Douglas A. Dennis
Robert T. Trousdale
Avoidance and Management of Intraoperative Complications in Revision Total Knee Arthroplasty
INTRAOPERATIVE FEMORAL FRACTURES
INTRAOPERATIVE TIBIA FRACTURES
INTRAOPERATIVE PATELLA FRACTURE
PATELLAR LIGAMENT AND QUADRICEPS TENDON INJURY
INTRODUCTION
Total knee arthroplasty (TKA) is a highly successful procedure with excellent functional outcomes. Analysis of results of TKA have demonstrated a 93% to 97% survivorship at 11 years, with 88% to 96% of patients having good or excellent HSS scores.1–3 This procedure, however, is not without complications. Even for the experienced surgeon, the possibility of perioperative complications always exists. The focus of this chapter is to describe the intraoperative complications of revision TKA, methods to avoid these complications, and management of these complications upon occurrence.
Although there are factors that are sometimes beyond the surgeon’s control, the responsibility of good surgical technique always rests within the hands of the surgeon and will minimize the risk of intraoperative complications. Knowledge of the local anatomy allows the surgeon to appropriately plan preoperatively and determine which type of implants to use. Anticipation of possible complications at each step of the operation will encourage the surgeon to proactively protect vital structures and to avoid damaging them with careless technique.
TKA cannot be performed by the surgeon alone and requires a choreographed team effort. Trained surgical assistants are important for providing adequate exposure and for protecting vital neurovascular structures. Retractor placement should be dictated by the surgeon, and assistants should be trained to know the appropriate amount of force that may be placed on each retractor. Communication is critical between team members throughout the operation. Each team member should understand the sequence of events and know their specific role at each step of the operative procedure.
In the setting of revision TKA, the surgeon’s awareness should be heightened for the possibility of intraoperative complications. Extensive scarring and vague delineation of anatomical structures are typical in revision knee exposures. Difficult exposures may result in avulsion of important structures if care is not taken to systematically perform appropriate releases and to utilize extensile approaches4–15 if necessary. Component removal must be performed carefully to minimize bone loss and the possibility of intraoperative fracture. Removal of cement is often painstaking for the surgeon, but patience and careful technique minimize the possibility of bone loss, cortical violation, or even fracture. Revision TKA is commonly coupled with osteolysis, which amplifies the risk of avulsion of ligaments and tendons, or intraoperative fracture. Placement of stemmed components can lead to iatrogenic fracture if care is not taken during bone preparation or implant selection.
Minimally invasive TKA has continued to gain popularity, perhaps secondary to expectations of patients, as well as marketing influences. As with any new technique, a learning curve exists and the incidence of complications is not insignificant. Component malpositioning16 iatrogenic ligament injury and even vascular injury leading to amputation are all complications that have occurred due to poor exposure and compromised technique in total joint arthroplasty.17 Although some studies have revealed some short-term benefits of the minimally invasive technique (decreased pain, less blood loss, quicker recovery, and shorter hospital stay), one should always remember that the exposure should never compromise the surgeon’s ability to perform a technically sound operation.
With experience, a surgeon not only develops the craftsmanship skills of handling instruments necessary to perform a TKA but also gains an awareness of possible complications that may occur at each step and develops a sound sense of judgment when critical decisions need to be made intraoperatively. In an academic or instructional setting, the possibility of intraoperative complications may be increased if the surgeon in training is yielded technical responsibilities prematurely.A lack of understanding of the anatomy combined with inexperienced instrument skills can lead to unanticipated complications. There exists a careful balance of allowing the surgical apprentice to perform steps that are necessary to nurture his or her skills while identifying his or her individual limitations, all in the context of providing the patient with an excellent total knee replacement.
INTRAOPERATIVE FEMORAL FRACTURES
A classification system described by Lewis and Rorabeck18–20 was designed for the evaluation of postoperative supracondylar periprosthetic femur fractures. The system demonstrates completeness, simplicity, and provides guidance in the choice of the appropriate treatment options. This system is based on fracture displacement and the status of the current prosthesis. Type I fractures are undisplaced and with a stable prosthesis without evidence of failure (loosening), or impending failure at the implant-bone interface. Type II fractures are those with stable implants but a displaced fracture pattern. Type III periprosthetic femoral fractures are those with a radiographically or clinically loose implant, regardless of fracture displacement. In the setting of intraoperative periprosthetic femur fractures, treatment options are primarily operative as there is little indication for nonoperative management upon identification of an intraoperative fracture.
