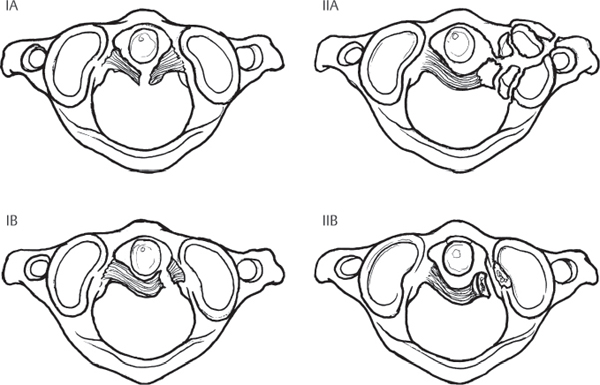
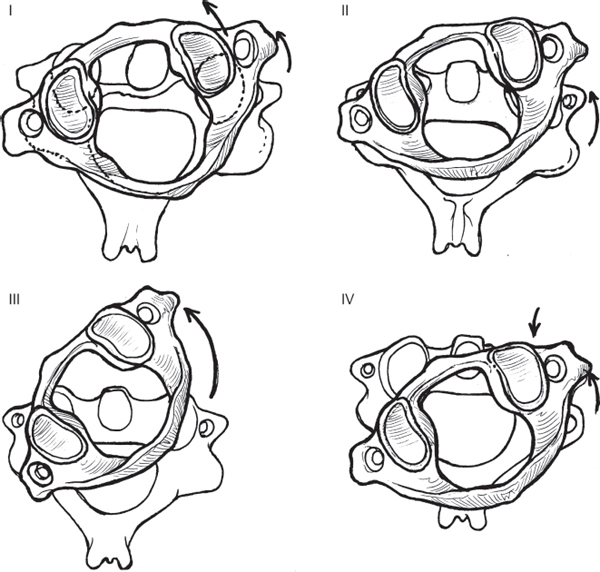
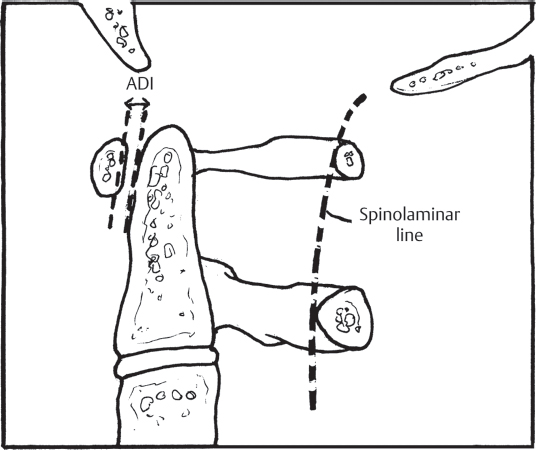
3 The atlanto-axial (AA) junction is one of the most mobile joints in the entire spine, accounting for ~ 50% of the head’s rotational ability about the torso. Motion at the AA junction occurs through the articulation of the atlas on the dens, with the C1 ring rotating around the fixed post of the C2 odontoid process. The stability of this articulation is ensured by several strong ligamentous structures: the transverse ligament, which spans the interval posterior to the odontoid and connects the lateral masses of C1; the apical ligament; and the alar ligaments, which stabilize both the occipitocervical (OC) and AA junctions. AA instability may result from injuries to the osseo-ligamentous structures, such as in conjunction with a C1 ring Jefferson fracture or odontoid fracture, or the ligaments alone can be disrupted. AA injuries exist on a continuum, from disruption of a single ligament to true AA instability, which represents the complete disruption of all ligamentous stabilizers of the articulation. Traumatic AA injuries are rare and are usually precipitated by significant forces applied across the articulation, as may occur from high-speed motor vehicle accidents or falls from a height. These injuries, although somewhat similar in terms of the structures involved, are different from the more common nontraumatic AA instability encountered in patients with rheumatoid arthritis, and treatment for these injuries cannot reliably be informed by studies describing management in the rheumatoid population. The two most commonly encountered injuries involving the AA junction are traumatic disruption of the transverse ligament and rotational instability. Based on their experience with 39 patients, Dickman and colleagues graded transverse ligament injuries in a four-part classification system (Fig. 3.1). The classification is largely descriptive in nature, based on the location of the ligamentous injury and the presence of associated fracture, but the system does provide a means of informing treatment. Rotational instability at the AA junction was classified by Fielding and Hawkins (Fig. 3.2). This classification consists of four grades and accounts for the amount of displacement of C1 on C2, the degree of lateral mass subluxation, and widening of the atlanto–dens interval (ADI). This grading scheme, derived from the authors’ experience with 17 patients, has not been validated. Yet it remains a descriptive classification, although its reliability, reproducibility, and ability to direct treatment are yet to be substantiated. Traumatic AA injuries usually occur as a result of significant high-impact trauma, such as motor vehicle accidents, falls from a height, or accidents in which a pedestrian is struck by a motor vehicle. Frontal-impact motor vehicle accidents have frequently been cited as precipitating trauma at the AA junction. All patients with an appropriate injury mechanism and complaints of substantial upper cervical or OC pain should be considered as potentially having an AA injury until proven otherwise. Those who present with a fixed torticollis should be suspected of having AA rotatory instability. Patients with a longstanding history of rheumatoid arthritis and children with Grisel’s syndrome (retropharyngeal infection) may be prone to developing AA injuries following minimal or no trauma. The similarity between these nontraumatic etiologies and traumatic AA instability remains unclear. Fig. 3.1 Classification of transverse ligament injuries described by Dickman et al. Type IA: mid-substance tear; Type IB: tear at the periosteal attachment; Type IIA: comminuted fracture of the lateral mass at the ligament insertion (which technically is not a ligament injury but results in ligament incompetence); Type IIB: small osseous avulsion of the ligament from C1. Fig. 3.2 The Fielding and Hawkins classification of traumatic rotatory AA instability. Type I is a pure, fixed rotation with no widening of the atlanto–dens interval (ADI); Type II is a rotation injury with an ADI less than 5 mm (transverse ligament alone disrupted) and one lateral mass joint intact; Type III is rotation with more than 5 mm of widening of the ADI and asymmetric lateral mass subluxation; Type IV