Benign Bone Tumors
Bruno Fuchs and Peter S. Rose
Key Points
• Many benign tumors about the hip require only observation and reassurance.
• The aggressiveness of treatment is matched to the aggressiveness of the tumor.
• Surgical treatment for benign tumors most commonly consists of curettage or marginal excision.
Introduction
Benign bone tumors about the hip and pelvis represent a varied group of rare lesions. As benign entities, they are characterized by autonomous growth but lack the ability to metastasize. Therefore benign tumors may be thought of as a local but not a systemic problem. Benign tumors around the hip are most common in young patients and on average affect males more frequently than females, although they may occur at any age.
Dr. Silverstein in Chapter 49 reviewed the evaluation and common features of tumorous conditions presenting about the hip. This chapter will review treatment modalities for patients presenting with benign tumors with specific recommendations for commonly encountered benign tumors. In contrast to patients presenting with malignancies, those with benign tumors in general require less aggressive/less radical treatment. Additionally, the role of adjuvant chemotherapy or radiotherapy is rare in the treatment of benign conditions.
Evaluation
Patients are evaluated as outlined by Dr. Silverstein in Chapter 49. Many benign conditions have characteristic imaging features and do not require biopsy. For example, nonossifying fibroma and enchondroma are conditions that are diagnosed generally by imaging modalities alone. Occasionally, biopsy will be necessary and should be carried out in keeping with the principles outlined in Chapter 49. The key feature of biopsy requires that minimal tissue be contaminated, and that the biopsy tract be excisable by a limb salvage procedure should a primary sarcoma requiring en bloc resection be diagnosed.
Occasionally, benign conditions will present in a multifocal manner. For example, patients with hereditary multiple exostoses or Ollier’s syndrome will present with disseminated benign tumors. These patients usually are detected on physical examination and by history to clue the clinician into the presence of multifocal lesions. Additionally, standard radiographs of the pelvis and femur would usually alert the clinician to the presence of more than one lesion. If a multifocal process is suspected, it is appropriate to obtain a baseline skeletal survey or bone scan to obtain an initial characterization of the extent of the process. Although benign, these processes often have a predisposition to malignancy.
Most benign conditions that arise about the hip are unifocal. Once the diagnosis of a benign tumor about the hip has been established, a careful treatment plan is tailored to the patient. This plan considers the anatomic location and extent of the lesion, its histology and accordant predicted biological behavior, the patient’s expectations and needs, and available surgical and other treatment options. Many benign conditions do not require surgery and can be observed or treated by lesser means. It is rare for benign conditions to require major reconstructive techniques, which would compromise patient function.
Treatment Options
A variety of treatment options are available for patients with benign conditions. They may be summarized as follows:
3. Injection/percutaneous treatment
4. Radiofrequency or cryoablation
5. Curettage with or without adjuvant treatment
These treatment techniques are tailored to the individual patient’s condition. We will discuss each option and will provide clinical examples of how these treatments may be used in individual patients. Treatment protocols for common benign lesions will follow.
Watchful Waiting
A large number of benign conditions around the hip can be identified and characterized as benign on the basis of their imaging characteristics. Many do not require surgical treatment. For example, a nonossifying fibroma/fibrous cortical defect diagnosed about the hip joint is typically found asymptomatically and requires no specific treatment. Another example of this would be an enchondroma. These conditions rarely if ever require surgical treatment; however, they should often be observed through serial imaging to ensure stability of the process. For example, as outlined in Chapter 49 by Dr. Silverstein, low risk is often present for a lesion that initially appears to be an enchondroma to develop into a low-grade chondrosarcoma. Patients who present with imaging studies that implicate an enchondroma are recommended to undergo serial radiograph examinations to ensure stability of the lesion. Experience shows that the risk of pathologic fracture through incidentally detected lesions of this nature is quite low.1 Other benign lesions that are commonly observed include small osteochondromas that are not causing mechanical problems.
Medical Therapy
Many benign conditions may not require interventional management but may benefit from drug therapy. For example, bisphosphonates may be used in the treatment of patients with fibrous dysplasia.2 The classic medical management of osteoid osteoma involves the use of aspirin, nonsteroidal anti-inflammatory drugs, or cyclooxygenase (COX)-2 inhibitors. Medical therapy may be used in patients who have benign conditions that can have both active and latent phases. Medical therapy thus is used to alleviate symptoms until the condition “burns itself out.” Drug therapy provided in this manner allows alleviation of symptoms without the morbidity and risk associated with an interventional procedure.
Injection Therapy
Various benign conditions may be treated with percutaneous injection therapy. For example, unicameral bone cysts are thought to respond to a variety of injection techniques.3,4 Methylprednisolone injection is commonly administered and in a randomized trial was superior to injection of bone marrow aspirate for unicameral bone cysts.5
Injection therapy is generally provided under computed tomography (CT) or fluoroscopic guidance. These treatments offer the benefit of low risk for any individual procedure; however, multiple procedures are often necessary. Technical considerations around providing injection therapy include the use of radiopaque injectate to ensure that intravenous injection is not occurring within the bone. As well, patients may require a period of non–weight bearing to allow healing of the lesion as the treatment takes effect. Therefore these treatments are used more commonly in pediatric patients than in adults.
Selective embolization may be categorized under injection therapy. Embolization can be used as an adjunct in the treatment of benign lesions around the hip and pelvis. For example, data are available to support the role of serial embolization of patients with giant cell tumors that are found in surgically inaccessible areas.6
Radiofrequency Ablation/Cryoablation
Benign lesions may be ablated with the use of thermal techniques (heat via radiofrequency ablation or cold via cryoablation). The classic lesion amenable to this is an osteoid osteoma. Previously, osteoid osteomas were treated by open surgical means to excise the nidus. Experience has demonstrated that ablation of the nidus via percutaneous radiofrequency ablation provides excellent and immediate pain relief for patients.7,8 Percutaneous ablation procedures are generally performed under CT guidance using a minimally invasive approach. A guide wire is placed in the desired location on the skeleton, and then a cannulated drill is used to bridge the cortex and advance the ablation probe (Fig. 50-1). This procedure is safe and well tolerated; it is usually performed under sedation or light general anesthesia on an outpatient basis. Careful shielding is necessary to minimize necrosis of the surrounding skin.
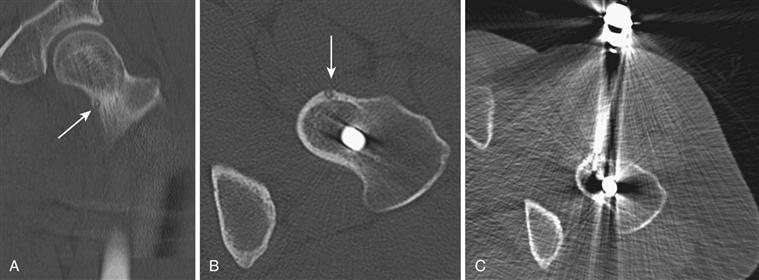
Figure 50-1 Radiofrequency (RF) ablation of an osteoid osteoma of the femoral neck. The patient had been treated erroneously with a sliding hip screw for a presumed stress fracture. A, Coronal computed tomography (CT) and (B) axial CT demonstrate a characteristic nidus. C, RF ablation resulted in immediate pain relief.
Recurrence rates following percutaneous ablation may approach 15%; however, these recurrences generally are readily handled with repeat ablation procedures and are usually due to suboptimal placement of the initial ablation catheter. Note that in lesions that are juxta-articular to the hip joint, a transient hemarthrosis may occur post procedure. This usually causes only temporary discomfort for the patient.7,8
Curettage
Curettage of benign bone lesions is usually coupled with grafting of the curettage cavity and has high efficacy in reducing painful symptoms.9 Curettage is the most common open surgical treatment for benign bone tumors. It is usually performed for active tumors such as giant cell tumors or chondroblastomas or for select eosinophil granulomas that are causing significant symptoms. The surgical approach for curettage is determined by the anatomic location of the lesion. In general, the most direct access point is chosen; this results in minimal damage to surrounding tissues. A direct lateral approach is used most commonly for lesions about the trochanteric region; surgical hip dislocation may be entertained for careful access to juxta-articular lesions.
Curettage is most commonly performed open with wide exteriorization of the lesion to provide good visualization and access to the lesion. Surrounding soft tissues are draped away to minimize contamination and implanting of tumor seeds (Fig. 50-2). Alternatively, less invasive techniques may be applied with curettage performed under fluoroscopic guidance and arthroscopy equipment used subsequently to evaluate the cavity, which is formed to detect residual tumor (Fig. 50-3).
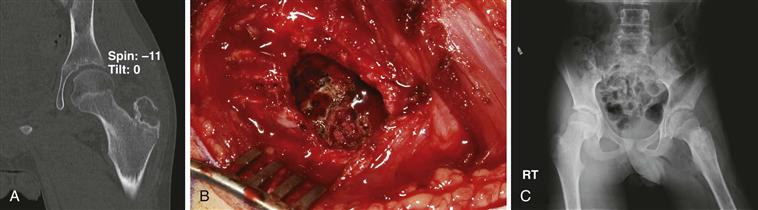
Figure 50-2 Open curettage of a chondroblastoma of the trochanteric apophysis. A, Coronal computed tomography (CT) demonstrates a lesion. B, Wide exteriorization of the lesion is performed. C, Radiograph demonstrating allograft incorporation.

Figure 50-3 Fluoroscopically guided curettage of cystic fibrous dysplasia of the hip with grafting and internal fixation. A, Preoperative computed tomography (CT) image. B, Fluoroscopically guided curettage. C, Postoperative image.
A variety of grafts may be used to fill the curettage defect; those chosen usually vary with surgeon preference and patient wishes.10 Autogenous graft is clearly the gold standard for these purposes; however, it is of potentially limited supply and is associated with harvest morbidity. Additionally, if autograft is used in the treatment of benign bone tumors, the surgeon should carefully segregate the instruments and the operative field of the bone graft harvest from the bone graft of the lesion itself to minimize the theoretical risk of transplantation of benign tumors from one area to another.
In addition to autograft, cancellous and corticocancellous allografts, as well as calcium sulfate and other bone graft substitutes, are successfully employed in the treatment of these lesions4,11,12 (Fig. 50-4). Although potentially attractive, the role of recombinant bone morphogenetic protein (BMP) has not been established in the treatment of benign bone lesions. Because BMP acts as a transcription factor and can potentially activate residual tumor cells, its use is relatively contraindicated in the treatment of benign bone tumors.

Figure 50-4 Calcium sulfate pellets used to treat a benign bone cyst. A, Preoperative computed tomography (CT). B, Postoperative radiograph.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








