INTRODUCTION
Stress fractures are common injuries that occur in both competitive and recreational athletes. Although the majority of stress fractures are diagnosed in runners, any athlete participating in activities that involve repetitive loading is at risk, including swimmers, rowers, and baseball players.
1,
2,
3 The most common sites in runners are the tibia and metatarsals; however, the ribs, olecranon, and spine are recognized as frequent sites among rowers, baseball pitchers, and gymnasts, respectively.
1,
2,
4,
5 Stress fractures can be a diagnostic challenge due to the insidious onset of symptoms. They can mimic other common musculoskeletal injuries such as muscle strains and tendinopathies. Having a high index of clinical suspicion and an awareness of the risk factors and sport-specific demands can narrow the time to the correct diagnosis and treatment. Clinical knowledge of high-risk sites is important because management differs from that of low-risk sites and early treatment may prevent catastrophic outcomes.
FUNCTIONAL ANATOMY
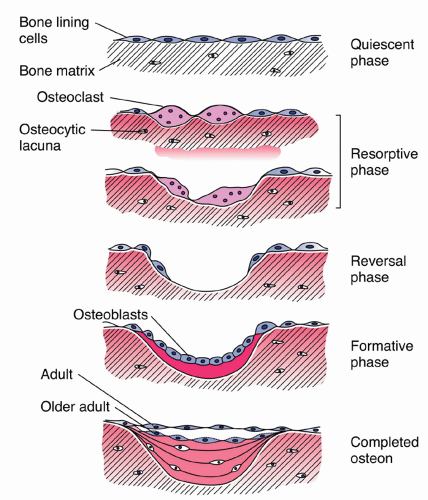
Proper bone health is dependent on the equilibrium of bone resorption by osteoclasts with bone rebuilding and remodeling by osteoblasts (
Fig. 22.1). Bone injury occurs on a continuum and begins when normal bone reparation and remodeling is disrupted. In this state, osteoclastic bone resorption outpaces osteoblastic bone building. In the earliest phases, cumulative microdamage occurs due to repetitive loading and may progress to microscopic crack initiation.
6,
7 If this imbalance between bone stress and reparation continues, crack propagation occurs, with the final stage being a nondisplaced or displaced fracture.
6Fatigue stress reaction or fracture is the most common type of bone stress injury in athletes and occurs when repetitive mechanical bone stress overloads the bone’s ability to repair and rebuild. This often occurs when there is insufficient rest between exercise bouts or rapid increases in training demands. The majority of fatigue fractures occur in cortical (compact) bone, which is found at the diaphysis of long bones and the outer layer of short bones such as the tarsals and vertebral bodies.
3,
6A second type of bone stress injury called an insufficiency reaction or fracture occurs when normal strains are placed on histologically abnormal bone as seen in osteopenia and osteoporosis. Athletes in a negative energy balance and hypoestrogenic state associated with the female athlete triad, osteoporosis, amenorrhea, and disordered eating, are at risk for this type of bone injury.
3,
6 Among female distance runners, 10% had osteoporosis, while 50% were osteopenic.
8 A negative energy balance with associated amenorrhea places an athlete at risk for low bone density, particularly cancellous bone.
8 Cancellous stress fractures in female athletes have been associated with osteopenia.
9 Cancellous bone is found at the metaphysis and epiphysis of long bones and in the interior of short bones.
Stress fractures are grouped into low-risk and high-risk sites. Low-risk sites are more likely to heal through conservative management, whereas high-risk sites tend to have delayed union or nonunion, progression to complete fracture, and recurrence and often require operative management. Common low-risk sites are ribs, ulna shaft, femoral shaft, posteromedial tibia, and the first four metatarsals.
10 Low-risk sites are loaded with compressive forces. High-risk sites include the femoral neck, patella, anterior tibial diaphysis, medial malleolus, talus, navicular, first metatarsal sesamoids, and the proximal fifth metatarsal.