Avoidance Understanding potential risk factors is critical to avoid potential intraoperative complications. Patient-related risk factors for periprosthetic femur fractures involve conditions that result in osteopenia. These include rheumatoid arthritis, neurologic disorders, advanced age, female gender, and those being treated with systemic corticosteroids.19,21–29
An understanding of femoral anatomy can minimize the risk of intraoperative fractures. Anatomic considerations regarding the femoral diaphysis include femoral canal geometry, compromised bone due to cortical attenuation or osteopenia, and the presence of local hardware. The femoral diaphysis has an anterior bow that risks cortical perforation or fracture during canal preparation or insertion of a femoral component with a diaphyseal-engaging stem. With a history of previous fractures, the canal geometry may also be altered. Osteopenic bone, particularly with attenuated cortices, amplifies the risk of diaphyseal fracture which should alert the surgeon to take extra precaution when working within the femoral canal. Hardware from previous procedures (cortical screws or an ipsilateral femoral stem from a hip arthroplasty) should be noted preoperatively in order for the surgeon to anticipate obstacles when using intramedullary instrumentation.
The anatomy of the femoral metaphysis must also be considered in revision TKA. In order to accommodate the intercondylar box of a revision femoral component, the box cut is often wider and deeper than that for the equivalent size in a primary cruciate-substituting component. Positioning of the box cutting guide too far medially or laterally may create a significant risk for development of a femoral condylar fracture.19 Even with precise preparation of the notch, there may be a significantly narrower bridge of bone between the corner of the box cut proximally and the metaphyseal flare, particularly medially (Fig. 58-1). This becomes even more critical in patients of small stature and females where the medial-lateral dimension of the distal femur is proportionately smaller and the relatively large width and depth of the box cut becomes a greater risk.
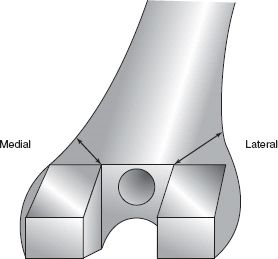
FIGURE 58-1. Narrow bridge of bone between the box cut and the medial metaphyseal flare.
Anterior notching of the femur has been documented in both clinical and biomechanical studies to cause compromise of distal femoral rotational strength, thus increasing the risk of periprosthetic fracture.19,21–28,30–32 Intraoperative anterior cortical notching is associated with 0% to 52% of periprosthetic femoral fractures.22,24,25,28,30–33 Lesh et al.28 observed that 30.5% of periprosthetic fractures reported in the literature were associated with anterior notching. Mathematical and biomechanical data also support these studies and have found that anterior notching of as little as 3 mm can decrease the mean torsional strength of the distal femur by 29% to 39%.28,34 Bending strength was less affected but still decreased 18% with full-thickness anterior notching.28 On the contrary, however, Ritter et al.31 in a review of 670 TKA cases observed 138 (20.5%) of the subjects reviewed exhibited an anterior notch ≥3 mm, yet only 2 of 670 (0.3%) developed a supracondylar femoral fracture, and only 1 of the 2 fractures were associated with an anterior femoral notch. This suggests that osseous remodeling over time may protect against fracture. Some believe the concern for fracture secondary to anterior notching is minimized after 6 months postoperatively due to bone remodeling.31 Avoidance of anterior notching, especially through the anterior-medial cortex at the time of the initial implantation, is advised to prevent excessive stresses occurring in the distal femur and the subsequent risk of future fracture.35
Risk of intraoperative fractures can be minimized through careful preoperative planning and thorough radiographic evaluation. The anterior bow of the femur is easily visualized on the lateral view and should be considered when templating for stemmed components. Cortical thickness, diaphyseal deformity, and previously implanted hardware which may obstruct intramedullary instrumentation should be noted. Radiographs should be scrutinized for the presence of osteolysis with the awareness that the severity of osteolysis is usually underappreciated on plain films. A CT scan is sometimes helpful preoperatively to assess the degree of bone loss if severe osteolysis is expected. Lugs or keels on the components should be identified to plan the appropriate approach for component removal.
Several stages during a revision TKA operation carry an elevated risk for intraoperative fracture. Component removal, intramedullary instrumentation, and trialing of components should heighten the awareness of the surgeon for potential fracture. Failed components can be carefully removed by using a small oscillating saw blade and flexible osteotomes in order to disengage the implant from native bone with minimal bone loss. During femoral preparation, misdirected starter drills used to initiate intramedullary instrumentation can lead to a cortical breach. Intramedullary reamers can be diverted from the intended trajectory if remnant cement or previous hardware is left in the canal. Trialing of components should be performed carefully particularly in the setting of osteolysis or osteopenic bone. Bone cuts should be checked to ensure the distal femur can adequately accommodate the components prior to impacting the trials in place. If difficulty is encountered during impaction of trial or final components, avoidance of increasing the impaction force is critical to minimize fracture risk. In these cases, consideration of obtaining an intraoperative radiograph is wise to assess component fit and position, particularly if a diaphyseal-engaging stem is being utilized.
Inadequate box preparation can potentially result in a femoral condylar fracture if the box cut is too shallow. Once trial components are impacted into place, the knee should be examined with considerable care when moving the knee from flexion to extension. A flexion-extension gap mismatch may result in an epicondylar avulsion fracture if the knee is brought into extension with a relatively tight extension gap, or brought into flexion with an excessively tight flexion gap. The risk is compounded when there is extensive osteolysis and the epicondyles are merely a thin cortical shell overlying an osteolytic void.
Implant factors can also play a role in intraoperative femur fractures. Although using stemmed components is often necessary to achieve optimal fixation, stems with dimensions that are not compatible with the host canal can potentially lead to diaphyseal fracture. Uncemented stems pose a greater risk for fracture than cemented stems since uncemented stems require tight diaphyseal purchase. Use of a cemented stem avoids the burden of a rigid uncemented stem applying hoop stresses to the cortices for fixation. Offset stems are sometimes required to accommodate canal geometry to allow more direct and central alignment of the stem relative to the diaphysis (Fig. 58-2). Press-fit “clothespin” or slotted stem designs allow more forgiveness when used in a highly bowed femur. Slotted stems should be assembled such that the plane of the slot is parallel to the axis of the bow. Bowed stems are also available for some systems for use with the femoral component and are particularly valuable if longer stems (≥150 mm) are required.

FIGURE 58-2. Offset tibial stem.
Management The goals of managing intraoperative fractures are to achieve anatomic reduction, rigid internal fixation, and early joint motion. Intraoperative fractures should be addressed upon identification. In order to ensure appropriate visualization of the reduction, an extensile exposure is usually required. Soft tissues surrounding the fracture, however, should be respected in order to maximize biologic healing. Excessive soft tissue stripping of the cortical surfaces in the vicinity of the fracture reduces local blood supply and can compromise fracture healing potential. Open reduction and internal fixation of intraoperative fractures often increases degree of difficulty secondary to working around the prosthesis or cement, and in many cases, trying to achieve fixation in osteopenic bone,36 but multiple treatment options are available.
Fixation options for intraoperative periprosthetic femur fractures include use of a condylar blade or screw plating system, distal femoral locking plates, or intramedullary fixation. Use of an intramedullary nail is an option for treatment of diaphyseal fractures above a TKA, however, in the revision setting, this is usually not possible given the closed box design and stemmed components.
Use of the condylar blade or screw plating systems has long been advocated for the treatment of supracondylar periprosthetic femoral fractures.22,37–39 With more current fixation devices available, its use should now be reserved for periprosthetic fractures that are displaced, are minimally comminuted, and have good bone stock with limited osteopenia.21 Problems cited with this method of fixation include unpredictable ability to achieve rigid distal fixation, especially in comminuted, osteopenic and very distal fractures, resulting in loss of fixation, alignment, and varus angulation.21,27,33,39,40 Figgie et al.40 reported a loss of fracture alignment in 80% of 10 severely osteopenic, comminuted fractures treated with a condylar plating system. Attempts to enhance fixation of these devices in patients with osteopenic bone and reduce the incidence of nonunion and malunion have included the additional use of polymethylmethacrylate,39 corticocancellous allograft,37 and retrograde placement of intramedullary fibular allograft38 to improve fixation along the length of the plating system. These adjunctive treatments typically improve fixation as evidenced in the results of Zehntner and Ganz who utilized adjunctive polymethylmethacrylate and condylar plating and reported a 100% success rate without malunion in six cases of supracondylar femoral fractures following TKA.38
