Thomas S. Thornhill
Balancing the Flexion and Extension Gaps in Revision Total Knee Arthroplasty
INTRODUCTION
Instability is a major reason for failure of total knee arthroplasty (TKA).1,2 During primary TKA, failure to obtain a knee that is equally balanced in flexion and extension can lead to instability. This can result in a knee that is painful and often functionally unstable. Likewise, in order for a revision TKA to be successful, the flexion and extension gaps must be equally balanced. In revision TKA, however, dealing with osteolysis, significant bone loss, and an often-compromised soft tissue envelope can make soft tissue balancing even more challenging.
Revision knee surgery encompasses a wide variation in complexity, from the relatively straightforward revision with little or no bone loss to those with severely compromised bone stock and ligamentous structures. While the results of revision TKA do not yet rival the success obtained with primary TKA, the outcome and success continue to improve.3–7 Obtaining a knee that is balanced in flexion and extension is an absolute requirement in order to have a successful result. The purpose of this chapter is to detail the surgical principles and techniques involved in order to achieve flexion and extension balance in revision TKA.
PREOPERATIVE PLANNING
Preoperative planning is one of the most critical steps in revision TKA.8–11 Prior to undertaking any revision surgery, regardless of its complexity, it is imperative to have a comprehensive preoperative plan. A thorough plan should include
- Identifying and understanding the mechanism and reason(s) for failure of the arthroplasty
- Obtaining and reviewing adequate radiographs as well as previous operative reports and identifying the brand of component in place
- Determining what important anatomic structures are absent, in jeopardy, or malfunctioning (skin, extensor mechanism, bone, ligaments)
- Being familiar with the revision system and assuring proper inventory of components and instruments
TKA can fail for several reasons. Instability, infection, polyethylene wear, osteolysis, aseptic loosening, arthrofibrosis, and periprosthetic fracture are some of the most commonly stated reasons for failure.1,2 By not properly identifying the reason for failure preoperatively, one may often inadvertently make the same mistakes or fail to correct previous problems at the time of revision.12–14 The results of revision TKA in which the mechanism of failure could not be identified are suboptimal.15,16 The reason for failure can often be determined by a thorough preoperative exam, laboratory studies, and evaluation of serial radiographs.
Adequate radiographs are the cornerstone of a comprehensive preoperative plan. Serial x-rays taken over the life of the implant may provide subtle clues as to the mechanism of failure. When plain radiographs fail to show the mechanism of failure, alternative imaging may be useful, including bone scintigraphy, CT scan that can be used to assess component rotation or osteolysis, and MRI techniques that allow for metal artifact suppression can be useful for assessing bone loss and osteolysis that may be underestimated or undetected on plain radiographs.17
Once adequate radiographs and the mechanism of failure have been identified, it is important to identify what anatomic structures are absent, in jeopardy, or malfunctioning. This requires a detailed physical examination focusing on the skin, presence of effusion or crepitus, integrity of musculotendinous units, and the existence of ligamentous instability. The presence of flexion instability should be noted, as this can be a reason for pain, instability, and failure, which is often overlooked if not specifically evaluated.18
Finally, one must assure that proper inventory is available for the case. This should include not only the planned implants and instruments but also bone graft, and possibly a cement removal system. Obtaining the original operative report and identifying the component in place are mandatory. A large variety of modular revision implant systems are currently available. Many have a multitude of options including modular augmentations, cemented or cementless stems, and various levels of prosthetic constraint. Use of these modular systems allows the surgeon to build the appropriate prosthetic component intraoperatively to solve deficiencies found during the revision TKA.
BASIC PRINCIPLES OF FLEXION AND EXTENSION GAP BALANCING
The surgical goals of a revision TKA are the same as those of a primary TKA: restoration of alignment and stability of the joint in all planes. Similar to the primary knee arthroplasty, the principles of obtaining an equally balanced flexion and extension gaps are also the same.