consists of posterior subluxation and rotation. The rare Type IV manifestation presumably results from an extension mechanism. All patients with suspected, or confirmed, AA instability should undergo a complete neurological evaluation. Those who are alert, cooperative, and lack other distracting injuries may complain of pain at the occipitocervical (OC) junction or upper cervical spine and can have reproducible pain on palpation. A cervical collar should be placed, immobilizing the cervical spine until definitive imaging can be performed. Patients with vertical dislocation of the AA joint should be immobilized with sandbags placed on either side of the head. The application of a collar, or halo traction, can worsen injury in these situations. If rotatory AA instability has been confirmed by imaging, a halo ring can be placed as a temporary means of stabilization and gentle traction may be applied. In children, this intervention alone can be capable of reducing the rotatory subluxation. Plain-film radiographs and computed tomography (CT) imaging of the cervical spine, performed as part of the standard trauma workup, should be reviewed in those individuals suspected of having an injury at the AA junction. The plain-film lateral should be scrutinized for evidence of retropharyngeal soft-tissue swelling in the upper cervical region. Soft-tissue swelling greater than 6 mm anterior to the C2 body may be considered highly suggestive of injury. The ADI should also be examined on plain-film or sagittal CT reconstruction images (Fig. 3.3). Widening of this space more than 3 mm in an adult or 5 mm in a child indicates potential injury or rupture of the transverse ligament. The posterior cervical line, or spinolaminar line, should also be evaluated between C1 and C2 (Fig. 3.3). Normally, this line is a smooth concave arc running from the occiput through the posterior processes of C2. Any disruption in the contour of this curve should be considered indicative of an abnormal articular relationship between C1 and C2. Rotatory abnormalities between C1 and C2 are difficult to assess on plain radiographs, although some indication may be evident on the open-mouth odontoid view. A more robust examination of this articulation may be made using axial CT images, and the definitive diagnosis of rotational AA subluxation can occur with this study alone. If the patient’s medical condition and cognitive status will allow, dynamic axial CT examination can be performed with the patient attempting to rotate the head to the left and then to the right. The degree of rotational instability can best be assessed using this technique. MR imaging may be employed as an adjunct, to evaluate for the presence of edema within the AA joints, or to visualize the transverse ligament directly. Injuries at the AA junction may be amenable to conservative management or may necessitate surgical intervention, depending on the type of injury and degree of instability. Transverse ligament injuries that involve an avulsion fracture of the C1 ring and that are not associated with neurological injury can be treated with rigid immobilization in a cervicothoracic orthosis, or halo–thoracic vest. Purely ligamentous disruptions of the transverse ligament that result in instability should be treated with AA arthrodesis. Traditionally, such fusion constructs have consisted of transarticular screws with posterior sublaminar wiring and interposition bone grafting (Fig. 3.4). More recently, C1 lateral mass screws and C2 isthmus screws, along with C2 laminar screws and unilateral fixation techniques, have gained popularity. Studies have shown the C1 lateral mass, C2 isthmus screw constructs to be biomechanically comparable to transarticular screws. Unilateral instrumentation is biomechanically inferior to bilateral constructs, but clinical studies have shown no difference in outcome between these two fusion methods. Fig. 3.3 The ADI should be evaluated in all cases of suspected AA instability. The spinolaminar line, drawn by connecting points along the anterior portion of the posterior rings of each vertebra, should consist of a confluent arc.
Atlanto-Axial Instability
![]() Classification
Classification
![]() Workup
Workup
History
Physical Examination
Spinal Imaging
![]() Treatment
Treatment
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