Various types of plates are currently available for providing rigid fixation after reduction. Recent plate designs use locking screw technology to create fixed-angle screw fixation which provides an extremely rigid construct. Several studies21,23,27,30,41 report on the use of the femoral Less Invasive Stabilization System (Synthes; Paoli, PA) locking plate for periprosthetic fractures above total knee arthroplasties. Results revealed low requirement for bone grafting to achieve union, excellent distal femoral fixation, and no varus collapse or loss of alignment. These locking plates provide numerous advantages over standard condylar plate systems. Locking plates act essentially as an “internal,” external fixator.21,23,30,42 In most systems, strategically placed screws along the fixation plate have the option of being rigidly locked at a fixed angle into the plate providing multiple sites of screw stability that each acts in a manner similar to that of a fixed-angle blade or condylar screw. Many of these plates have the option of using standard unlocked screws or locking screws at the same screw hole level.27 This gives the potential benefit of using the anatomic plate to assist in fracture reduction with the standard screws and providing superior fixation with the locking screws.27 The use of multiple distal fixed-angle locking screws provides increased fixation and stability of the distal fragment.30 This is especially important in the short, osteopenic distal fracture fragment which is commonly seen in periprosthetic femoral fractures (Fig. 58-3). Locking of each screw to the plate prevents toggle of the screw at its interface with the plate and provides a rigid internal scaffolding and fixation for the reduced bony fragments.27,30,42 They do not require bicortical bone fixation to maintain stability of the fracture fragments. Unicortical lateral locking screws may be used in the regions of the femur occupied by an intramedullary stem or where the intercondylar box of the femoral component prevents bicortical screw fixation. In addition, many of these systems are designed to be tissue sparing in which the locking plate can be passed beneath a submuscular plane through limited skin incisions30,42 Once the distal fracture fragments have been aligned and distal locking screws appropriately placed, fixation into the diaphysis can be performed through indirect closed reduction and percutaneous techniques with or without the use of a guide (Fig. 58-4). Submuscular plate placement with percutaneous proximal screw fixation requires less soft tissue dissection and subsequent osseous devascularization. In addition, percutaneous submuscular plate placement has been associated with improved periosteal and intramedullary perfusion when compared to standard plating techniques.42 This potentially may decrease the incidence of infection and the need for primary bone grafting, improve union rates, and decrease postoperative stiffness allowing an earlier return to normal function.21,27,30,43,44 This is supported in clinical studies that have shown superior maintenance of reduction allowing early postoperative range of motion and early weight bearing (6 to 12 weeks) when compared to standard distal femoral plate or retrograde nailing systems.21,27,30,43,45,46 In reviews including 38 cases of periprosthetic femoral fractures treated with a locking femoral plate system, the authors observed excellent maintenance of distal fixation, no occurrence of postoperative varus collapse or infection, an average time to full weight bearing of 13 weeks, limited need for additional bone grafting (1 of 38; 2.6%), and a union rate of 97% (37 of 38).27,30 Potential disadvantages of use of interlocking plates include iatrogenic malalignment of the fracture fragments due to indirect reduction using percutaneous techniques27,30, poor submuscular plate placement,30 and proximal unicortical screw pullout if stresses are high.43,44

FIGURE 58-3. Four-month postoperative anteroposterior (A) and lateral (B) radiographs following treatment with a locking condylar plate.

FIGURE 58-4. Intraoperative photograph of insertion of a locking condylar plate with attached screw guide which facilitates submuscular plate placement and proximal percutaneous screw insertion.
Some recent plate designs have incorporated polyaxial locking screw technology which allows freedom of screw angulation while maintaining the benefits of a locking screw. This is particularly advantageous in the setting of achieving fixation around the prosthesis (lugs, intercondylar box, or existing stems) (Fig. 58-5). In these designs, screws can be inserted in a 30-degree arc around the central axis to allow more freedom of locking screw placement. Additionally, this allows the surgeon to have more options to gain fixation into optimal bone without allowing the device itself to determine the ultimate locking screw angles. Several plate designs can also accommodate cables, which is an extremely useful option in regions of the canal occupied by an intramedullary stem of the femoral component or an ipsilateral total hip arthroplasty.
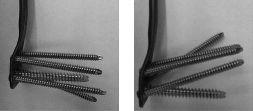
FIGURE 58-5. Photographs of a condylar locking plate in which the distal screws can be inserted in a 30-degree arc around the central axis to allow more freedom of locking screw placement.
With a distal femoral fracture, it may be possible to bypass the fracture with a longer diaphyseal-engaging stem.24,25,29,40,47,48
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