Classically, nine permutations of flexion and extension gap balancing have been described (Fig. 43-1). Each permutation highlights an asymmetry in the flexion/extension gap balance along with the method of achieving balance through resection of bone or component augmentation. While it is important to understand the concepts of each situation in flexion and extension balancing, rather than memorizing each permutation and solution, it is more helpful in the revision setting to understand the role of the proximal tibia, the distal and posterior femur, and the position of the joint line as they relate to flexion and extension gap balancing.
In general, three rules apply, namely, the extension space is determined by the distal femur, which sets the position of the joint line. The flexion space is determined by the posterior condyles of the femur. The proximal tibia affects both the flexion and extension space.
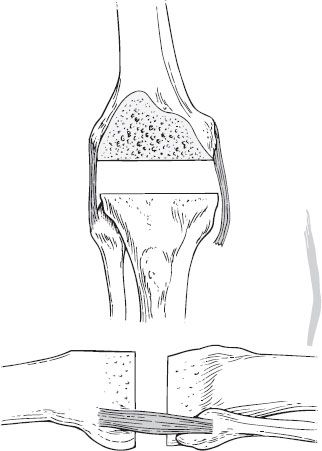
The Proximal Tibia The relationship of the proximal tibia to the flexion and extension space is based on the size of the gap between the proximal tibial and the distal femur with the knee in full extension (Fig. 43-2) and the position of the proximal tibia to the posterior condyles of the femur with the knee in 90 degrees of flexion (Fig. 43-3). As a result, any change in the height or thickness of the proximal tibia will affect both the flexion and extension spaces.
Depending on the severity of bone loss associated with either component removal or osteolysis, the proximal tibia may require bony or metal augmentation to restore flexion and extension balance. Rarely in the revision setting is resection of more tibial bone required other than minimal removal to form a smooth and stable platform perpendicular to the mechanical axis of the tibia.
The Femur The femoral side should be thought of as two distinct entities, the distal femur and the posterior femur, each affecting the flexion and extension gaps respectively.
The distal femur as it relates to the proximal tibia affects the balance of the knee in extension. One can assume that with removal of the femoral component and cement, some bone loss has occurred at the distal femur. As a result, this will increase the extension gap. If this loss is not accounted for at the time of revision, then instability in extension and joint line elevation can exist.
The flexion gap is determined by the relationship of the proximal tibia to the posterior condyles of the femur in flexion. Restoration of the appropriate posterior condylar offset (Fig. 43-4) is important to allow adequate tensioning of the collateral ligaments in flexion and prevent instability. A knee that is too tight in flexion (loss of range of motion [ROM]) is often due to overstuffing of the flexion space, due either to an increased posterior condylar offset or, more commonly, the use of a thicker tibial insert to compensate for a loose extension gap. In cruciate retaining TKA, a tight posterior cruciate ligament (PCL) can also cause flexion tightness. The appropriate posterior condylar offset can be restored by increasing the anterior/posterior dimensions of the femur (larger femoral component) with the addition of posterior condylar augments to fill the flexion space.
The Joint Line In conjunction with obtaining equal flexion and extension gaps during revision, restoration of the joint line will provide stability throughout a full ROM if the components are placed at or near their normal anatomic location. In general, the distal femoral joint line is roughly 25 mm from the medial epicondyle and 30 mm from the lateral epicondyle to the distal aspect of the femur, landmarks that generally tend to be preserved even in the setting of severe bone loss. Additionally, the joint line lies 15 to 18 mm distal to the femoral origin of the PCL or on a lateral radiograph, at approximately the lower pole of the patella.
In revision TKA, joint line elevation occurs as bone is lost from the distal femur. This is commonly associated with osteolysis, aseptic loosening, migration of the femoral component, and bone loss associated with component removal. Reconstruction of the normal anatomic joint line requires the use of bone graft, cement, or metal augmentation to support the femoral component in its correct position. Failure to properly restore the joint line during primary and revision TKA has been associated with instability, pain, and early failure.19 Elevation of the joint line, the most common error, can result in patellar infera and inferior patellar pole impingement, hyperextension/recurvatum with quadriceps weakness and midflexion instability.
