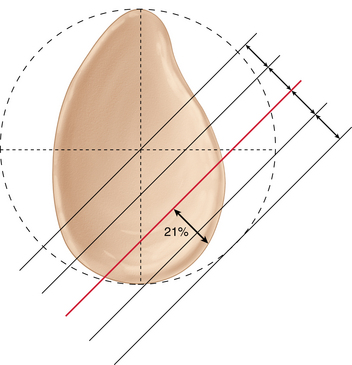
FIGURE 13-4 Critical size of the glenoid osseous defect. Our biomechanical study3 demonstrated that an osseous defect with a width that was at least 21% of the glenoid length might cause instability even after Bankart repair.
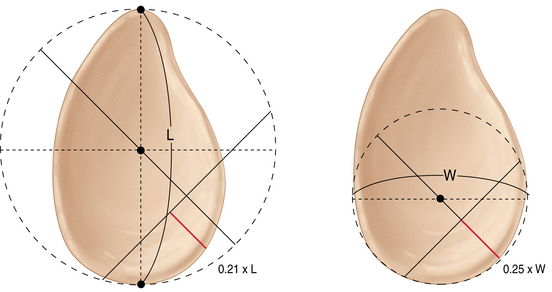
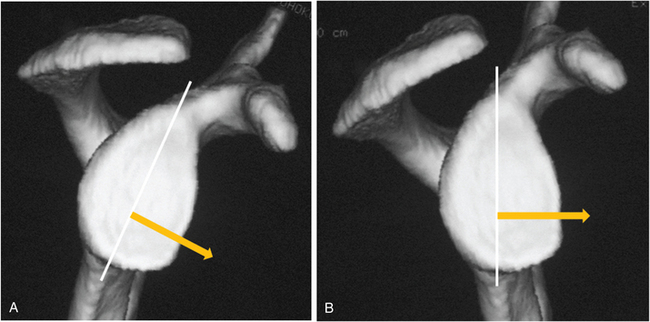
FIGURE 13-5 Critical size from the biomechanical study3 and from the clinical experience.5 It is interesting that 21% of the glenoid length (north-to-south distance or the diameter of the outer fitting circle), which we call the critical size of the defect from our biomechanical study, is very close to 25% of the glenoid width (east-to-west distance or the diameter of the inner fitting circle), which Lo et al. call the critical size from their clinical experience. L, Glenoid length; W, glenoid width.
The glenoid osseous defect is located anteriorly rather than anteroinferiorly
It is generally thought that a glenoid osseous defect is located anteroinferiorly from surgical or radiographic findings. All previous clinical5 and biomechanical3,6 studies evaluated the effect of the glenoid defect on stability based on this assumption. Griffith et al7 was the first who investigated the location of osseous defects with use of CT. No studies have described the precise location of the osseous defect of the glenoid except for our recent study.8 We investigated the location of the glenoid defect in 123 patients with anterior instability using 3-D CT and found that the mean orientation of the defect was pointing toward 3:01 on the clock face of the glenoid. The defect was proved to be located anteriorly relative to the glenoid because of the anterior inclination of the glenoid in the sagittal plane relative to the trunk (Fig. 13-6).
Which size of the glenoid osseous defect should be treated?
Recent studies
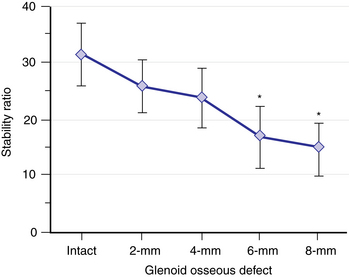
Since the true location of the glenoid is anterior, we need to reevaluate the effect of bony defect of the glenoid on anterior shoulder stability. We performed a biomechanical study using fresh cadavers to clarify the critical size of anterior glenoid defect.9 An osseous defect was created stepwise with a 2-mm increment of the defect width. The stability ratio,10 defined as the peak translational force divided by the applied compressive force, was used to evaluate joint stability. The stability ratio at 3 o’clock was 32% ± 6% (mean ± SD) without a glenoid defect, which gradually decreased with an increase of the defect size (Fig. 13-7). The stability ratio significantly decreased after creating a 6-mm defect (p < .004) compared with that of the intact glenoid. A 6-mm defect was equivalent to 20% ± 1% of the glenoid length or 26% ± 2% of the glenoid width. Our results suggest that reconstruction of the glenoid concavity might be necessary in shoulders with an anterior glenoid defect of at least 20% of the glenoid length. However, this study was performed after removing all the soft tissues including the labrum and the capsule: we checked the effect of bony defect on bony stability without soft tissue contribution. Therefore, we performed a similar biomechanical study in another set of cadavers but with soft tissue contribution taken into consideration.11 This study also showed that a 6-mm defect was the critical size of an anterior glenoid defect, which was equivalent to 19% of the glenoid length or 25% of the glenoid width in this group of cadaveric shoulders. From all these studies, we conclude that the critical size of the glenoid defect is equivalent to 20% of the glenoid length, which is equal to 25% of the glenoid width (Fig. 13-8).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree