Athlete with Acute Wrist and Hand Injuries
Michelle Mariani
INTRODUCTION
Hand and wrist injuries are common in athletes, making up between 3% and 9% of all athletic injuries. Athletic injuries to the hand and wrist can range from simple sprains to severe fractures. Many injuries of the hand and wrist are obvious, but subtle injuries can be missed and may require a high index of suspicion with a systematic examination and diagnostic imaging. Often injuries to the hand and wrist may be dismissed as trivial; however, delay in diagnosis and treatment may lead to significant and possible permanent disability. Overtreatment or inappropriate treatment can be just as problematic. Swanson appropriately said, “Hand fractures can be complicated by deformity from no treatment, stiffness from over-treatment, and both deformity and stiffness from poor treatment.”1 In this chapter, we will discuss the diagnosis, treatment, and rehabilitation of common hand injuries to the athlete.
FUNCTIONAL ANATOMY
A basic understanding of the complex anatomy of the finger, hand, and wrist is necessary to properly diagnose and treat acute injuries. There are 27 bones that act dynamically to allow oppositional grip: eight carpal bones, five metacarpals, and fourteen phalangeal bones. In general, the radial nerve accounts for wrist and finger extension, the ulnar nerve provides finger flexion on the ulnar side and power grip, and the median nerve provides thumb opposition and circumduction to allow for fine control. Vascularity to the hand is provided by the radial and ulnar arteries, which join together in the palm to make up the deep and superficial palmar arches. Each digit has two neurovascular bundles, which travel volarly on both the radial and ulnar aspects of the digit.
Bony anatomy of the hand includes the five metacarpals, with first, fourth, and fifth metacarpals having increased mobility at their corresponding carpometacarpal (CMC) joints. In contrast, the second and third metacarpals are held rigid at the CMC joint by stout ligaments and congruent articulation with the trapezoid and capitate. The transverse metacarpal ligaments interconnect the second through the fifth metacarpals adding to their internal support. The thumb metacarpal is positioned on the trapezium in an abducted and pronated position to allow for its prehensile function.
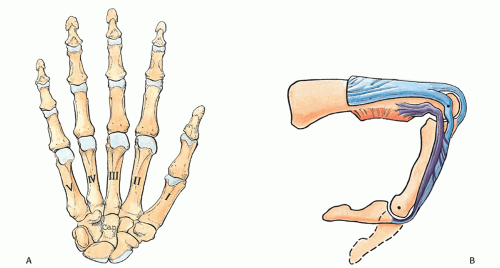
Each finger is an individual skeletal unit made up of a proximal, middle, and distal phalanx (Fig. 15.1A). The proximal and middle phalanges can be divided into the base, shaft, neck, and head, whereas the distal phalanx has a base, shaft, and tuft. There are three ginglymus (hinged) joints in each finger: distal interphalangeal (DIP), proximal interphalangeal (PIP), and metacarpophalangeal (MCP). The interphalangeal (IP) joints in the fingers are bicondylar, providing a great arc of motion as well as bony stability for lateral and rotatory forces. The collateral ligaments, volar plate, and extensor mechanism offer additional stability to the joint, and injury to these structures may compromise function significantly. The thumb CMC joint is unique with its reciprocally biconcave saddle joint allowing for opposition with the other digits.2 The thumb is made up of the first metacarpal and only two phalanges with a single IP joint.
The most complex anatomy of the hand includes the extensor mechanism of the fingers. The extensor digitorum communis (EDC) splits into four separate tendons, one to each finger. As the extensor tendon passes over the MCP joint, there is some adhesion to the joint capsule, but no formal insertion. The tendon is anchored over the MCP joint by the sagittal bands that arise from the volar plate. In addition to keeping the extensor tendon centralized over the MCP joint, sagittal bands also function to extend the proximal phalanx. At the MCP joint, the extensor tendon splits into three slips. The middle slip, which connects to the proximal phalanx by sagittal bands, inserts on the base of the middle phalanx. The two lateral slips unite more distally on the base of the distal phalanx after receiving contributions from the interossei on both sides and the lumbrical on the radial side (Fig. 15.1B). On the radial side of each digit, the lumbrical unites with the lateral slip to form the lateral band. The interossei also insert into the lateral slips to form the lateral bands in addition to the base of the proximal phalanx and joint capsule.