10 High-risk sites tend to be loaded with tensile forces, increasing the risk of adverse outcomes (
Table 22.1).
EPIDEMIOLOGY
The incidence and anatomic location of stress injuries vary not only with each sport but also with regional and national sporting trends.
1,
5 In track and field athletes, the incidence is 8.7% to 21.1% in males and females combined, although one study reported an incidence of greater than 30% in collegiate female track and field athletes alone.
1,
8,
11 The majority of studies cite the lower extremities as the most frequently affected anatomic region, with the tibia, fibula, metatarsals, and tarsals reported as the most common sites, with bilateral stress fractures occurring in 16.6% of cases.
1,
2,
8 More recently, the tibia and ribs were reported as the most common sites when greater representation of overhead
throwing and rowing athletes was included than in previous studies.
5Among track and field athletes, distance runners were more likely to sustain stress fractures of the tibia, femur, fibula, and pelvis. Jumpers, sprinters, hurdlers, and those participating in multiple events had more foot fractures. Jumping and sprinting events were associated with navicular stress fractures.
3 Upper-extremity stress fractures occur in overhead throwing and racquet sports. Rib stress fractures have been associated with overhead throwing athletes and rowers and ulnar stress fractures with baseball pitchers.
5 Pars interarticularis stress fractures of the spine (spondylolysis) comprise 45% of all stress fractures in female gymnasts.
1Bone health in athletes is influenced by multiple factors, but the lack of well-designed, large prospective studies has resulted in a paucity of epidemiologic data regarding risk factors for stress fractures.
1 Intrinsic factors include nutritional status, gender, hormonal status, fitness levels, and biomechanical factors.
6,
12 Extrinsic factors include training errors associated with changes in intensity, frequency, and duration of activities.
2,
6 The effect of oral contraceptives on bone mineral density is unclear.
6,
8,
13 Oral contraceptive pills normalize menses in athletes with hypothalamic amenorrhea through estrogen replacement, but may mask underlying nutritional insufficiencies.
8Limited data identify disordered eating and menstrual dysfunction as significant risk factors for stress fractures among female athletes.
1 Amenorrheic and oligomenorrheic girls had an incidence of 15% versus 4% among eumenorrheic girls.
1 Osteopenia and amenorrhea in female athletes have been associated with cancellous stress fractures.
8,
9 Limited comparative data suggest that there is no difference in the incidence of stress fractures between female and male athletes. However, adjustment of training hours for stress fracture rates has been suggested as a more definitive method to demonstrate that women are at higher risk.
1 With regard to age and race, there are no consistent or significant findings in the literature among athletes.
1 Hard training surfaces have not been associated with an increased risk for stress fractures.
8 Training errors were associated with 22.4% of all stress fractures in one study.
2
NARROWING THE DIFFERENTIAL DIAGNOSIS
History
The earliest symptom of bone stress injury is insidious onset of lower-extremity pain during weight-bearing or sport-specific activities, which is relieved with rest. If the condition goes unrecognized and the athlete ignores the pain without activity modification, the pain may begin earlier in each exercise session and with greater severity. The pain may transition to a sharp, severe localized pain that occurs with all weight-bearing or inciting activities, with progression to resting pain.
3The patient will usually deny any specific trauma or injury prior to the onset of pain. An exception may be the tarsal bones, where a history of trauma was found to be associated with this type of stress fracture.
2 A specific episode of direct trauma or injury to a joint associated with torsional or hyperextension forces followed by swelling or joint instability should be investigated for ligamentous or cartilaginous pathology. Severe localized pain with fever as an initial
symptom in the absence of trauma may be indicative of an acute infectious or inflammatory process. Night sweats and weight loss should raise concern for malignancy.