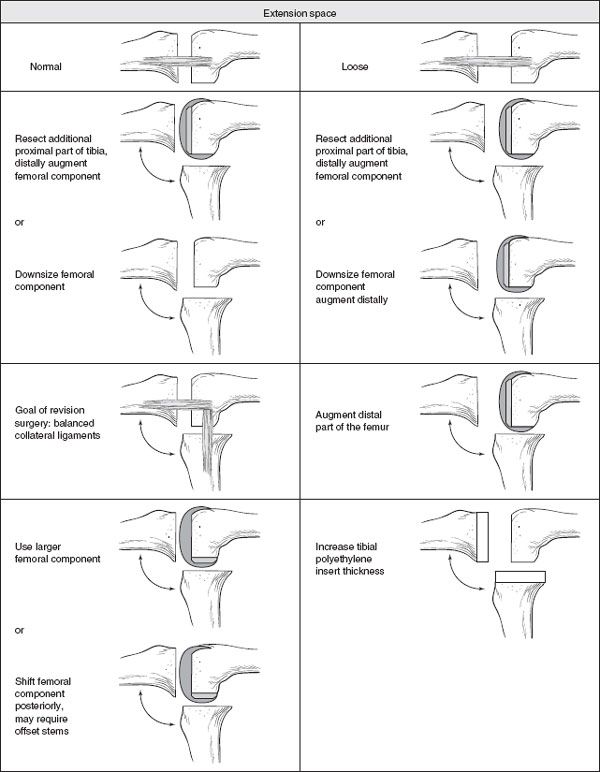
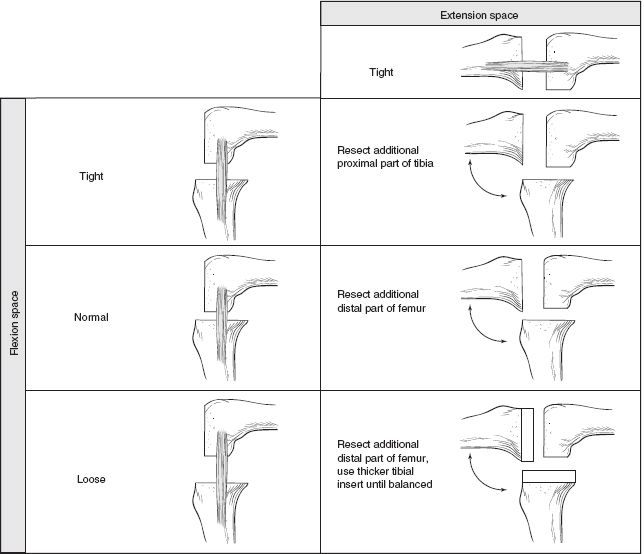
FIGURE 43-1. Nine permutations of flexion and extension gap balancing in revision total knee arthroplasty. (Reprinted from Ries MD, Haas SB, Windsor RE. Soft-tissue balance in revision total knee arthroplasty. Surgical technique. J Bone Joint Surg 2004;86-A(Suppl 1):81–86, with permission.)
Midflexion instability occurs most often in a patient with a preoperative flexion contacture. In order to restore full extension, more bone is often erroneously removed from the distal femur. Stability in extension is then achieved by tight posterior structures, including a contracted posterior capsule, rather than from normally tensioned collateral ligaments. As the knee flexes, the posterior capsule becomes lax, the collateral ligaments remain loose due to elevation of the joint line, and the knee is unstable in midflexion. This can be prevented by recognition of tight posterior structures, release of the contracted posterior capsule, and avoidance of overresection of the distal femur, which results in an elevated joint line. Additionally, midflexion instability can result from the knee that is lax in flexion. A tight extensor mechanism in flexion will often compensate for this instability. As the knee is extended, however, the extensor mechanism loosens and midflexion instability results.
It is important to note that, on occasion, elevation of the joint line cannot be avoided. Achieving adequate extension is some cases must occur at the expense of an elevated joint line. Most commonly, this occurs in knees with significant preoperative flexion contractures with excessive scarring. In these instances, a release of tight posterior structure alone is not enough to allow full extension, and a combination of posterior capsular release with joint line elevation is required. In cases in which substantial joint line is unavoidable, consideration of PCL substation is wise and has been found to be better tolerated.20
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