The flexor tendons on the volar side of the finger include the flexor digitorum superficialis (FDS) and the flexor
digitorum profundus (FDP). The FDS tendon travels volar to the FDP and splits to form two slips that attach to the base of the middle phalanx and function to flex the PIP joint. The FDP tendon is located dorsal to the FDS and inserts into the base of the distal phalanx and flexes the DIP joint.
digitorum profundus (FDP). The FDS tendon travels volar to the FDP and splits to form two slips that attach to the base of the middle phalanx and function to flex the PIP joint. The FDP tendon is located dorsal to the FDS and inserts into the base of the distal phalanx and flexes the DIP joint.
The anatomy of the wrist comprises one of the most complex joints in the body. The eight wrist carpal bones articulate with the radius and ulna and allow for a large arc of motion in three degrees of freedom. The proximal row of carpal bones includes the scaphoid, lunate, triquetrum, and pisiform, which are closely approximated to the distal radius. The triangular fibrocartilage complex, an articular disk located between the proximal row of carpals and the ulna, completes the concave surface on which the carpals move. The distal row of carpal bones includes the hamate, capitate, trapezium, and trapezoid, which articulate with the metacarpals. The scaphoid is the common link between the proximal and the distal row of carpals.
EPIDEMIOLOGY
Injuries to the hand and wrist are common in athletes of all levels. The two main types of injuries suffered by athletes include soft-tissue injury (tendon and ligament) or bony injury (fracture and/or dislocation). Thumb injuries should be considered a discrete group of injuries compared with the other digits as the anatomy and function differ significantly.
The hand is usually out in front of the athlete and used to catch a ball in motion, brace any falls, and block opponents. The middle finger is a commonly injured finger because it extends most distally, allowing it to be vulnerable to jamming, catching, and torsion. Thumb injuries are more common in falls to the side or reaching behind to brace a fall, such as during skiing. The small finger can also easily be injured as it gets caught on a jersey. An axial load to a closed fist or a misdirected punch may cause a metacarpal fracture or CMC injury. Any fall on an outstretched hand can cause a hyperextension injury and lead to fracture or ligamentous injury in the wrist.
Injuries to flexor and extensor tendons can occur during athletics, but injuries to the extensor mechanism are more common because they are weaker when compared to the flexors. The common injuries of the extensor mechanism include the mallet finger, acute boutonniere, and sagittal band injuries. The main injury to the flexor tendon suffered during sporting events is an FDP avulsion injury, also known as jersey finger. Whereas most of the extensor injuries seen are easily treated with splinting and observation, all flexor tendon injuries should be referred to a hand surgeon urgently for surgical fixation.
Extensor tendon injuries such as mallet finger and acute boutonniere injuries are common injuries in ball sports such as basketball, when the athlete’s fully extended finger is struck by the ball. In a mallet finger, the result is a stretching or disruption of the terminal tendon, which is responsible for active extension of the DIP joint. An acute
boutonniere injury ranges from a sprain to complete disruption of the central slip that can result from a volar PIP dislocation. An avulsion fracture is possible with both of these injuries, so x-rays need to be done to evaluate for this variant of injury.
boutonniere injury ranges from a sprain to complete disruption of the central slip that can result from a volar PIP dislocation. An avulsion fracture is possible with both of these injuries, so x-rays need to be done to evaluate for this variant of injury.
Injury to the sagittal bands can result in pain and extensor tendon subluxation during finger flexion. These injuries may occur from blunt trauma, forced flexion of the MCP joint, or sometimes even minor insults. These injuries usually involve a sagittal hood tear of the radial side of the long finger.
An FDP avulsion/rupture results from a forceful hyperextension of the DIP joint while the FDP is contracting. A classic example is catching the middle finger on a competitor’s jersey. The tendon may rupture from its insertion or avulse a small bone fragment from the distal phalanx. The tendon may retract into the finger or palm.
Fractures of the metacarpals and phalanges are the most common fractures of the upper extremity.3 The thumb and small finger are the most frequently fractured.4 The majority of these fractures can be managed nonoperatively, but unstable fractures need to be recognized and referred to a hand surgeon for operative management. Regardless of treatment, the goal is to restore hand function and prevent stiffness or deformity.