Activity and nutrition patterns often provide significant clues in the diagnosis of bone stress injuries. Any alteration in the training routine can place both experienced and novice athletes at risk for stress fractures. Competitive athletes may reveal a change in the type, intensity, or duration of their training. Recreational athletes may report beginning a new activity or embarking on an ambitious training program. Nutrition and training patterns should be assessed in all male and female athletes with a suspected eating disorder. A thorough menstrual history should be obtained in females since amenorrhea is a risk factor for stress fractures.
8 Even subtle menstrual irregularities may put the athlete at risk for poor bone health.
14 A direct correlation exists between the number of stress fractures and the length of amenorrhea.
8The underlying pathophysiology of menstrual dysfunction in female athletes relates to an energy imbalance that causes hypothalamic dysfunction.
8,
13 A state of undernutrition leads to the loss of pulsatile hypothalamic hormone release.
8,
13 This may occur when the athlete fails to meet his or her caloric needs either intentionally through excessive exercise and restrictive eating or through a combination of both. It may also occur unknowingly when minor alterations in a training program result in higher energy demands.
13Stress fractures often mimic other conditions. Thorough history taking and knowledge of particular pain patterns may help to narrow the differential (
Table 22.2).
Evidence-based Physical Examination
Observation
Varus alignment (forefoot 72.6%, subtalar 71.9%, genu 29%, and tibial 18.9%) has been identified as a frequent finding among athletes with stress fractures.
2 No association was found between the severity of varus alignment and the stress fracture site.
2 Foot overpronation was associated with tarsal, fibular, and tibial stress fractures. Rigid pes cavus was observed most often in metatarsal and femoral stress fractures.
2
Palpation
Localized bony tenderness is a common finding.
2,
20 Palpable deformities and swelling may occur at the fracture site.
20 Swelling was found most commonly in the metatarsal and tarsal bones (
Table 22.3).
2
Range of Motion (ROM)
ROM is usually normal except for limitations in lumbar spine extension and hamstring flexibility that may occur in pars interarticularis defects.
16 Strength testing is usually normal.
12
Special Tests
Hop Test
This test is used to assist in the clinical diagnosis of lower-extremity stress fractures, especially of the femoral neck and tibia. The test is positive when the patient is single-leg hopping and experiences pain in the area of concern for a stress fracture. A positive hop test has been associated with femoral stress fractures.
2,
3,
14
Fulcrum Test
This test is used to assist in the clinical diagnosis of femoral shaft stress fractures. The athlete is seated on the edge of the examination table. The examiner’s arm acts as a fulcrum under the patient’s thigh and is moved from the distal to
proximal thigh while pressure is applied to the dorsum of the knee with the other hand. The test is positive if the patient experiences sharp pain localized to an area on the thigh that is being compressed by the examiner’s arm that is an area of concern for a stress fracture.
22
Tuning Fork Test
This test is used to assist in the clinical diagnosis of tibial stress fractures. A 128-Hz tuning fork is applied to the anterior surface of the tibia. The test is considered positive if the patient reports a marked exacerbation or reproduction of shin pain in a focal area of the tibia.
23
Diagnostic Testing
The clinical presentation of bone injuries frequently mimics other musculoskeletal problems; therefore, laboratory testing and imaging studies can expedite the diagnostic process. Imaging studies vary in their specificity and sensitivity and therefore utility in making a diagnosis, grading the injury and guiding treatment, and return-to-play decisions. Common imaging studies include plain radiographs, magnetic resonance imaging (MRI), computed tomography (CT), and bone scan. Laboratory testing is not required to diagnose a stress fracture, but it can be valuable in the evaluation of multiple stress fractures and insufficiency fractures and in suspected cases of spondyloarthropathy or an eating disorder.
Laboratory Studies
Laboratory studies are not necessary for the diagnosis of stress fractures but may be useful to determine underlying causes and rule out other conditions (
Table 22.4).
Imaging
Radiographs
MRI
MRI has emerged as the leading diagnostic modality for stress fractures, because it is highly specific in determining the site and grade of the injury and, as a result, treatment options.
3,
4,
17,
24