The most commonly dislocated joint in the body is the PIP joint of the finger. Injury to the PIP joint can range from a jammed finger to a complex irreducible fracture dislocation. The severity of these injuries is often underestimated, and improper treatment may cause long-term disability. The direction of dislocation is usually dorsal, but volar and lateral dislocations may occur.
The DIP and MCP joints are less commonly dislocated. Dorsal dislocations are the more common variant of these IP dislocations. DIP dislocations are usually related to a crushing-type injury and are more prone to open injuries because of the tissue attachments distally. It is important to realize that MCP joint dislocations can be either simple subluxation injuries that can easily be reduced or a complex complete dislocation that usually requires surgery to relocate.
All IP dislocations are associated with some ligamentous injury. The most common soft-tissue injury with joint dislocations is avulsion of the volar plate. Collateral ligament and tendon avulsions are also possible at the time of injury. Intra-articular fractures can occur and range from small, insignificant avulsions to larger triangular or comminuted fractures that make up a significant portion of the joint.
Injuries to the thumb MCP joint are quite common. The most common injury to the MCP joint is an ulnar collateral ligament (UCL) disruption. This injury occurs when an athlete falls on an outstretched hand with the thumb abducted, as might occur when a skier falls while holding a pole.
The wrist is a complex anatomic structure made up of eight carpal bones, the distal radius, distal ulna, and multiple tendons and ligaments. It is beyond the scope of this chapter to discuss every injury that can occur to the intricate wrist, but the more common athletic injuries should be recognized. Appropriate treatment of wrist injuries can prevent future disability. Scaphoid fractures are by far the most common carpal fracture. Other acute sporting injuries to the wrist include hamate fractures and scapholunate ligament tears.
NARROWING THE DIFFERENTIAL DIAGNOSIS
History
A good history and detail of the mechanism of injury may help you focus on a diagnosis prior to the examination and help guide your decision-making. Some injuries are more prevalent in specific sports, such as jersey finger in rugby and football or hook of the hamate fractures in golf and baseball. Also a history of refractory pain in an initial negative assessment should prompt further examination and diagnostic imaging as a more subtle diagnosis may be present.
Evidence-based Physical Examination
Start with the basics of inspection, palpation, and a thorough neurovascular examination. Inspect for swelling, deformity, ecchymosis, and possible open injuries. Palpate for point tenderness, stepoffs, and crepitation. The patient should be able to actively extend all of their fingers and thumb. An inability to actively extend a finger should prompt further examination. Examination of finger flexion should include isolating the FDP and the FDS function. The FDP can be tested by holding the PIP straight and asking the patient to flex their DIP joint. Evaluation of rotational deformity may be picked up by observing that the plane of the fingernails lines up. If a rotational deformity is present, there will be finger crossover with flexion. Varus and valgus testing will help determine joint laxity. MCP joints should be stressed with the joint flexed to 90 degrees.
Diagnostic Testing
Imaging
Routine radiographs of the hand or wrist should begin with PA, lateral, and oblique views. If you are suspicious of a specific injury or need better visualization of a fracture, other views should be considered. Individual fingers should have a true lateral of the injured finger. A true AP of the thumb (Roberts view) is obtained by having the patient hyperpronate the hand and rest the dorsum of the thumb on the x-ray cassette. A true lateral of the basal joint is obtained by pronating the hand 20 degrees with the thumb flat on the x-ray cassette and the x-ray tube angled 10 degrees in a distal-to-proximal direction. A 30-degree pronated lateral will help visualize the second and third metacarpals, and a 30-degree supinated lateral will help visualize the fourth and fifth
metacarpals. Suspicion of an easily missed CMC fracture dislocation should prompt careful inspection of these oblique views.
metacarpals. Suspicion of an easily missed CMC fracture dislocation should prompt careful inspection of these oblique views.
MRI may be utilized to better visualize soft-tissue injuries, while CT may be required to assess complex fractures and bony anatomy not visualized on plain radiographs. Musculoskeletal ultrasound is gaining popularity due to its excellent soft-tissue visualization of superficial structures along with the dynamic capabilities. Its relatively low cost and lack of ionizing radiation also make it a good option.
APPROACH TO THE ATHLETE WITH A TENDON INJURY
HISTORY AND PHYSICAL EXAMINATION
A mallet finger and acute boutonniere injuries are both caused by forced flexion of extended DIP and PIP joints, respectively. The history of a mallet injury often involves a ball striking the tip of the finger. The athlete may have only minimal pain and may even continue playing. The patient usually presents after the game or in the office with inability to actively extend the injured finger. Examination will confirm this flexion deformity, but passive extension should be possible.
Central slip injuries are usually from a jamming-type injury to the finger, and the patient will complain of pain at the PIP joint. The examination may demonstrate an acute boutonniere deformity, making the diagnosis easy, but this deformity usually takes several weeks of no treatment to develop. The patient should be tested for active PIP extension. Weak active PIP extension, with intact passive extension, is indicative of an acute central slip injury.
Patients with sagittal band injuries at the MP joint can present with a history of a direct blow or a more mundane activity such as flicking their finger. Boxers can suffer from this injury after repetitive trauma. Symptoms vary from pain and loss of motion at the MP joint to actual extensor tendon snapping during finger flexion. Ulnar deviation of the finger may also be apparent in severe cases. In order of frequency, these injuries are most common in the long, small, index, and ring fingers.
FDP avulsion injuries are an injury not to be missed, as surgical intervention is needed promptly to restore full finger function. The history usually involves catching or jamming the tip of the finger on an opponent or a ball. The DIP joint will be swollen and painful, and a painful fullness may also be appreciated more proximally along the volar aspect of the finger or in the palm. To test the integrity of the FDP, ask the patient to actively flex the DIP joint while immobilizing the PIP joint. Inability to do so should prompt immediate referral to a hand surgeon for surgical repair of the FDP tendon.
DIAGNOSTIC TESTING
Imaging
AP and lateral x-rays
Evaluate for any avulsion fractures of the phalanges
Evaluate lateral x-ray for volar subluxation joints (bony mallet or central slip disruption)
Large fragment may be an indication for surgery (FDP avulsion)
Identify the level of retraction for operative planning.
TREATMENT
Nonoperative
Most are able to be treated nonoperatively
Six to eight weeks of continuous extension splinting
Followed by 2 weeks of splinting at night and sporting activities5
Lightly padded aluminum splint, stack splint, or ring splint
Applied to dorsal aspect of the DIP joint
Avoid immobilizing the PIP joint
Treatment can be initiated up to 6 months after the injury
Success rate with splinting approximately 80%6
Avoid pressure breakdown of skin with splinting
Acute central slip injuries with a supple joint
PIP joint splinting for 6 weeks
Followed by night splinting for another 6 weeks
DIP and MP joints are left free and DIP flexion encouraged
Older patients immobilized for a shorter time to prevent PIP joint stiffness
Sagittal band injuries not causing extensor tendon subluxation
Treated with buddy taping.
Symptomatic subluxing extensor tendon and is diagnosed less than 3 weeks from injury
Continued for 6 weeks
Block MP flexion, and allow for PIP motion.
Operative
Surgical indications include
Open injuries
A large avulsion fracture with a volar subluxation of the distal phalanx
Closed injuries in patients who may not be able to work with a splint (i.e., surgeon)
Surgical treatment recommended for
Closed boutonniere injuries with a large avulsion fracture9
Repair of the sagittal band in a patient with a symptomatic subluxing extensor tendon
Diagnosed more than 3 weeks from injury
Or if they failed splint treatment
All open injuries to tendons and flexor tendon injuries
FDP tendon avulsion, which is usually repaired primarily
Protected immobilization of the repair for 6 to 8 weeks
Prognosis/Return to Play
Prognosis is excellent in a closed mallet or boutonniere injury
Diligent in continual splinting for 6 to 8 weeks
If the finger falls into flexion, must start from the beginning
Return to play varies with the severity
Most can return with an appropriate splint
Sagittal band injuries have a good prognosis
If no tendon subluxation, may return to play with buddy taping
Surgery may delay return to play until full range of motion and grip strength returns
Prognosis of flexor tendon injuries prognosis depends on early recognition and treatment
FDP avulsion injuries require surgical intervention
May restrict activities for 3 to 4 months
Complications/Indications for Referral
Complications of extensor tendon injuries are not common, but can occur with insufficient treatment or noncompliance. An extensor lag deformity may persist and secondary deformities may develop. A persistent mallet injury will develop into a swan-neck deformity, and the central slip injury will fall into a boutonniere deformity. Complications of sagittal band injuries are rare, but operatively repaired sagittal band injuries may become stiff.
There are specific findings in tendon injuries that should prompt referral to a hand surgeon. Any open tendon injury, unstable joint, lack of passive extension, or avulsion fracture involving greater than 30% are indications for referral and possible surgical intervention. It is also imperative to diagnose the FDP avulsion injury early and refer promptly. A delay of 7 days will make repair difficult and may compromise the outcome of the finger function.
APPROACH TO THE ATHLETE WITH A HAND FRACTURE
HISTORY AND PHYSICAL EXAMINATION
Phalangeal and metacarpal fractures can range from nondisplaced stable fractures to displaced, comminuted fractures. Often the type of fracture is directly related to the mechanism of injury. A direct blow usually causes a transverse fracture. Rotational forces, such as those that occur when an athlete grabs an opponent’s jersey, cause spiral fractures. Axial loading to the finger usually causes intra-articular fractures and may be associated with joint dislocation as previously discussed. An axial load on a closed fist is the common mechanism of a fourth or fifth metacarpal neck fracture, commonly referred to as a “boxer’s fracture.”
Physical examination should include a routine neurovascular examination, range of motion of each joint, inspection of the skin for potential open fractures, and evaluation for any deformity. Every phalangeal and metacarpal fracture should be evaluated specifically for rotational deformity. This can be accomplished by asking the patient to flex all digits and evaluate for any rotation or overlap of the injured finger in comparison with the other digits. All fingers should point toward the scaphoid.
DIAGNOSTIC TESTING
Imaging
Radiographs – PA, lateral, and oblique views
Identify fractures and define the severity of the injury
Semipronated view will allow optimal visualization of the index metacarpal
Semisupinated view will allow optimal visualization of the ring and small finger metacarpal
Individual finger radiographs to assess for phalangeal fractures
TREATMENT
Nonoperative
Most phalangeal and metacarpal fractures can be managed nonoperatively
Distal phalanx fractures are divided into tuft and transverse fractures
Tuft fractures
Associated with an open nail bed injury or subungual hematoma
If a subungual hematoma that involves greater than 50% of the nail bed is decompressed
Dorsal aluminum splint
Rarely indicated for more than 3 weeks
Should not include the PIP joint3
Nondisplaced and stable middle and proximal phalangeal fractures
Buddy taping or splinting
Can be reduced to convert to a stable fracture
Wrist-based splint, MP joints flexed to 70 degrees and the digits in extension
Follow up radiographs weekly until bony union is evident
Spiral and oblique fractures have a tendency to redisplace and shorten and often require internal fixation
Metacarpal fractures
Ring and small fingers can tolerate up to 40 degrees of dorsal angulation
Index and middle fingers can tolerate only 10 to 15 degrees of dorsal angulation
Reduction by flexing the MP joint to 90 degrees and using the proximal phalanx to exert an upward pressure on the flexed metacarpal head10
Held in place by plaster or fiberglass
X-ray is done weekly to confirm satisfactory reduction
Nondisplaced metacarpal neck fractures can be treated with simple buddy taping
A functional brace is an option in treatment of stable metacarpal fractures
Spiral or oblique fractures are more likely to cause a malrotation deformity and need to be corrected to restore normal hand function. If the rotation is not corrected after reduction, surgical intervention may be necessary.
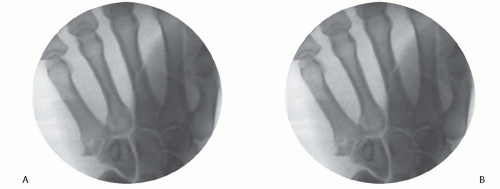 FIG. 15.2. A: 25-year-old male professional baseball player who sustained a closed carpometacarpal (CMC) fracture dislocation of the left hand after a diving catch. B: Note the displaced fracture of the small finger metacarpal base. Reprinted with permission from Strickland JW, Graham TJ. Master Techniques in Orthopeadic Surgery: The Hand. 2nd ed. Philadelphia: Lippincott Williams & Wilkins; 2005.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|